Natriuretic peptide family as diagnostic/prognostic biomarker and treatment modality in management of adult and geriatric patients with heart failure: remaining issues and challenges
Zhen–Lu ZHANG, Ran LI, Fei–Yan YANG, Lei XI
?
Natriuretic peptide family as diagnostic/prognostic biomarker and treatment modality in management of adult and geriatric patients with heart failure: remaining issues and challenges
Zhen–Lu ZHANG1, Ran LI1, Fei–Yan YANG2, Lei XI3
1Department of Clinical Laboratory, Wuhan Asia Heart Hospital, Wuhan University, Wuhan, China2Department of Cardiology, The Central Hospital of Wuhan, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China3Division of Cardiology, Pauley Heart Center, Virginia Commonwealth University, Richmond, VA, United States
B-type natriuretic peptide (BNP) and N-terminal proBNP (NT-proBNP), the key members of natriuretic peptide family have been recommended as the gold standard biomarkers for the diagnosis and prognosis of heart failure (HF) according to the current clinical guidelines. However, recent studies have revealed many previously unrecognized features about the natriuretic peptide family, including more accurate utilization of BNP and NT-proBNP in diagnosing HF. The pathophysiological mechanisms behind natriuretic peptide release, breakdown, and clearance are very complex and the diverse nature of circulating natriuretic peptides and fragments makes analytical detection particularly challenging. In addition, a new class of drug therapy, which works via natriuretic peptide family, has also been considered promising for cardiology application. Under this context, our present mini-review aims at providing a critical analysis on these new progresses on BNP and NT-proBNP with a special emphasis on their use in geriatric cardiology settings. We have focused on several remaining issues and challenges regarding the clinical utilization of BNP and NT-proBNP, which include: (1) Different prevalence and diagnostic/prognostic values of BNP isoforms; (2) methodological issues on detection of BNP; (3) glycosylation of proBNP and its effect on biomarker testing; (4) specificity and comparability of BNP/NT-proBNP resulted from different testing platforms; (5) new development of natriuretic peptides as HF treatment modality; (6) BNP paradox in HF; and (7) special considerations of using BNP/NT-proBNP in elderly HF patients. These practical discussions on BNP/NT-proBNP may be instrumental for the healthcare providers in critically interpreting laboratory results and effective management of the HF patients.
J Geriatr Cardiol 2018; 15: 540?546. doi:10.11909/j.issn.1671-5411.2018.08.008
Angiotensin-renin-neprilysin-inhibitors; Biomarker; BNP; Heart failure; NT-proBNP
1 Introduction
It has been increasingly recognized that biomarker test-ing may play a central role in the evidence-based cardio-vascular medicine, which in turn promote the improved clinical outcome, better quality of life, and alleviated socio- economic burden of cardiovascular diseases.[1]Based on the number of Pubmed-indexed publications upon the keyword “Cardiovascular Biomarkers”, there was a five-fold increase between 1995 and 2015[2]and these articles include those related to B-type natriuretic peptide (BNP), an important biomarker that was introduced into clinical application in 2002 and since then it has been widely used for both diagnostic and prognostic purposes in management of adult and elderly patients with heart failure (HF).[3–7]
BNP and N-terminal proBNP (NT-proBNP) are the key members of natriuretic peptide family that have been rec-ommended as the gold standard biomarkers for the diagno-sis and prognosis of HF according to the current clinical guidelines.[8,9]In 2011, van Kimmenade & Januzzi[10]eva--luated BNP/NT-proBNP and other 19 related biomarkers on the aspects of diagnosis, prognosis, and therapy guidance as well as the specificity of cardiac production. They reported that BNP/NT-proBNP have the highest comprehensive scores, which are conceptually consistent with a recent re--view by Ibrahim & Januzzi.[11]Although there is a consen--sus that BNP/NT-proBNP is the primary biomarker of HF, our knowledge about BNP/NT-proBNP remains incomplete and a number of questions demand better answers.[12]For examples, these questions might include: what is the differ-ence and consistency among various BNP detecting plat-forms? How many key steps for degradation of proBNP and does proBNP still exist in the blood circulation after the degradation? How much proBNP interfere with BNP/NT- proBNP detection? What is glycosylated proBNP/NT- proBNP and their influence on the current detection meth-ods? How to standardize natriuretic peptide detections? A comparable number of issues also exist in the therapeutic front. Therefore, this article focuses on providing a concise review and discussion on the unsolved puzzles concerning the clinical use of BNP/NT-proBNP as the essential bio-markers to detect HF in both adult and elderly patients.
