Association of invasive treatment and lower mortality of patients ≥ 80 years with acute myocardial infarction: a propensity-matched analysis
Shuo-Lin LIU, Na-Qiong WU, Meng ZHANG, Jing-Lu JIN, Bing-Yang ZHOU, Qian DONG, Jian-Jun LI
Division of Dyslipidemia, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Abstract Objective To investigate whether invasive strategy was associated with lower mortality in Chinese patients ≥ 80 years with acute myocardial infarction (AMI). Methods We used retrospective data from our center between 2013 and 2017. During a median of 17.4 (interquartile range: 7.3–32.3) months follow-up, 120 deaths were recorded among 514 consecutive patients ≥ 80 years with AMI. The patients were divided into two groups: invasive treatment group (IT group, n = 269) and conservative treatment group (CT group, n = 245), which were also then compared with propensity score matching. Results High mortality was found in CT group compared with that in the IT one.Cox proportional hazard regression analysis showed that invasive treatment was associated with lower mortality of patients ≥ 80 years.Moreover, the results revealed that the patients in IT group had lower in-hospital mortality (3.35% vs. 9.39%, P = 0.005). Besides, the Kaplan-Meier analysis revealed that the mortality was significantly lower in IT group compared with that in CT group using entire and propensity-matched cohort analysis (P < 0.001, respectively). Conclusions Our data suggested that IT appeared to be associated with lower mortality in Chinese patients ≥ 80 years with AMI, which consists with previous studies in spite of either ST elevated myocardial infarction(STEMI) or non-STEMI (NSTEMI) patients.
Keywords: Mortality; Myocardial infarction; Percutaneous coronary intervention; The elderly
1 Introduction
The global population was expected to grow from 6 billion at present to about 9.4 billion by 2050, with the ageing as the most pressing population issue facing humanity in the near future.[1,2]In very elderly patients, cardiovascular diseases now count among the principal causes of death.[3]Acute myocardial infarction (AMI) results in more complications, poor clinical outcomes and incremental mortality in patients 80 years compared with patients at younger age,[4-7]and advanced age is associated with an increased mortality in AMI.[10]
Primary percutaneous coronary intervention (PCI) was recommended by present guidelines in patients presenting with AMI. Should very elderly patients admitted with AMI accept for a routine invasive approach? Limited data are available on the outcome of PCI in patients ≥ 80 years, for the subgroup of patients aged 80 or older are under-represented in randomized controlled trials comparing the effect of invasive strategy and conservative medical strategy,and the subsequent analysis of benefits and disadvantages about in-hospital and follow-up mortality in this particular population are uncertain.[8-11]
The present study aimed to identify whether invasive treatment could improve outcomes of patients ≥ 80 years with AMI during nearly two years follow-up period compared with conservative treatment. We put forward a hypothesis that invasive treatment, which including PCI and coronary artery bypass graft (CABG), is associated with lower in-hospital and intermediate-term mortality in patients≥ 80 years with AMI.
2 Methods
2.1 Study design
Participants in the present study were divided into two groups according to the follow-up survival status: alive group and death group. Then, in order to investigate whether invasive treatment was associated with mortality benefit, we divided all patients into two groups according to different treatment strategies: invasive treatment group (early coronary angiography with immediate assessment for PCI and CABG) and conservative treatment group (optimal medical treatment alone). Univariate and multivariate Cox proportional hazards regression analysis of the mortality was carried out to examine the independent risk factors of death.
2.2 Study population
Our study abided by the Declaration of Helsinki, and the study protocol was approved by the ethical review board of the Fu Wai hospital & National Center for Cardiovascular Diseases, Beijing, China. Their informed, written consents were received for all patients.
