Inoperable severe aortic valve stenosis in geriatric patients: treatment options and mortality rates
Julie Paul, Jo?lle Kefer, Marianne Beeckmans, Niko Speybroeck, Benoit Boland,5
1Departments of Geriatric Medicine, Cliniques universitaires Saint-Luc, Brussels, Belgium
2Departments of Cardiology, Cliniques universitaires Saint-Luc, Brussels, Belgium
3Clinical Research, Université catholique de Louvain, Brussels, Belgium
4Departments of Biostatistics, Université catholique de Louvain, Brussels, Belgium
5Institutes of Health and Society, Université catholique de Louvain, Brussels, Belgium
Keywords: Aortic valve stenosis; Medical treatment; The elderly; Transaortic valve implantation
Among geriatric patients suffering from severe but inoperable aortic valve stenosis because of high surgical risk and severe co-morbidities,[1]some benefit from trans-aortic valve implantation (TAVI) while others are deemed too frail for TAVI and received medical treatment (MT). This study conducted in frail geriatric patients aimed at describing the patient’s characteristics and the mortality rate associated with the treatment option (MT vs. TAVI) as well as the patient’s characteristics associated with one-year mortality.
We conducted a retrospective cohort study of 110 consecutive very old patients with a geriatric profile admitted with severe and symptomatic aortic valve stenosis to the Cardiology Department of a Belgian academic hospital between January 2009 and July 2013.
Four inclusion criteria had to be met, namely older age(75 years or more), severe (valve area < 1.0 cm2 on echocardiography and symptomatic (NYHA ≥ class II, or syncope) aortic valve stenosis, contra-indication to aortic surgery according to the heart team (based on clinical evaluation and EuroSCORE), and a geriatric profile confirmed by the mobile geriatric team according to a comprehensive geriatric assessment.
Medical and cardiac data was collected by cardiologists:weight, height, glomerular filtration rate (GFR, mL/min)and other cardiac and medical conditions belonging to logistic Euro-SCORE I and Charlson co-morbidity index.[2]Aortic valve orifice area and transvalvular mean gradient were measured by transthoracic and/or transoesophageal echocardiography. The geriatric liaison team collected the geriatric data: malnutrition (BMI < 21 kg/m2 or/and albuminemia < 3 g/dL), polymedication (≥ 8 daily drugs), dementia (known diagnosis), functional dependency two weeks before admission (Lawton < 3/7), falls during past year, and risk of functional decline (SHERPA ≥ 7).
The treatment option decision (TAVI vs. MT) was made by the heart team (cardiologists and cardiac surgeons) according to the patient’s cardiac, medical and geriatric conditions. There was at that time (2009–2013) no official framework to guide the decision making. MT was essentially supportive, focusing on symptoms relief with medications(angiotensin converting enzyme inhibitor/angiotensin receptor blocker, β-blockers, diuretics, and if needed morphine). The survival status and the date of death were obtained through the Belgian National Registry.
Data are presented as mean ± SD unless otherwise stated,while dichotomous variables are presented as proportions(%). For the sake of clinical interpretation, some continuous variables were dichotomized: Charlson index > 3, number of daily medications at home ≥ 8 drugs (median number),SHERPA score > 7, and Lawton score < 3. Analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago,Illinois). Differences between patient groups (MT versus TAVI) were analyzed by Student t test for continuous variables, or χ2 test for categorical variables. The survival analyses were conducted with the coxph command in R version 3.3.2.[3]Survival curves according to AS treatment(MT vs. TAVI) were established by the Kaplan-Meier estimation method. A P value < 0.05 was considered statistically significant.
