Effects of lung protective ventilation on pulmonary function,inflammation, and oxidative stress in patients undergoing craniotomy: study protocol for a multi-center, randomized,parallel, controlled trial
Chao-liang Tang, Juan Li, Bo Zhao Jia-bao Hou Zhong-yuan Xia
1 Department of Anesthesiology, Renmin Hospital of Wuhan University, Wuhan, Hubei Province, China
2 Department of Anesthesiology, Anhui Provincial Hospital (Southern District), Hefei, Anhui Province, China
BACKGROUND
Mechanical ventilation is the most effective means of providing respiratory support in critically ill patients. Annually approximately 2.5 million patients rely on mechanical ventilation during surgery (Weiser et al., 2008). General anesthesia can cause changes in lung tissue structure and diaphragm position, and inappropriate ventilator settings are likely to cause air pressure injury and atelectasis, leading to postoperative in flammation (Duggan and Kavanagh, 2005;Brueckmann et al., 2013). General anesthesia complicated by surgical trauma can also lead to postoperative local,and even systemic, in flammatory responses and pulmonary complications (The Acute Respiratory Distress Syndrome Network, 1999, 2000; Bouadma et al., 2004, 2007; Gajic et al., 2004; Hess, 2011). A lung protective ventilation strategy has recently been developed to reduce ventilatorassociated lung tissue injury and simultaneously improve systemic oxygenation (Schilling et al., 2005). Lung protective ventilation regulates positive end-expiratory pressure(PEEP), maintains more pulmonary alveoli in an open state(i.e., to maintain end-expiratory lung volumes), avoids elevated end-expiratory lung volume, maintains targeted tidal volumes, and alleviates the injury caused by elevated lung volume and abnormal tidal volumes (Schilling et al.,2005). PEEP can prevent the collapse of open pulmonary alveoli (Lachmann, 1992), maintain lung volume and the function of pulmonary surfactants, and reduce the shear stress caused by repeated/loss of alveolar or bronchiolar recruitment(s). High tidal volume ventilation maintains the partial pressure of oxygen in arterial blood (PaO2) at normal levels, but it can cause excessive expansion of the lung with normal oxygenation. In 1993, mechanical ventilation with low tidal volumes was recommended (Slutsky, 1993). Lung protective ventilation has been widely used in the clinic,particularly in one-lung ventilation and abdominal surgeries.We searched PubMed for relevant articles published in the past 3 years and three original research articles regarding the use of lung protective ventilation in abdominal and pulmonary surgeries were retrieved (Table 1). No articles about the use of lung protective ventilation in craniocerebral surgeries were retrieved. Only three similar trials have been registered in ClinicalTrials.gov, but no conclusions have been obtained (Table 2).
There is evidence that mechanical ventilation of the healthy lung can induce up-regulation of cytokines, leading to pre-in flammatory cytokine gene transcription, predisposing the organism to infection and oxidative stress (Brégeon et al., 2002). This study protocol has been designed to investigate the safety of a lung protective ventilation strategy with low tidal volume and PEEP on respiratory status,postoperative pulmonary and systematic in flammation, and oxidative stress in patients undergoing craniotomy.
METHODS/DESIGN
Study design
A multi-center, randomized, parallel, controlled trial.
Study setting
Anhui Provincial Hospital (Southern District) and Renmin Hospital of Wuhan University, China.
Study procedure
Sixty eligible patients scheduled to undergo craniotomy will be randomly allocated to undergo either lung protec-tive ventilation (6 mL/kg tidal volume, 10 cmH2O PEEP,respiratory frequency 15 breaths/min; n = 30) or conventional mechanical ventilation (10 mL/kg tidal volume,respiratory frequency 12 breaths/min; n = 30). All patients will be evaluated from just prior to changing the ventilation mode before surgery until immediately after extubation. The primary outcome measure will be dynamic lung compliance, an index used to evaluate the degree of pulmonary function impairment. The secondary outcome measures will be respiratory index, mean airway pressure (Pmean), plateau pressure (Pplat), alveolar and plasma markers of in flammation and oxidative stress. The planned flow of participants through the trial is shown in Figure 1.