2 Different prevalence and diagnostic/pro-gnos-tic values of BNP isoforms
Human BNP is synthesized as a 134-amino acid precursor protein (pre-proBNP) and is subsequently processed to form a 108-amino acid propeptide, proBNP 1–108. Some proprotein convertases (such as corin and furin) are produced in the cardiomyocytes, may process proBNP 1–108 to form two separate peptides: the 76-amino acid N-terminal peptide, proBNP 1–76 (the so-called NT-proBNP), and the biologically active 32-amino acid C-terminal peptide, proBNP 77–108 (usually called BNP). B-type natriuretic peptides have an intact cysteine-ring that is able to bind to the specific natriuretic receptors to afford their regulatory function that is known to be central to cardiovascular homeostasis, including natriuresis, diuresis, vasodilation, and inhibition of inflammatory processes. It is realized that this process is complicated and influenced by multiple factors. ProBNP and NT-proBNP (and probably other shorter peptides derived from these precursors) are present in plasma in both glycosylated and non-glycosylated forms.[13]BNP 1–32 will be further degraded by related receptors and some enzyme like neutral endopeptidase (NEP), dipeptidyl peptidase-IV, IDE, methyldopa and other possible pathways. The bioactive BNP 1–32 is further processed by receptors or enzymes like neprilysin, dipeptidyl peptidase IV, insulin degrading enzyme, meprin, and potentially other enzymatic pathways which may be identified in the future. Multiple plasma proBNP derived peptides present in heart failure patients will be further truncated.
A multitude of BNP forms are known to be present in the circulation of patients with HF (e.g., BNP 3–29, 3–30, 4–29, 5–29,). Among these, BNP 3–32, 4–32, and 5–32 have been shown in recent studies to be the major forms and BNP 5–32 was recently reported to have the strongest association with prognosis in chronic HF patients.[14]On the other hand, glycosylated form of NT-proBNP are the most prevalent form, whereas very small amount of intact BNP 1–32 remains in the blood circulation.[15]The concentration of circulating natriuretic peptides depends not only on myocardial wall stress, but also on the concentrations of corin and other mediators, such as furin, neprilysin, and proBNP glycosylation. Hypothetically, a patient with a low corin concentration might need a larger stimulus in terms of increased myocardial wall stretch to achieve the same concentrations of circulating natriuretic peptides as a patient with a high corin concentration. In other words, patients with high NT-proBNP and low corin concentrations have the most severe form of HF, which is in accordance with their poorer survival during follow-up.[16]
3 Methodological issues on detection of BNP
Current clinical guidelines in Europe and America for HF diagnosis have used the diagnostic cut-off values of BNP as 100 pg/mL and NT-proBNP as 450 pg/mL, 900 pg/mL, 1800 pg/mL, which are set according to age group and gender of the patients. However, there are concerns and cautions for these cut-off values to be overconfidently used in clinics. First, the BNP test results obtained from Shionogi IRMA platform and Centour platform (using Siemens AIA-ADVIA method) and Tosoh AIA platform (using Tosoh AIA PACK method) are 30%–50% lower than those of AxSYM platform, Architect platform, Alere POCT platform and Beckman DxI and Access platforms, which use Alere Triage method. The BNP cut-off of 100 pg/mL seems more appropriate for the more sensitive platforms.[13]The other factors that may influence the BNP test results include: gender, age, renal function, body mass index, individual biological difference, sample type, tube type, medications taken before blood collection, and blood sample storage time, etc. Since BNP/NT-proBNP is a biomarker of cardiac stress/contraction/volume expansion, the complexity of cardiac hemodynamics can also interfere the interpretation of this biomarker for HF diagnosis. In addition, we should know how much proBNP, glycosylation of proBNP, NT-proBNP and BNP may influence the testing results. The microstructure heterogeneity of natriuretic peptide family is also a matter of special attention.