From January 2012 to August 2017, 514 consecutive patients ≥ 80 years with AMI were enrolled in the present study. We made a diagnosis of patients with ST elevated myocardial infarction (STEMI) according to the third universal definition of myocardial infarction.[12]Briefly, diagnosis was given if the detection of positive myocardial markers of necrosis (MB fraction of creatine kinase, preferably cardiac troponin I and T) with typical temporal evolution associated with at least one of the evidence of ischemia based on the following conditions existed: acute onset of typical ischemic chest pain 20 min or more; imaging evidence of new loss of viable myocardium or new regional wall motion abnormality; ST-segment elevation of at least 1 mm in two or more contiguous leads, or development of pathological Q waves in electrocardiogram with dynamic change or new left bundle branch block.[12]
The diagnosis of Non-STEMI was made if such conditions existed covering the typical chest pain symptom or breath shortness, electrocardiogram showing normal findings or pathological Q wave, or persistent or dynamic electrocardiographic change of ST depression > 0.5 mm, or new deep T-wave inversion in more than 2 contiguous leads,imaging evidence of new loss of viable myocardium or new regional wall motion abnormality, with an elevation of troponin T or I.[12]
2.3 Date collection
The demographic and clinical characteristics of all patients were recorded: age, gender, body mass index (BMI),past history including history of hypercholesterolemia, diabetes, hypertension, and smoking status; prior angina, prior myocardial infarction, prior PCI and prior CABG;[13]comorbidities: prior stroke and history of chronic kidney disease; and clinical presentation: Killip class,[14]blood pressure, heart rate; in-hospital medications and invasive procedures. The chronic kidney disease was defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2.[15]Stroke was defined as a new focal neurological deficit of vascular origin lasting more than 24 h.[16]
2.4 Gensini score calculation
The severity of coronary artery was commonly evaluated according to the Gensini score (GS) in our groups. The process was computed by assigning the severity score of each coronary stenosis, and the GS was expressed as the total of the score of all the coronary arteries.[17]GS was approximately equal to the score of luminal narrowing multiplied by the score of its geographic importance as demonstrated by numbers of studies.
2.5 Follow-up
We prospectively followed up discharged patients every six months by standardized telephone interviews conducted by trained doctors, who did not know the purpose of our research in advance. We defined the primary endpoint as the happening of all-cause death during the follow-up. The secondary follow-up clinical endpoint included non-fatal MI,unstable angina needed for hospitalization, stroke, and unexpected coronary revascularization (including PCI and CABG) because of clinical deterioration. Non-fatal MI was defined as increased myocardial zymogram along with typical chest pain or typical electrocardiogram changes or new dysfunction of ventricular wall motion. For dead patients, data were collected from their families and hospitals.
2.6 Statistical analysis
Continuous variables were presented as the mean ± SD or median with interquartile range and were assessed by Student’s t-tests, one-way ANOVA, or Mann-Whiteney U tests as appropriate. Categorical variables were expressed as numbers and percentages and were examined by chi-square tests.
Because patients were not randomly received either type of treatment, clinical follow-up outcomes of both groups were compared using the propensity score (PS) matching. A logistic regression analysis was used to evaluate propensity scores among patients receiving invasive treatment or conservative treatment with baseline and clinical variables included as predictors. Variables associated with invasive treatment included age, BMI, hypertension, hyperlipidemia,diabetes, active smoking, prior myocardial infarction and family history. Patients receiving invasive treatment were matched in a 1: 1 accommodation to patients receiving con-servative treatment on the strength of the approximated propensity score of each patient (the match tolerance was 0.01).
The odds ratio (OR) of in-hospital mortality and its 95%CI for patients receiving invasive treatment were calculated by logistic regression. The Hazard ratio (HR) of follow-up endpoints and its 95% CI were calculated for invasive strategy versus conservative strategy by univariate and multivariate Cox proportional regression analyses. Then HR were adjusted for age, including age > 85 years old, sex,current smokers, hypertension, hypercholesterolemia, diabetes, prior myocardial infarction, prior stroke, systolic blood pressure < 100 mmHg, heart rate < 100 beats/min,hemoglobin < 10 g/dL, Killip class, chronic kidney disease and Gensini score, all of which may confound the relationship between invasive treatment and follow-up mortalities.The event-free Survival curves between invasive treatment and conservative treatment groups were assessed by the Kaplan-Meier method and compared by the log-rank test among the entire cohort and the matched cohort.