The 110 older patients (mean ± SD: 86 ± 5 years; 57%female) presented with severe cardiac, medical and geriatric profiles (Table 1). The Euro-SCORE logisitic I predicted a 28% one month post-surgical mortality. Geriatric syndromes were present in 83% of the patients, e.g., malnutri-tion (35%), multiple falls (38%), poly-pharmacy (26% prescribed ≥ 10 daily drugs), and dementia/chronic cognitive impairment (14%). Patients were frequently dependent in the activities of daily living (ADL), both the basic (Katz 8.8± 3.2/24; median number of 3 out of 6 domains with dependency) and the instrumental ones (Lawton 3.1 ± 2; median number of 3 out of 7 domains with independency).Upon hospital admission, half of the patients (50%) presented a high risk of functional decline at three months based on a SHERPA score ≥ 7 (Table 1).
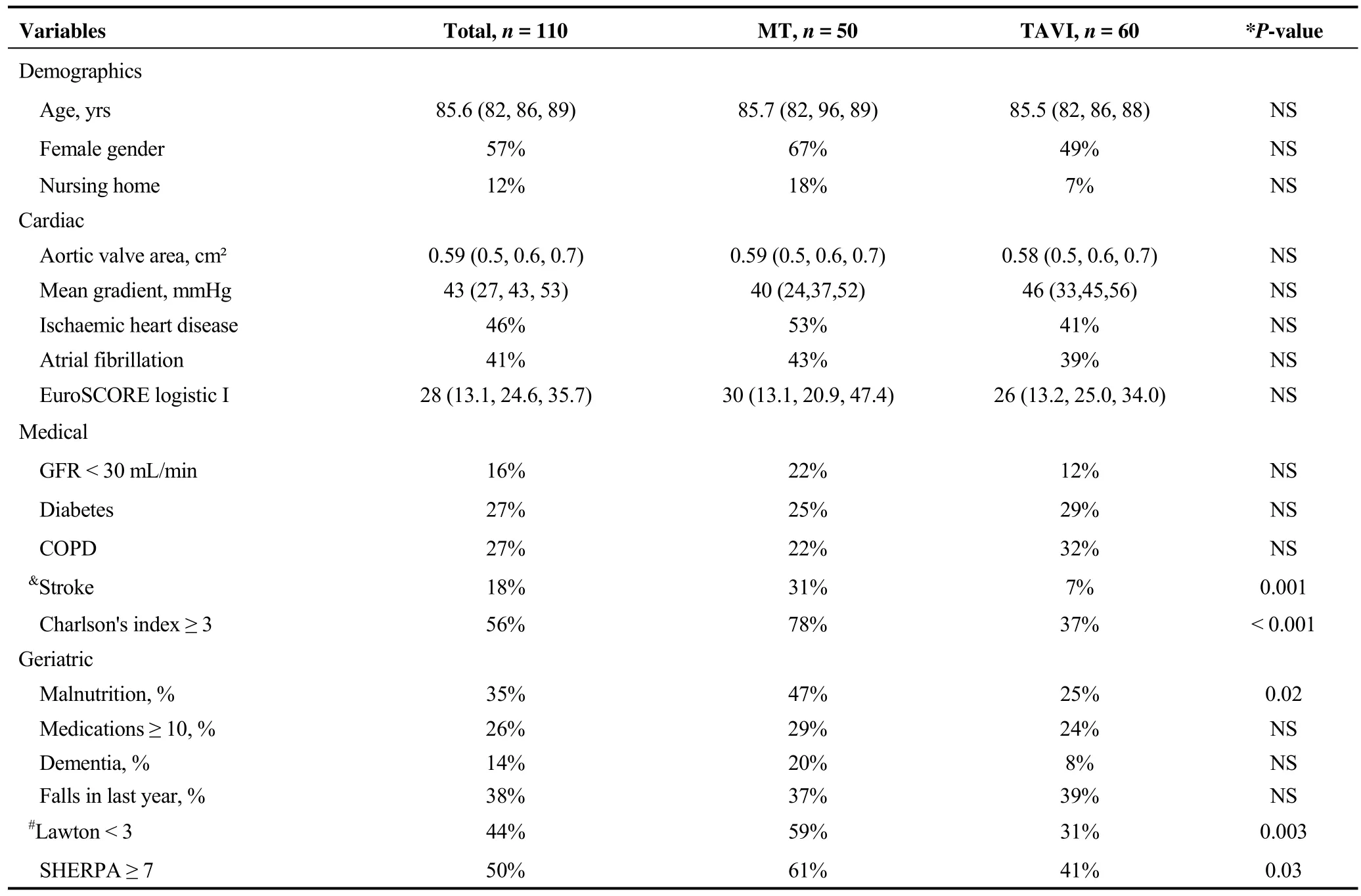
Table 1. Comparison of baseline characteristics in 110 geriatric patients according to the aortic stenosis treatment option: MT vs.TAVI.