4 Glycosylation of proBNP and its effect on biomarker testing
O-Glycosylation is the process that glycans attach to the hydroxyl oxygen of serine and threonine on proteins or pep-tides. This important protein modification is comparable to phosphorylation and it can effectively regulate cell func-tion.[17]Most recently, Halfinger,.[18]demonstrated that there are 9 glycosylation sites on proBNP and NT-proBNP by using tandem immunoaffinity purification, sequential exoglycosidase treatment for glycan trimming, high-re-solu-tion nanoflow liquid chromatography electrospray multi-stage mass spectrometry. These nine glycosylation sites are Ser5, Thr14 or Ser15, Thr36, Ser37, Ser44, Thr48, Ser53, Thr58, and Thr71. The glycosylation status of Thr71 was shown to suppress proBNP processing, which leads to the dysfunction of proBNP, since only BNP is biologically ac-tive. It is unknown that whether other glycosylation sites influence the metabolism of proBNP and NT-proBNP. The degree of proBNP glycosylation varies in different patients. It was lower at Thr71 in acute decompensate HF (ADHF, 20%) than in chronic HF (CHF, 31%). Therefore, proBNP likely functions less in CHF.[19]Furthermore, the glycosylation of Ser or Thr blocks the combination of antibodies and epitopes, and in turn affects the testing results. For example, there is an antibody that is specific to the mid-fragment of NT-proBNP (amino acid residues 28–56), which contains several glycosylation sites including Thr36, Ser37, Ser44, Thr48, Ser53, and Thr58. Assays using such an antibody specific to the mid-fragment of NT-proBNP would seriously underestimate the true concentration of NT-proBNP in blood samples. However, after treatment with glycosidases, a substantial increase of the signal, from 5.8- to 41-fold (Mean = 19) was reported.[20]Therefore, one should choose antibodies that only recognize the epitopes other than those of the glycosylation sites of proBNP and NT- proBNP, in order to ensure the accuracy of the testing re-sults.
5 Specificity and comparability of BNP/NT- proBNP resulted from different testing platforms
Following the above-discussed issues, there are major concerns on the comparability among various testing platforms for BNP/NT-proBNP and the relative purity of BNP/ NT-proBNP that we are detecting. Apparently, the analyti-cal differences between assays from various manufacturers may be attributed partially to the different specimen types, platforms, and detecting antibodies. A recent study by Saenger,.[15]indicated that the factors like 9 standard substrates and antibody specificity and glycosylation status would make more difficult to compare the results from dif-ferent testing assays. Regarding the “purity”, glycosylated or truncated prohormone forms are also detected by various BNP, NT-proBNP and proBNP immunoassays.[15]
It is notable that several commercial immunoassays may not recognize all the glycosylation proBNP and NT-proBNP conformations and therefore may underestimate BNP con-centrations in the patients’ samples, even though their clinical symptoms of HF are evident. In addition, these commercially available immunoassays also exhibit large systematic differences between methods because the various assays cross-react to a differing extent with various BNP, NT- proBNP, and proBNP peptides. Recently, Saenger et al. studied nine BNPs including synthetic and recombinant BNP (Shionogi, Scios, Mayo), human and synthetic glycosylated and nonglycosylated NT-proBNP (HyTest, Roche Diagnostics), and human glycosylated and nonglycosylated proBNP (HyTest, Scios).[15]Five BNP [Abbott, Abbott POC, Alere, Beckman Coulter, Siemens (Centaur)], 9 NT-pro-BNP [Ortho-Clinical Diagnostics, Roche, Response, bio-Merieux, Siemens (Dimension, Immulite, Stratus CS), Mit-subishi] and 3 research-use-only proBNP immunoassays [Biosite (Alere), Bio-Rad, Goetze] were also evaluated by these authors.[15]They found that BNP and NT-proBNP assays have substantial cross-reactivity with proBNP peptides. NT-proBNP assays do not detect glycosylated forms of either NT-proBNP or proBNP. ProBNP assays preferentially detect the BNP 1–32 peptide and have minimal cross- reactivity with BNP peptides and glycosylated proBNP. Taken together, we may summarize that: (1) Substantial differences exist between the testing results from various analytical platforms, which would make the BNP, NT- proBN, proBNP results not transferable among the current immunoassays. Therefore, there is no single unified diag-nostic cut-off value that fits all patients; (2) currently avail-able commercial immunoassays detect total concentration of BNP-related peptides; (3) there is a large variance in pro-portions of a variety of BNP-related peptides. Therefore it is not appropriate to utilize human-derived calibrator and syn-thetic calibrators should be used to avoid such cross-reac-tion; and (4) apart from BNP and NT-proBNP, the clinical value of other BNP-related peptides, especially proBNP, should be evaluated. BNP or NT-proBNP results may not be transferable among the immunoassays due to their differences in cross-reactivity and ability to detect various glycosylated forms of proBNP-derived fragments. A standardization of the testing assays is much needed for BNP and NT-proBNP assays.