The statistical analysis was achieved by SPSS version 22.0 software (SPSS Inc., Chicago, IL). For all analyses,two-tailed P < 0.05 was considered significant.
3 Results
3.1 Baseline characteristic of patients with different survival status
From January 2012 to August 2017, the present study enrolled 514 eligible patients ≥ 80 years with AMI. The median age was 82 years, and the age range of the study was 80-94 years old.
There were 32 patients dead in hospital (6.23%), among them, patients with IT group had lower in-hospital mortality in both entire cohort (3.35% vs. 9.39%, P = 0.005) and propensity score matched cohort (2.78% vs. 9.26%, P = 0.001).For the other 482 patients, the median period of follow-up was17.4 (IQR: 7.3–32.3) months. Moreover, there were 88 deaths (18.26%) during the follow-up period and 394 alive(81.74%) at the end of follow-up. 69 cardiovascular events occurred in the alive group. Among them, 10 patients(14.49%) had a stroke, 10 (14.49%) developed non-fatal MI,41 (59.42%) developed heart failure and 6 (8.70%) underwent PCI or CABG.
The baseline characteristics of the patients, stratified by follow-up survival status, were reported in Table 1. No significant difference in age or sex was found in both groups.However, the dead group had lower BMI (23.15 ± 3.33 vs.24.00 ± 3.51, P = 0.021), higher percentage of hypertension(78.63% vs. 69.27%, P = 0.049) and hyperlipidemia (73.50%vs. 82.12%, P = 0.04). In addition, the percentage of severe heart failure was considerably higher in the dead group(13.68% vs. 3.78%, P < 0.001). Patient ≥ 80 years alive had lower Killip classification (1.0 vs. 2.0, P < 0.001), higher Gensini score (43.01 ± 38.16 vs. 31.39 ± 45.95, P < 0.006)and a lower rate of atrioventricular block (11.97% vs. 5.29%,P = 0.012). Patients in alive group were more often used angiotensin-converting enzyme inhibitor/ angiotensin receptor blocker (ACEI/ARB), statins, nitrates and IIB-IIIA antagonists than those in the dead group. The use of betablockers, Ca2+channel blockers and aspirin had not significant difference in both groups.
The patients in the dead group had higher creatinine,higher NT-proBNP, higher percentage of the history of prior MI while they had lower hemoglobin, lower FT3 and less likely underwent coronary angiography.
3.2 Baseline characteristic of patients with different treatment strategies
Then, all the patients were allocated to two groups: invasive treatment group (n = 269) and conservative treatment group (n = 245). Among the invasive treatment group, 252(93.68%) patients underwent PCI, and first-generation drugeluting stents were implanted if necessary, while 161 patients (59.85%) received complete revascularization. 17(6.32%) patients underwent coronary artery bypass graft.Patients ≥ 80 years who receive invasive treatment had higher total cholesterol (4.13 ± 1.14 vs. 3.09 ± 0.94, P <0.001), higher low-density lipoprotein cholesterol (LDL-C)(1.76 ± 0.58 vs. 2.49 ± 0.95, P < 0.01), higher percentages of STEMI, severe heart failure, higher Killip classification,more numbers of vessel disease of the coronary artery and more use of angiotensin-converting enzyme inhibitors,while they had lower percentages of atrial fibrillation, less history of prior AMI and prior CABG, lower rates of NSTEMI. However, no significant differences were observed in age, sex, the use of aspirin, IIB-IIIA antagonists,statins, nitrates, beta-blockers, and Ca2+channel blockers(Table 2).
A total of 216 patients adjusted to determinants of invasive treatment were generated by propensity score matching(Table 2).