According to the heart team decision, 50 patients (45%)received a MT and 60 (55%) underwent a TAVI. Table 1 show that MT and TAVI groups differed in terms of Charlson index and SHERPA score. These two differences were mainly explained by significant differences in, respectively,stroke prevalence and Lawton score.
One-year mortality rate (43/110, 39%) was significantly higher in the presence of five predictors, i.e., GFR < 30 mL/min (83 vs. 30%, P < 0.001), MT (55 vs. 25%, P =0.003), atrial fibrillation (53 vs. 29%, P = 0.02), Charlson index ≥ 3 (50 vs. 25%, P = 0.01) and SHERPA ≥ 7 (49 vs.39%, P = 0.05) (Table 2). The largest mortality difference between the MT and the TAVI groups was noted during the first year of follow-up (Figure 1). At six months, mortality was higher in MT than in TAVI patients (38% vs. 15%, χ2=6.4, OR = 3.45, P = 0.01).[4]In MT patients, the mortality rate was highest during the first months following the hospital stay (12%, 18%, 38%, and 54%, respectively, at 1, 3, 6 and 12 months). The multivariate analysis confirmed the impact on mortality of three factors, namely MT (HR = 3.59,P < 0.001), atrial fibrillation (HR = 2.15, P = 0.002), and renal function (per 1 mL/min GFR decrease, HR = 1.02, P =0.018)
In this study, as expected, TAVI was decided and performed by the heart team in the subgroup of older patients with lower multi-morbidity (Charlson index) and lower risk