6 New development of natriuretic peptides as HF treatment modality
BNP possesses significant biological functions in inhib-iting myocardial fibrosis and hypertrophy, inflammation, angiogenesis, and overactivation of renin-angiotensin-aldo-sterone system (RAAS) and sympathetic nervous system. This class of molecules have emerged as a potential thera-peutic strategy for treating cardio-renal diseases via admini-stration of recombinant (nesiritide or ularitide) or synthetic natriuretic peptides (e.g., vasonatrin or CD-NP) and/or en-hancing levels of natriuretic peptides through inhibition of neprilysin, also known as NEP in combination with either inhibition of angiotensin-converting enzyme or angiotensin receptor blockade (e.g., LCZ696). The first approach aims to increase the biological effect of natriuretic peptides and the second approach with drug combination may have broader effects because of the broader biological benefits of neprilysin inhibition plus the presence of vasodilator therapy. NEP inhibition and natriuretic peptides therapy appear to be promising treatments for HF.
NEP (neprilysin) is a zinc-dependent membrane metallopeptidase with a subunit molecular weight of 90 ku and contains glycosylation sites. NEP is widely distributed in various tissues, such as kidney, lung, brain, heart, and vas-culatures. Importantly, the kidney is the richest source of NEP,[21]which degrades a variety of bioactive peptides. Its substrates include natriuretic peptides, which are the important regulators of cardiovascular and renal biology. However, NEP is not very precise in its actions and it hydrolyzes numerous peptides including angiotensin I, angiotensin II, endothelin-1, kinins, adrenomedullin, opioid peptides, enkephalin, gastrin, and amyloid beta.[22]Therefore, such diverse targets of NEP unavoidably lead to certain side effects.[23]For example, as an off-target effect, inhibition of NEP could increase levels of amyloid beta in brain and eyes leading to development of symptomatic Alzheimer’s disease or age-related macular degeneration, respectively and in turn increase the risks of cognitive and/or visual dysfunction that need to be monitored closely when using a NEP inhibitor.
On the other hand, LCZ696 (Entresto) is an advanced inhibitor of angiotensin receptors and a recently approved drug for HF treatment. LCZ696 is orally available and provides an 1:1 ratio blockade of type I angiotensin receptors in a valsartan moiety together with NEP inhibition with AHU377 (Sacubitril), a prodrug moiety that is rapidly metabolized to an active moiety. It enhances natriuretic peptides directly through peptide delivery and hence it should have fewer adverse effects as compared with NEP inhibition.[21]Furthermore, since BNP, not NT-proBNP is the substrate of NEP, circulating BNP can reflect the drug efficacy of LCZ696. Therefore, BNP/NT-proBNP/cyclic guanosine monophosphate (cGMP) concentrations should be monitored during NEP inhibitor treatment. The use of BNP, NT-proBNP, and cGMP as a triad of biomarkers has also been proposed in guiding the treatment using inhibitors of angiotensin receptors like LCZ696.[21]Interestingly, an analysis of the PARAMOUNT trial by Jhund,.[24]indicated the independence of the blood pressure lowering effect and efficacy of LCZ696 in 301 HF patients. They reported that by 12 weeks of drug treatment, the systolic/diastolic blood pressure was reduced by 9 mmHg/5 mmHg in the HF patients receiving LCZ696 in comparison with 3 mmHg/2 mmHg in those receiving valsartan. However, the change in NT-proBNP was poorly correlated with change in blood pressure.[24]
7 BNP paradox in HF
Whereas the plasma level of BNP may serve as an effec-tive biomarker for HF, the therapeutic benefits of BNP have been a matter of puzzling since the increased BNP levels in HF often do not act against congestion, sodium and water retention, and vasoconstriction, although chronic admini-stration of BNP relieved HF symptoms in HF patients. Evi-dence has accumulated supporting the notion that the so-called “BNP paradox” is caused by inaccurate assay measurement, in which plasma BNP is overestimated by proBNP immunoreactivity (due to BNP deficiency or re-duced BNP availability).[16]This BNP paradox in HF may partially be explained by more advanced assays of BNP, NT-proBNP, and proBNP that were developed from mass spectrometry and specific monoclonal antibodies. Such work demonstrated that commercially available assays bind nonspecifically to both proBNP and BNP and its degradation products, and most BNP-immunoreactive forms detected by immunoassay in HF represent proBNP. Therefore, the results obtained from the commercially available kits do not necessarily represent the actual values of mature biologically active BNP in the body.[21]The present commercially available immunoassays for measurement of intact biologically active BNP are inaccurate, because these assays cross-react in a variable but significant degree with proBNP 1–108. Thus the assays yield high results derived by their measurement of a mixture of BNP and proBNP and others do not reflect the actual concentration of active BNP.[18]