3.3 Predictors of the mortality of patients ≥ 80 years with myocardial infarction
In the propensity matched cohort, univariate Cox proportional hazards regression analysis found that invasive treatment was associated with lower intermediate-term mortality of patients ≥ 80 years (HR: 0.36, 95% CI: 0.24-0.53, P <0.001). We also found that hypercholesterolemia, hemoglobin < 10 g/L, higher Killip class, and higher Gensini scorewere risk factors of mortality. Therefore, multivariate Cox proportional hazard regression analysis was performed with the purpose of exploring risk factors associated with mortality of the patients ≥ 80 years with AMI. After fully adjusting for potential risk factors, including age > 85 years old, sex,current smokers, hypertension, hypercholesterolemia, diabetes, prior myocardial infarction, prior stroke, systolic blood pressure < 100 mmHg, heart rate < 100 beats/min,hemoglobin < 10 g/L, Killip class, chronic kidney disease,Gensini score and revascularization, invasive treatment was found to have a negative association with all-cause mortality independently (HR: 0.48, 95% CI: 0.26-0.89, P = 0.01)(Table 3).
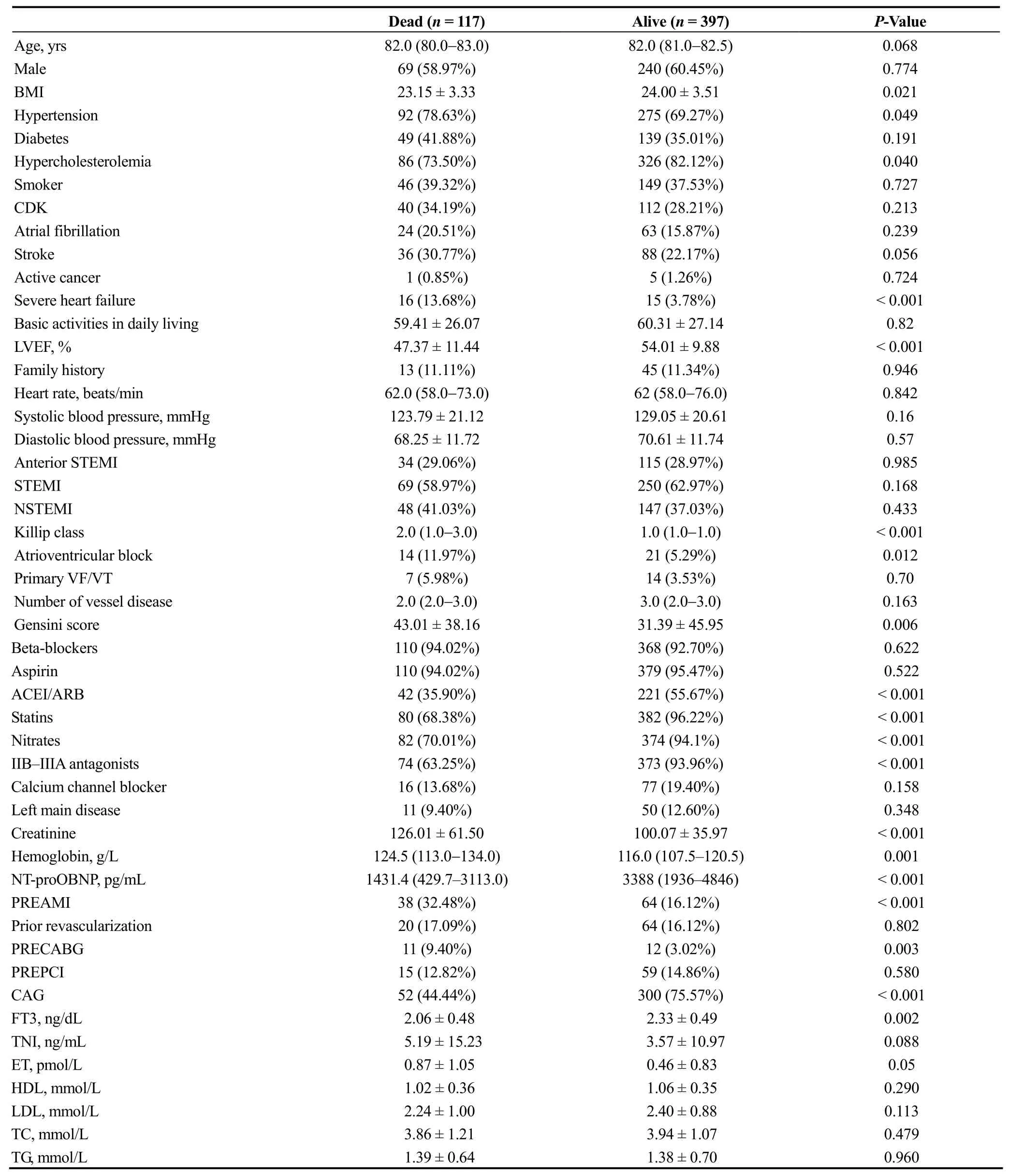
Table 1. Baseline characteristics of enrolled patients according to outcomes.
