Atypical electrocardiographic manifestations of ischemia: a case of dynamic Wellens patterns
Alex Tsz Lai Ngan RN, Cynthia Yeung, Lorraine Chiang, Tong LIU, Gary Tse,Ka Hou Christien Li
1Department of Medicine and Therapeutics, Faculty of Medicine, Chinese University of Hong Kong, Hong Kong, China
2Li Ka Shing Institute of Health Sciences, Faculty of Medicine, Chinese University of Hong Kong, Hong Kong, China
3Department of Medicine, Queen’s University, Kingston, Ontario, Canada
4Li Ka Shing Faculty of Medicine, University of Hong Kong, Hong Kong, China
5Tianjin Key Laboratory of Ionic-Molecular Function of Cardiovascular Disease, Department of Cardiology, Tianjin Institute of Cardiology, the Second Hospital of Tianjin Medical University, Tianjin, China
6Faculty of Medicine, Newcastle University, Newcastle, UK
Keywords: Dynamic pattern; Ischemia; Wellens
A 55-year-old male with hypertension, hyperlipidemia,impaired fasting glucose, obesity, gout, and osteoarthritis,statin-induced myopathy, but no known cardiac disease, presented with a one day history of intermittent exertional chest discomfort without radiation. Symptoms included sweating,dyspnea, dizziness, and upper limb numbness. The pain settled soon after admission. The patient was diagnosed with unstable angina. On admission, high-sensitive Troponin I(hsTnI) level was 161 ng/L. The initial electrocardiogram(ECG) captured after resolution of chest discomfort revealed sinus rhythm with biphasic T-waves in V1-V3and T-wave inversion in aVL (Figure 1A), consistent with a type 2 Wellens pattern. Eleven hours after admission, hsTnI increased to 431 ng/L and a repeated ECG demonstrated biphasic T-wave in V3and new onset T-wave inversions in V4-V6(Figure 1B). Seven hours later, hsTnI remained at 414 ng/L and a third ECG showed deep T-wave inversions in V2and V3(Figure 2) consistent with a type 1 Wellens pattern.The patient denied chest pain or discomfort during the course of admission. His initial treatment included aspirin(160 mg) in the ambulance and in the accident and emergency department. Subsequently, clopidogrel (300 mg) and enoxaparin (110 mg) were administered. Cardiac catheterization was performed two weeks later with angiography demonstrating critical stenosis of left anterior descending artery (80% proximal stenosis, 70% distal stenosis). Two drug-eluding stents were deployed and TIMI grade 3 flow was achieved. A final ECG demonstrated normalization of the ECG findings (Figure 3).
First described in 1982 by Hein J.J. Wellen and colleagues, Wellens pattern represents a temporal relationship between an initial ischemic event in the context of coronary artery disease and the point at which the ECG is captured.[1]Wellens pattern is not a rare phenomenon, occurring in 14%-18% of patients admitted to hospital for unstable angina.[2]The diagnostic criteria of Wellens pattern are summarized in Table 1. The classical ECG finding (type 1 Wellens pattern) accounting for 75% cases is a minimally elevated or isoelectric ST segment with deeply inverted T-waves in leads V2and V3.[3]By contrast, a type 2 pattern is observed in around 25% of cases and is characterized by biphasic T-waves (with initial positivity and terminal negativity) in leads V2and V3.[3]Despite symptomatic relief from medical management, the unresolved high-grade stenotic lesion often degenerates rapidly into an acute anterior wall myocardial infarction (MI), left ventricular dysfunction,arrhythmias, or death.[4-6]Therefore, the definitive treatment for patients presenting with Wellens pattern is cardiac catheterization.