8 Special considerations of using BNP/NT- proBNP in elderly HF patients
It has been well recognized that the prevalence of HF rises with age, approximately from 2–3% in adult population to 10–20% at the age of 70–80 years old and consequently about a half of HF patients are over 75 years old.[25,26]The age-associated increasing occurrence and worsen prognosis of HF are likely due to the high prevalence of preexisting structural and functional abnormalities of the heart and the co-morbidities in older patients than young patients. In addition, HF with preserved ejection fraction (HFpEF) is the more common phenotype of HF in elderly people, due to the predominance of female gender and the high prevalence of the above-mentioned age-related cardiac abnormalities, which is usually under-diagnosed because the initial symptoms of HF such as exercise intolerance or decreased functional capacity may be mistakenly attributed to a natural aging-associated decline in cardiac function. It is noteworthy that patients with high NT-proBNP levels but without HF diagnosis have a higher risk of cardiovascular events and mortality and therefore NT-proBNP may be a useful biomarker of silent cardiac damage to identify the patients with HFpEF in elderly patients.[5,27]
However, the interpretation of BNP and NT-proBNP re-sults may be challenging due to several confounding factors such as old age per se, renal dysfunction, obesity and hemodynamic alterations caused by atrial fibrillation, acute coronary syndrome, venous thromboembolism, sepsis, hy-perthyroidism and anemia that are quite common in elderly patients. Among the confounders, age and chronic kidney disease are two major determinants of circulating levels of NT-proBNP, which appear to demand different andspecific cutoffs values in taking account of these factors. Scanty data are available concerning the accuracy of NT-proBNP in diagnosing HF and the effects of comorbidities in very old patients. For example, Bombelli,.[4]studied very elderly patients (86 ± 4.3 years old) to identify the best cutoff point for balancing the biomarker sensitivity and specificity. Ad-ditionally with the aim to rule in or out HF, they identified a NT-proBNP confirmatory threshold with specificity > 85% and a NT-proBNP exclusion threshold with sensitivity > 95%. They identified NT-proBNP < 980 pg/mL as the threshold to rule out HF with 90% sensitivity and NT- proBNP > 5340 pg/mL to rule in HF with 85% specificity. The use of two threshold values resulted in a gray area of diagnostic uncertainty of 42.4% (= 380) of whom 59% did not suffer HF.[4]They further determined a second pair of cutoff values (1470–4200 pg/mL) that reduced the gray-area to 27.4%, while maintained an acceptable diagnostic performance of the commonly used cutoffs (300–1800 pg/mL). This study demonstrated that NT-proBNP may be satisfactorily used for the diagnosis of HF in very elderly patients and also their data did not support the use of different NT-proBNP cutoffs depending on eGFR, Ht and CRP.
On the other hand, a Swedish study by Edvinsson,.[28]reported that BNP is a potent vasodilator in aged human microcirculation and there is a blunted response to BNP in HF patients. These investigators compared 15 HF patients (BNP > 3000 pg/mL) with 10 age-matched healthy controls. Interestingly, the responses to BNP in chronic HF patients were significantly reduced to about one third of those seen in healthy controls, whereas the vasodilator capacity and nitric oxide signaling were not affected to the same extent as BNP-mediated dilation, indicating a possible downregulation of BNP receptor function in the elderly HF patients. Another study by Jensen,.[29]compared prognostic value of NT-proBNP/BNP ratio with NT-proBNP or BNP alone in a 2-year follow-up of 189 elderly chronic HF patients [72 ± 11 years old, male 52%, left ventricular ejection fraction (LVEF) 46 ± 14%]. They found that NT-proBNP/BNP ratio provided no additional prognostic information as compared to NT-proBNP or BNP alone in these HF patients. The cut-off values are NT-proBNP > 800 pg/mL, BNP > 60 pg/mL, and NT-proBNP/BNP ratio > 6.4 respectively. If NT-proBNP serum level is above 2000 pg/mL, it indicates poor prognosis. Similarly for BNP, as long as its serum level is above 100 pg/mL, it indicates poor prognosis. There was a significant correlation between survival and NT-proBNP, BNP and Cystatin-C but not with NT-pro BNP/BNP ratio.