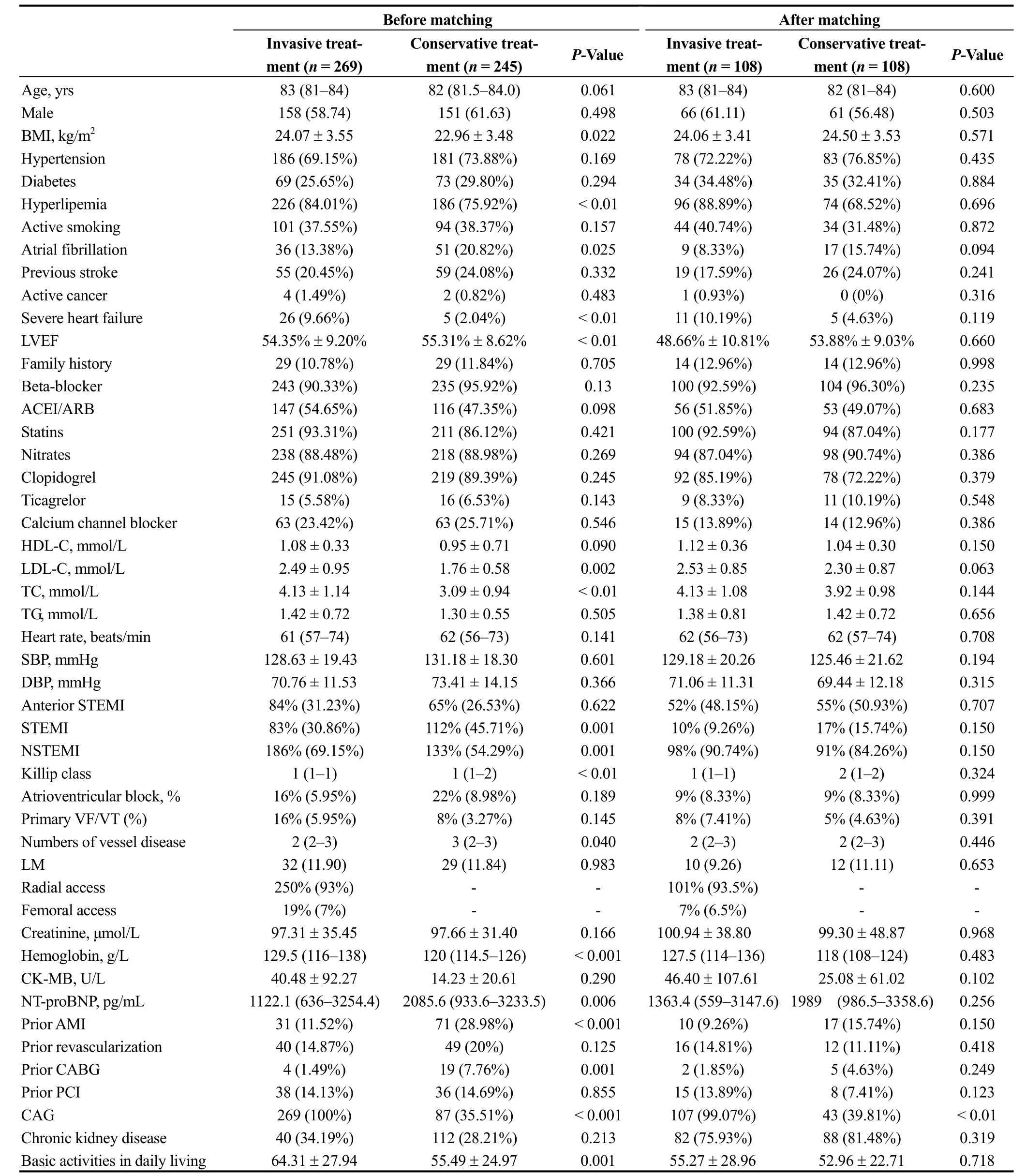
Table 2. Baseline characteristics of enrolled patients by treatment strategies before and after matching.