In our case, the ECG initially showed a type 2 pattern changing to a type 1 pattern. Previously, it has been noted that Wellens pattern and de Winter’s T-waves may represent the same disease spectrum reflecting high-risk proximal left anterior descending artery narrowing and occlusion,respectively.[7]T-wave inversion may occur after reperfusion of the myocardium. Wellens pattern makes for a chal-
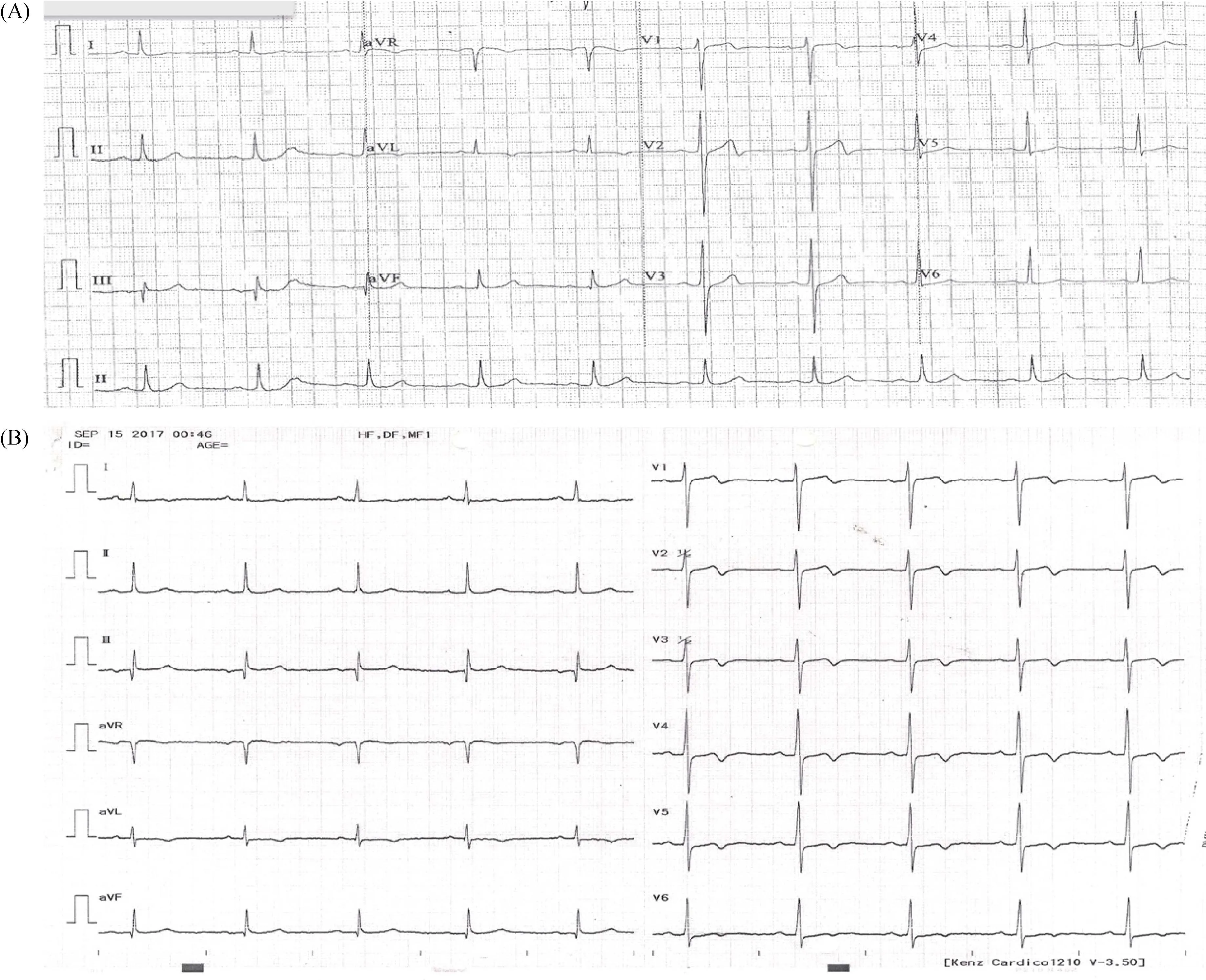
Figure 1. Initial electrocardiogram. (A): Captured during a period of no chest discomfort, revealed sinus rhythm with biphasic T-waves in V1-V3. Positive P wave in leads I and II, Q wave (4 mm) in lead III, ST depression (0.5 mm) in V4 and V5, narrow QRS complex, T-wave inversion (1 mm) in aVL, and normal R wave progression. Consistent with Wellens pattern Type 2. (B): More pronounced biphasic T-wave in V3 and new T-wave inversions in V4-V6.
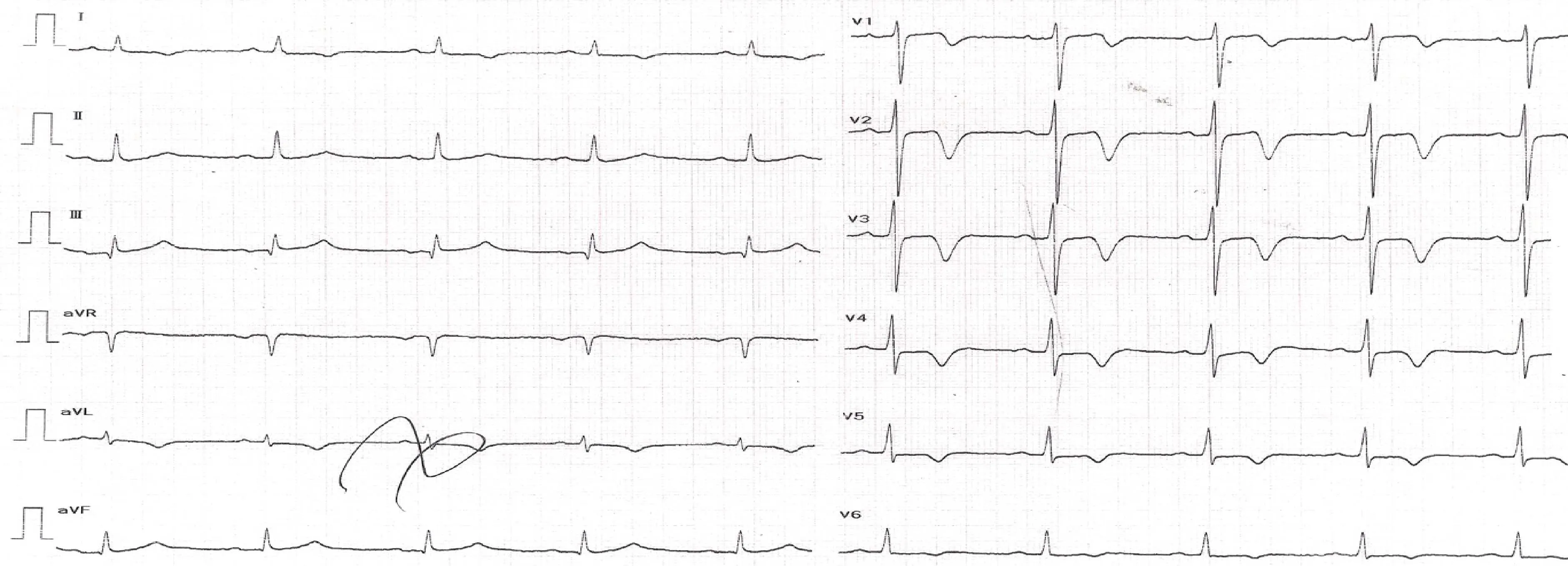
Figure 2. Electrocardiogram. T-wave inversions in V2 (8 mm), V3 (7.5 mm), V4 (4 mm), V5 (2 mm), V6 (1 mm), and aVL (2 mm); biphasic T-wave V1. Positive P wave in Lead I and II, Q wave (1 mm) in lead III, ST depression (1 mm) in V4 and V5, narrow QRS complex,normal R wave progression. Consistent with Wellens pattern type 1.