Most recently, a retrospective study by Jia,.[30]demonstrated a prediction model of in-hospital mortality in elderly Chinese patients with acute HF. A total of 2486 patients (> 60 years old from cardiac intensive care units) were analyzed with binary logistic regression method. The identified heart rate [odds ratios (OR): 1.043,< 0.001], LVEF (OR: 0.918, 95%,< 0.001), pH value (OR: 0.001, 95%,< 0.001), renal dysfunction (OR: 0.120,< 0.001) and NT-proBNP (OR: 3.463,< 0.001) as the independent risk factors of in-hospital mortality for elderly acute HF patients and provided a risk prediction model for in-hospital mortality in elderly patients with acute HF.[30]
9 Future perspectives
As summarized in Figure 1, we are likely at a breakthrough crossroad in connecting the past and present knowledges on the biomarker and therapeutic roles of natriuretic peptides into the future directions that may significantly advance these important applications in cardiovascular medicine. The recognition and development of HF biomarkers can be divided into 2 phases. The Phase I is technical efficacy and diagnostic accuracy and the Phase II is therapeutic efficacy and patient outcome.[2]With the devel- opment of clinical examination techniques, the current cardiology practice has advanced from the Phase I to the Phase II and towards a goal for biomarker-guided therapy. Thus, since enhancement of BNP level has emerged as an important treatment strategy of HF, it is very important to accurately detect the concentration of circulating BNP, NEP, sNEP, NEP substrates and recognize the dual role of biotarget and biomarker for these BNP-related peptides.[31]Furthermore, the new concept of “Designer Natriuretic Peptides (DNPs)” has resulted from novel peptide engineering, in which strategic modifications in peptide molecular sequences are employed. The rationale behind this concept is to produce chimeric natriuretic peptides whose pharmacological and beneficial biological profiles go beyond those of native natriuretic peptides while minimizing undesirable effects. Another goal would be to engineer DNPs that are highly resistant to NEP and can be administered subcutaneously and orally. Taken together, we hope that these practical discussions on natriuretic peptide family may be instrumental for the healthcare providers in critically interpreting laboratory results and effective management of the HF patients.
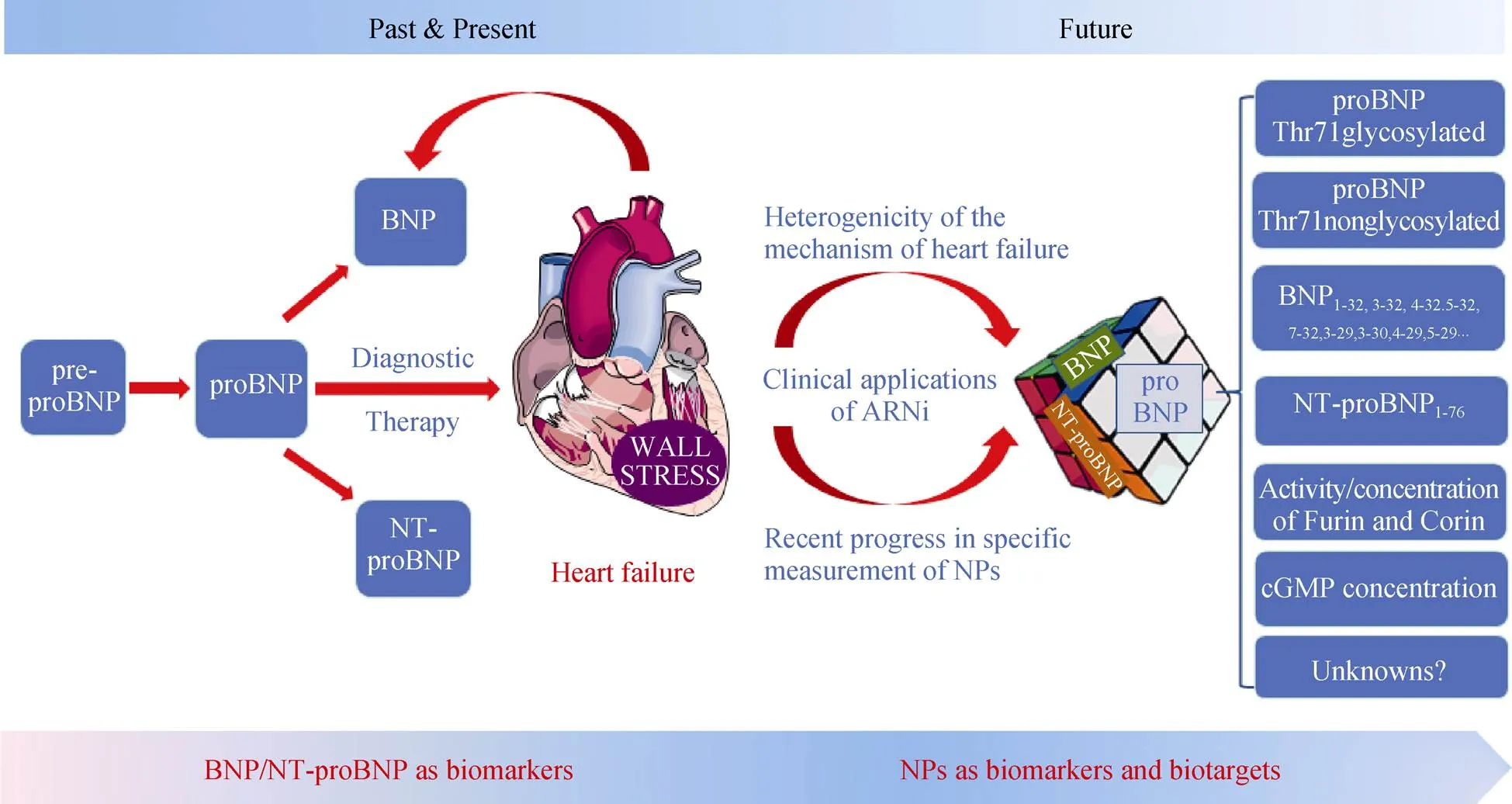