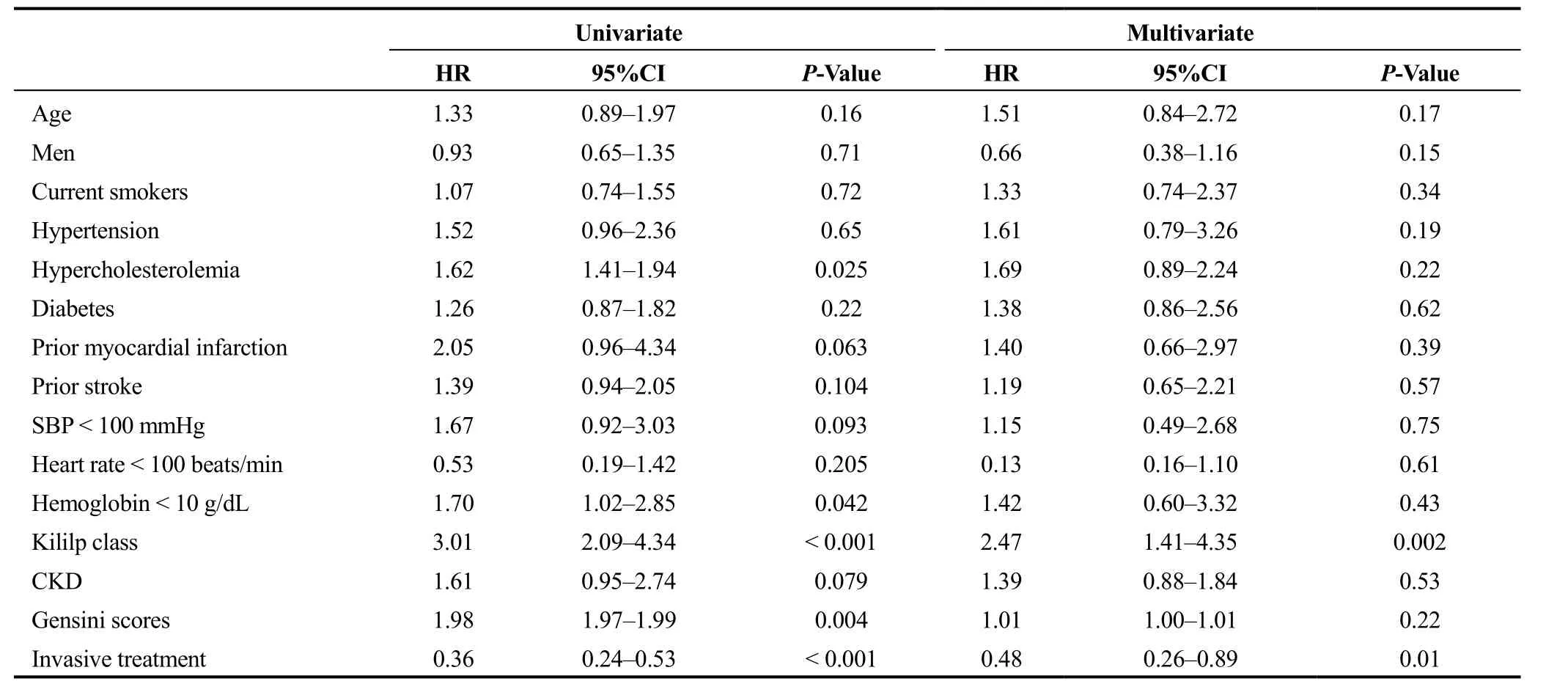
Table 3. Cox regression analysis of mortality predictors of studied patients.