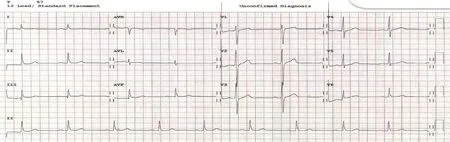
Figure 3. Electrocardiogram after cardiac catheterization and the placement of two drug-eluding stents: normal sinus rhythm without any T-wave inversions or biphasic T-waves.
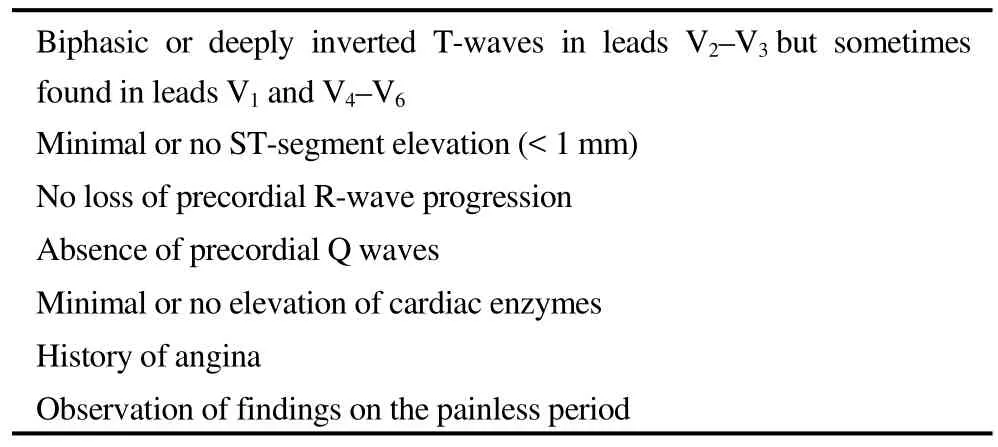
Table 1. Clinical and electrocardiographic criteria for Wellens pattern.
lenging diagnosis, given the possible absence of symptoms and pseudo-normalization of ECG patterns and normal cardiac enzyme or biomarker levels.[8]It is important that the literature has reported on fatal MIs due to exercise stress testing for “non-specific ST-segment or T-wave changes” in patients with missed Wellens pattern.[9]In summary, ECG changes other than the classic ST elevations and depressions can indicate coronary artery disease, and patients presenting with atypical ECG patterns may also benefit from prompt catheterization.
This case illustrates the importance of recognizing nonconventional ECG presentations of severe coronary artery disease; the dynamic nature of such ECG manifestations that may reflect a spectrum of the ischemic processes; and the value of awareness among clinicians to help make correct and timely decisions to maximize myocardial salvage.Early identification of atypical ECG changes is important because Wellens pattern often occurs in asymptomatic patients with potentially normal cardiac biomarker levels.Nevertheless, these are high-risk patients who require urgent angiography and revascularization to avoid evolution to acute anterior MI and possible sudden death.
 Journal of Geriatric Cardiology2018年11期
Journal of Geriatric Cardiology2018年11期
- Journal of Geriatric Cardiology的其它文章
- Inoperable severe aortic valve stenosis in geriatric patients: treatment options and mortality rates
- Chemical renal artery denervation with appropriate phenol in spontaneously hypertensive rats
- Increased index of microcirculatory resistance in older patients with heart failure with preserved ejection fraction
- Prevalence of iron deficiency in patients aged 75 years or older with heart failure
- Frailty significantly impairs the short term prognosis in elderly patients with heart failure
- Association of invasive treatment and lower mortality of patients ≥ 80 years with acute myocardial infarction: a propensity-matched analysis