Figure 1. Schematic summary of the current opinions on the biomarker roles and therapeutic potentials of natriuretic peptide family and the future directions of research and clinical applications. ARNi: Angiotensin receptor-neprilysin inhibitor; BNP: B-type natriuretic peptide; cGMP: cyclic guanosine monophosphate; NPs: natriuretic peptides; NT-proBNP: N-terminal proBNP; pre-proBNP: precursor protein of proBNP.
1 Xi L, Kouvelos G, Paolocci N. Circulating biomarkers for cardiovascular diseases: the beats never stop.2018; 39: 1065–1067.
2 Tunis SR, Messner DA. Payer perspectives on coverage of biomarker testing in cardiovascular disease.2017; 63: 258–260.
3 Li XF, Pan D, Zhang WL,. Association of NT-proBNP and interleukin-17 levels with heart failure in elderly patients.2016; 15.
4 Bombelli M, Maloberti A, Rossi S,. Clinical value of NT-proBNP assay in the emergency department for the diagnosis of heart failure (HF) in very elderly people.2015; 61: 296–300.
5 Lelli D, Pedone C, Rossi FF,. Clinical and echocar-dio-graphic characteristics of elderly hospitalized patients with high levels of NT-proBNP without clinical diagnosis of heart failure.2014; 26: 607–613.
6 Sitar Taut AV, Pop D, Zdrenghea DT. NT-proBNP values in elderly heart failure patients with atrial fibrillation and diabetes.2015; 29: 1119–1123.
7 Choudhary R, Gopal D, Kipper BA,. Cardiorenal bio-markers in acute heart failure.2012; 9: 292–304.
8 Gandhi PU, Testani JM, Ahmad T. The current and potential clinical relevance of heart failure biomarkers.2015; 12: 318–327.
9 Yancy CW, Jessup M, Bozkurt B,. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.2013; 62: e147–e239.
10 van Kimmenade RR, Januzzi JL Jr. Emerging biomarkers in heart failure.2012; 58: 127–138.
11 Ibrahim NE, Januzzi JL Jr. Beyond natriuretic peptides for diagnosis and management of heart failure.2017; 63: 211–222.
12 Sharma A, Felker GM. Brain natriuretic peptide treatment and heart failure prevention: reliving the mistakes of the past or charting a new course for the future?2016; 4: 548–550.
13 Clerico A, Franzini M, Masotti S,. State of the art of immunoassay methods for B-type natriuretic peptides: An update.2015; 52: 56–69.
14 Suzuki T, Israr MZ, Heaney LM,. Prognostic role of molecular forms of B-Type natriuretic peptide in acute heart failure.2017; 63: 880–886.
15 Saenger AK, Rodriguez-Fraga O, Ler R,. Specificity of B-Type natriuretic peptide assays: cross-reactivity with different BNP, NT-proBNP, and proBNP peptides.2017; 63: 351–358.