3.4 The mortality of the patients in different treatment groups
For patients ≥ 80 years with AMI, the composite events which include myocardial infarction, need for urgent revascularization, stroke, or death did not reach statistical significance between two groups. Whereas, invasive treatment was associated with lower in-hospital mortality (OR: 0.34,95% CI: 0.15-0.74, P = 0.007). For patients with STEMI,invasive treatment was found to be associated with lower in-hospital mortality (OR: 0.38, 95% CI: 0.16-0.94, P <0.05), while for patients with NSTEMI, the correlation between invasive treatment and in-hospital mortality (OR:0.14, 95% CI: 0.02–1.14, P = 0.066) did not reach statistical significance. As showed in Figure 1, the intermediate-term mortality rate was significantly lower for patients ≥ 80 years who received invasive treatment compared with the patients who received conservative treatment, both in STEMI group and NSTEMI group. Figure 2 depicts the Kaplan-Meier survival curves. The higher rate of survival in the patients ≥80 years who received invasive treatment was noted during the follow-up period in the entire as well as the propensity-adjusted cohort (P < 0.001, either).
4 Discussion
The present study at the period of median 17.4 (IQR:7.3–32.3) months of follow up of the very elderly showed that the invasive treatment (PCI and CABG) was associated with intermediate-term all-cause mortality in comparison to a conservative strategy which only includes optimum medical treatment. The results were seen in patients with both STEMI and NSTEMI.
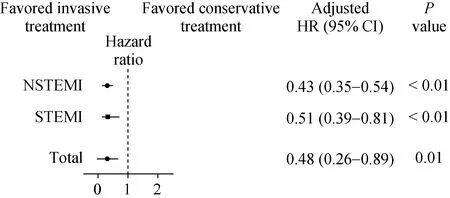
Figure 1. Efficiency in subgroup analysis by treatment on mortality according to ST elevation. STEMI: ST elevation myocardial infarction; NSTEMI: non-ST elevation myocardial infarction.
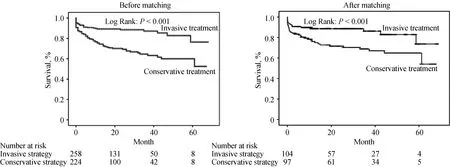
Figure 2. Kaplan-Meier curves of death by treatment groups.
The China PEACE-Retrospective Acute Myocardial Infarction Study[18]showed that rates of patients receiving reperfusion therapies in China were much lower than those in the USA or Europe,[19,20]and the rate of primary percutaneous coronary intervention was still low.[18]Furthermore,the general population is ageing, patients ≥ 80 years account for a growing proportion of the population with AMI. PCI for most patients with STEMI[21,22]or with non ST-elevation acute coronary syndrome (NSTE-ACS)[22]was recommend by the current guidelines, however, the very elderly with AMI, especially patients ≥ 80 years, seldom receive invasive treatment the guidelines recommended and were treated more conservatively compared to their younger counterparts,because they were more likely had atypical symptoms, frequently with more complications, had higher rate of death.[23,24]Meanwhile, these patients had been scarcely represented in clinical trials comparing treatment strategies in AMI.[25]Thus, the treatment strategies of elderly patients with AMI, especially patients ≥ 80 years, lack evidence at present.