of functional decline (SHERPA score). Our results suggest that these two scores were mostly influenced by, respectively, a history of stroke and by a functional dependency in instrumental activities of daily living. The present study confirms that a geriatric assessment by SHERPA provides information about patient robustness, and suggests that the predicting yield of SHERPA is mainly related to its functional domain, collected through the recent patient’s performance in instrumental ADL. These instrumental ADL are important in older patients as they are associated with their recovery after severe medical events such as pneumonia,[5]or heart failure.[6]
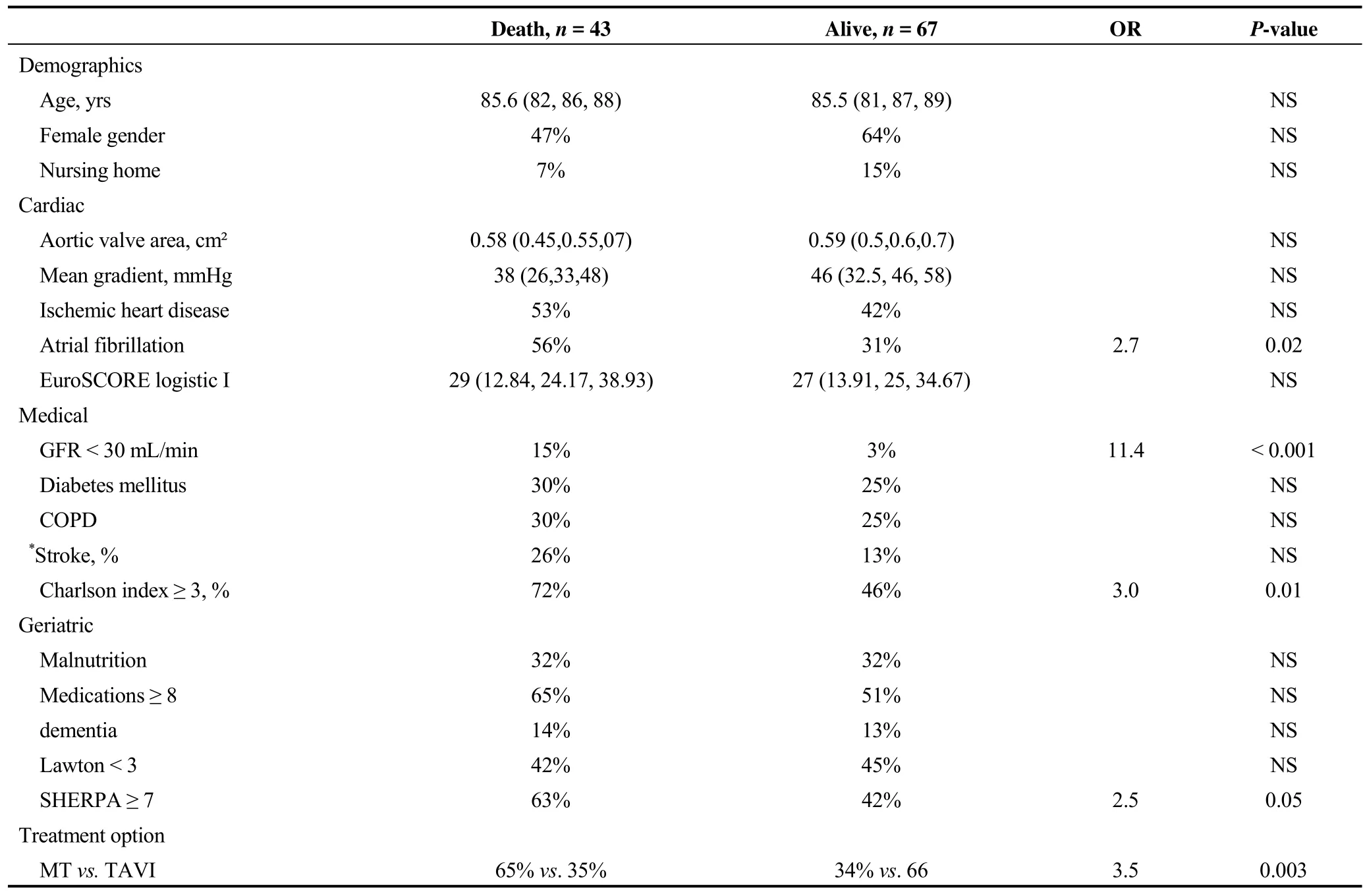
Table 2. Comparison between non-survivors and survivors one year after hospital admission (bi-variate analyses).
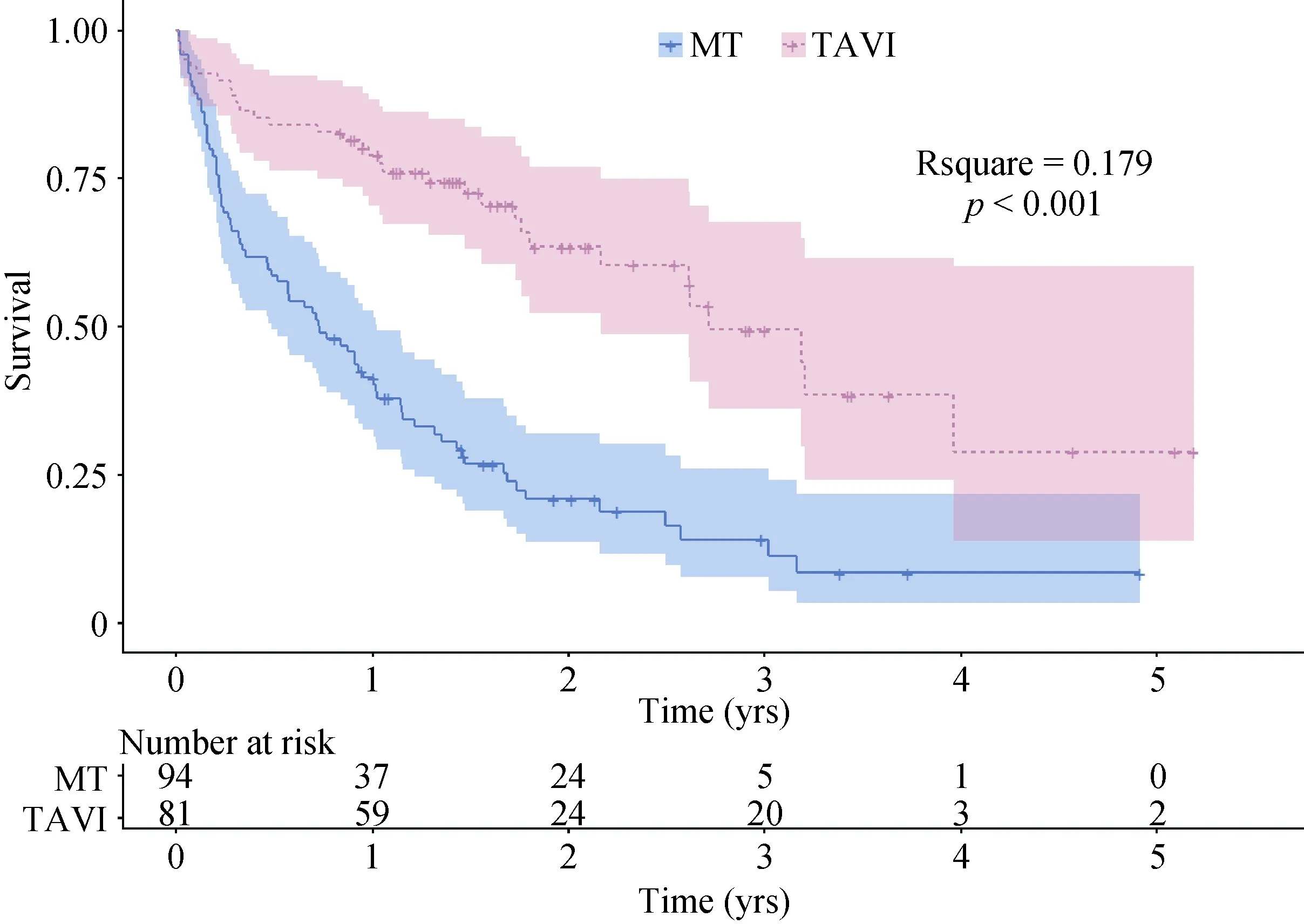
Figure 1. Kaplan-Meier analysis of the survival time in the 110 geriatric patients according to the treatment option. The mortality rate in MT patients (continuous curve) was higher than in TAVI patients (discontinuous line). In MT patients, mortality was highest during the first months following the hospital stay. Results of the multivariate analysis are provided in the text. MT: medical treatment; TAVI:trans-aortic valve implantation.
The one-year mortality rate of 54% in our geriatric patients with MT compares to the 50% observed in the 179 older patients (mean age of 83 years) randomized to the standard therapy arm of the PARTNER trial, cohort B.[7]The one-year mortality was also rather comparable in our TAVI patients and the 179 ones randomized to TAVI (27 vs.30%) in this latter trial. Geriatric features were not reported in this PARTNER trial. These figures confirm that inoperable severe aortic stenosis is a very severe condition with a poor prognosis whatever the TAVI option is, as the general one-year mortality rate in patients aged 80 years or more was 94% in a Belgian population based cohort.[8]In our cohort of very old and geriatric patients, one-year mortality was associated with geriatric features leading to treatment option (MT vs. TAVI) as well as with several medical conditions, i.e., renal impairment, atrial fibrillation and Charlson index. Mortality was thus related to specific baseline geriatric, medical and cardiac features, both in bivariate and multivariate analyses. The present results are in line with those of our previous report in 30 octogenarians undergoing a TAVI where the 27% one-year mortality rate was associated with lower SHERPA scores, renal dysfunction and atrial fibrillation.[9]Euro-SCORE however did not predict mortality neither in this previous study nor in the present one. Euro-SCORE was designed and validated for the prediction of one-month perioperative mortality after open heart surgery and not of one-year mortality after TAVI.Euro-SCORE does not include geriatric variables, which have been shown to predict mortality in older patients undergoing TAVI.