16 Gommans DH, Bayes-Genis A, van Kimmenade RR. Putting together the pieces of the natriuretic peptide puzzle.2016; 4: 670–673.
17 Yu P, Hong K. [Research advances on the relationship between O-linked N-acetylglucosamine and cardiovascular diseases].2016; 44: 271–274. [Article in Chinese].
18 Halfinger B, Hammerer-Lercher A, Amplatz B,. Unra-veling the molecular complexity of O-Glycosylated Endo-genous (N-Terminal) pro-B-Type natriuretic peptide forms in blood plasma of patients with severe heart failure.2017; 63: 359–368.
19 Vodovar N, Seronde MF, Laribi S,. Post-translational modifications enhance NT-proBNP and BNP production in acute decompensated heart failure.2014; 35: 3434–3441.
20 Seferian KR, Tamm NN, Semenov AG,. Immuno-de-tection of glycosylated NT-proBNP circulating in human blood.2008; 54: 866–873.
21 Chen Y, Burnett JC Jr. Biochemistry, therapeutics, and bio-marker implications of neprilysin in cardiorenal disease.2017; 63: 108–115.
22 Feldman AM. Neprilysin inhibition in the time of precision medicine.2016; 4: 409-414.
23 Vodovar N, Seronde MF, Laribi S,. Elevated plasma B-Type natriuretic peptide concentrations directly inhibit circulating neprilysin activity in heart failure.2015; 3: 629–636.
24 Jhund PS, Claggett B, Packer M,. Independence of the blood pressure lowering effect and efficacy of the angiotensin receptor neprilysin inhibitor, LCZ696, in patients with heart failure with preserved ejection fraction: an analysis of the PARAMOUNT trial.2014; 16: 671–677.
25 Wannamethee SG, Welsh P, Whincup PH,. N-terminal pro brain natriuretic peptide but not copeptin improves prediction of heart failure over other routine clinical risk parameters in older men with and without cardiovascular disease: population-based study.2014; 16: 25–32.
26 Mureddu GF, Agabiti N, Rizzello V,. Prevalence of preclinical and clinical heart failure in the elderly. A population-based study in Central Italy.2012; 14: 718–729.
27 Su Q, Liu H, Zhang X,. Diagnostic values of NT- proBNP in acute dyspnea among elderly patients.2015; 8: 13471–13476.
28 Edvinsson ML, Uddman E, Edvinsson L,. Brain natriuretic peptide is a potent vasodilator in aged human microcirculation and shows a blunted response in heart failure patients.2014; 11: 50–56.
29 Jensen J, Ma LP, Bjurman C,. Prognostic values of NTpro BNP/BNP ratio in comparison with NTpro BNP or BNP alone in elderly patients with chronic heart failure in a 2-year follow up.2012; 155: 1–5.
30 Jia Q, Wang YR, He P,. Prediction model of in-hospital mortality in elderly patients with acute heart failure based on retrospective study.2017; 14: 669–678.
31 Seronde MF, Mebazaa A. Neprilysin: biotarget and biomarker in heart failure.2015; 3: 645–646.
Zhen–Lu Zhang, Department of Clinical Laboratory, Wuhan Asia Heart Hospital of Wuhan University, Wuhan, China (ZHANG ZL) & Lei Xi, Pauley Heart Center, Virginia Commonwealth University, Richmond, VA 23298–0204, UnitedStates (XI L). E-mails: zhenluzhangwh@163.com (ZHANG ZL) & lxi@vcu.edu (XI L)
July 11, 2018
August 14, 2018
August 14, 2018
August 28, 2018
 Journal of Geriatric Cardiology2018年8期
Journal of Geriatric Cardiology2018年8期
- Journal of Geriatric Cardiology的其它文章
- Rare combination of dilated cardiomyopathy and ankylosing spondylitis in a family
- Patent foramen ovale in an old patient with ischemic stroke following carotid surgery
- Normalization of plasma growth hormone alleviated malignant ventricular tachycardia in acromegaly
- Subclinical hypothyroidism is associated with lipid-rich plaques in patients with coronary artery disease as assessed by optical coherence tomography
- Five-year major clinical outcomes between first-generation and second- generation drug-eluting stents in acute myocardial infarction patients underwent percutaneous coronary intervention
- Correction of hypovitaminosis D improved global longitudinal strain earlier than left ventricular ejection fraction in cardiovascular older adults after orthopaedic surgery