Compared with ACOS registry,[26]PL-ACS,[27]the present study had a lower rate of hypertension, diabetes, previous myocardial infarction and hypercholesterolemia, whereas, the rates of these comorbidities in our study were higher than After Eighty Registry.[28]Besides, the rate of the previous stroke was highest among them. In accordance with the results of the present study, ACOS study[26]and PL-ACS Registry study[27]showed the reduction of in-hospital mortality in invasive therapy group compared with conservative treatment group. The After Eighty study showed that invasive strategy had an advantage over conservative strategy in reducing composite events, including stroke, MI, need for urgent revascularization and death, for patients aged 80 years or older after presenting with NSTEMI or unstable angina.[28]On the contrary, the Italian Elderly ACS study showed that there were no differences between routine invasive therapy and initial medical management at one year,and there were no statistically significant findings of the in-hospital mortality between two groups.[29]The present study found that invasive treatment was associated with lower intermediate-term mortality for the patients aged 80 or older with NSTEMI, but there was no statistical significance between IT group and CT group about the composite endpoints of myocardial infarction, need for urgent revascularization, stroke, and death. Compared with other trials,the lower rate of invasive treatment (52.34%) and the higher rate of death (18.26%) probably explain these differences.
As for elderly patients with STEMI, a few research have found that the mortality of patients aged 80 or more with STEMI was associated with many risk factors, including age, history of hypertension,[30]history of diabetes mellitus,longstanding ischemic heart disease (prior myocardial infarction), lower heart rate, Killip class ≥ 2,[30]lower hemoglobin, renal dysfunction, and revascularization. Among them, revascularization was one of the most robust predictors of short-term[31,32]and intermediate-term mortality.[33-35]Even for patients aged ≥ 85 years or older with STEMI,who underwent invasive management, have better shortand long-term outcomes,[36-38]meanwhile, aggressive treatment is associated with excellent quality of life.[39]Our results are in accordance with the previous studies, showing that better intermediate-term survival and lower in-hospital are associated with invasive treatment of STEMI patients ≥80 years. Thus, should all very elderly patients with AMI through a regular invasive process? The data of the present study indicated that invasive strategy might be associated with better prognosis of AMI patients aged 80 or older, certainly, each patient should receive individualized treatment,and random control trials of two treatment strategies were needed to verify that hypothesis.
4.1 Study limitations
There are some limitations in our study. Firstly, as an observational study, there may be bias from non-random assignment of exposure, unmeasured confounders like frailty,cognitive status and physical performance might influence the choice of treatment in patients with AMI, while selection bias and other significant differences observed between two groups can be balanced in some measure by propensity-score matching. Furthermore, the bleeding event was not registered in evaluating the intermediate-term outcomes of subjects receiving invasive strategy, however, results of the After Eighty study[28]showed no difference of bleeding complications between the invasive strategy and the conservative strategy. The time to PCI and the type of PCI were also associated with long-term clinical outcome,[40]we did not analyze the time to PCI, and the type of PCI (primary PCI, rescue PCI, delayed PCI) of patients underwent revascularization, which may be a confounder of our study.
4.2 Conclusions
This study indicates that the invasive strategy including PCI and CABG is more associated with lower intermediate-term mortality compared with the conservative strategy of using optimal medical treatment alone for patients older than 80 years presenting with or without ST elevation.Moreover, patients ≥ 80 years with STEMI who received invasive treatment during hospitalization had a lower risk of in-hospital mortality.
Acknowledgements
We declare that we do not have any conflict of interest.This work was partially supported by the Capital Health Development Fund (201614035) and CAMS Major Collaborative Innovation Project (2016-I2M-1-011) awarded to Dr. Jian-Jun LI.
 Journal of Geriatric Cardiology2018年11期
Journal of Geriatric Cardiology2018年11期
- Journal of Geriatric Cardiology的其它文章
- Atypical electrocardiographic manifestations of ischemia: a case of dynamic Wellens patterns
- Inoperable severe aortic valve stenosis in geriatric patients: treatment options and mortality rates
- Chemical renal artery denervation with appropriate phenol in spontaneously hypertensive rats
- Increased index of microcirculatory resistance in older patients with heart failure with preserved ejection fraction
- Prevalence of iron deficiency in patients aged 75 years or older with heart failure
- Frailty significantly impairs the short term prognosis in elderly patients with heart failure