Geriatric features come into play as far as the vital prognosis is concerned in older TAVI patients. In a Swiss study of 100 consecutive older TAVI patients (84 ± 5 years), the 19% one-year mortality was associated in multivariable analysis with probable frailty (odds ratio 3.3) defined in that study according to an index based on performance in the cognitive, nutritional, walking and functional domains(Mini-Mental Status Examination, Mini-Nutritional Assessment, Timed get Up and Go test, and basic ADL, respectively).[10]In a US study gathering 159 older TAVI patients(86 ± 6 years), mortality rate at 300 days was 15%.[11]
The mortality in rate in this latter study was higher in the 83 physically frail than in the 76 other patients (17% vs.7%). This physical frailty score was based on grip strength,gait speed, ADL and serum albumin; geriatric syndromes were not collected.
When severe aortic stenosis in geriatric patents is not treated by surgery or TAVI, the one-year mortality rate is about 50 %, as shown in the PARTNER B trial. Such a high mortality rate among medically treated patients would advocate for considering end-of-life treatment optimization.[8]
Our study has several strengths. We observed a very old population with marked geriatric features, an unfrequently studied but growing population. A one-year follow-up of a population with severe aortic stenosis deemed unable to undergo both surgery and TAVI which has hardly been described yet. We analyzed of the association of geriatric,medical and cardiologic features with both the treatment option (TAVI or MT) and the mortality rate. We identified patient’s characteristics predicting one-year mortality that may help clinicians in the complex decision making of the aortic stenosis treatment choice.
The study presents some limitations. Firstly, its singlecentered design limited the size of this geriatric cohort.Geriatric evaluation may differ across hospitals, hampering geriatric data sharing. The limited study size was also related to the inclusion criteria specific to geriatric patients, and to the need of analyzing patients with a full data set for the sake of the multivariate analysis. Secondly, because of its retrospective design, our study could not collect information on patient’s functional status overtime, nor on the cause of the death when it occurred. Finally, our AS definition was only based on valve area but new recommendations redefine AS with a new algorithm taking also into account gradient.[12]
In conclusion, in very old and geriatric patients with severe inoperable aortic valve stenosis, both multi-morbidity(Charlson index) and geriatric features (functional status and malnutrition) were associated with the heart team decision making as to whether TAVI or MT was the appropriate treatment option. The one-year mortality in this geriatric cohort was predicted by the treatment option (and thus its main predictors) as well as by the baseline cardiac rhythm,renal function and Charlson index. These findings confirm the need for a multidisciplinary medical approach of the geriatric patients with severe aortic valve stenosis. The option of MT should be considered as a red flag for an end-of-life treatment optimization for those very old and very frail cardiac patients.
 Journal of Geriatric Cardiology2018年11期
Journal of Geriatric Cardiology2018年11期
- Journal of Geriatric Cardiology的其它文章
- Atypical electrocardiographic manifestations of ischemia: a case of dynamic Wellens patterns
- Chemical renal artery denervation with appropriate phenol in spontaneously hypertensive rats
- Increased index of microcirculatory resistance in older patients with heart failure with preserved ejection fraction
- Prevalence of iron deficiency in patients aged 75 years or older with heart failure
- Frailty significantly impairs the short term prognosis in elderly patients with heart failure
- Association of invasive treatment and lower mortality of patients ≥ 80 years with acute myocardial infarction: a propensity-matched analysis