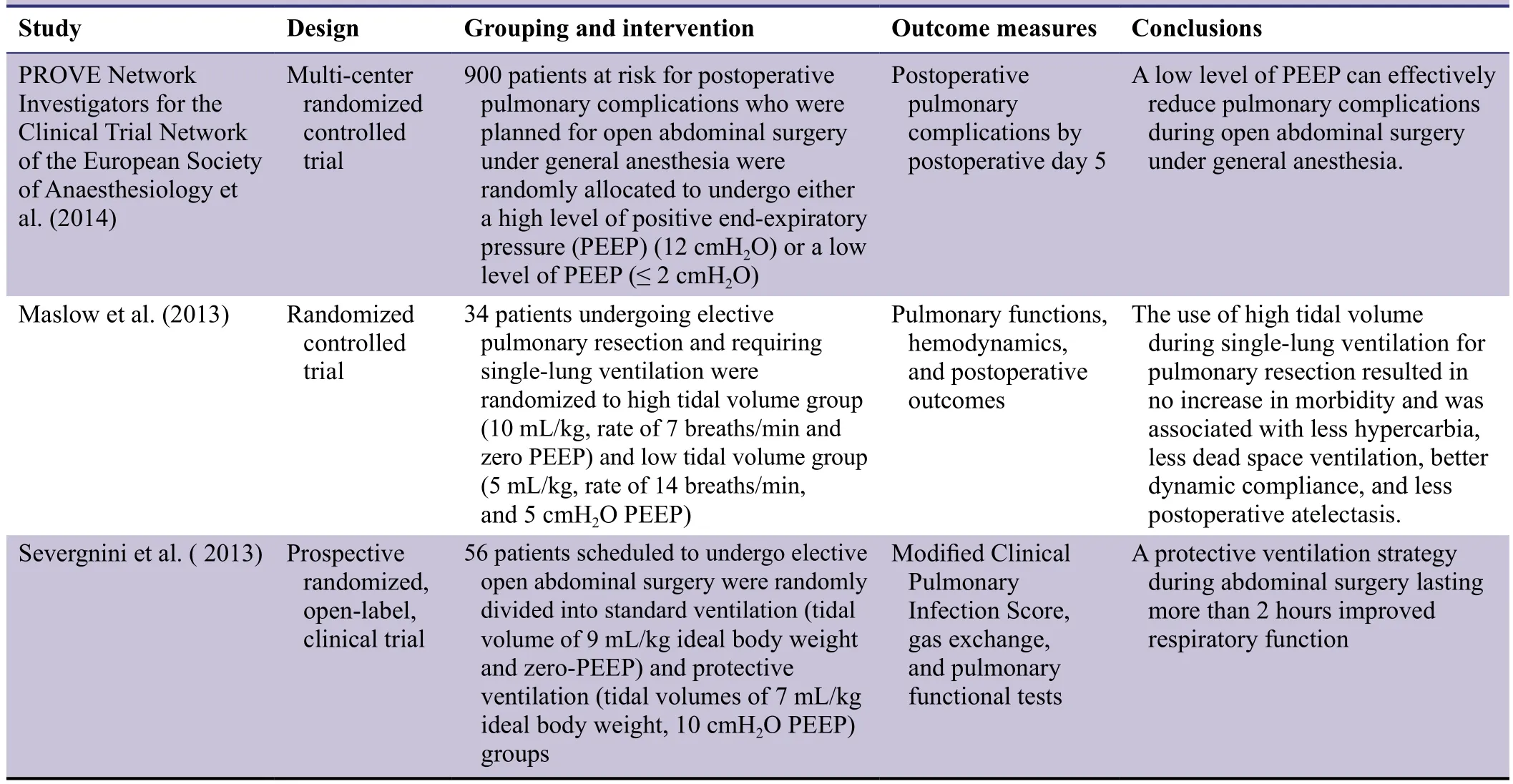
Table 1: Previous studies of lung protective ventilation in clinical surgeries
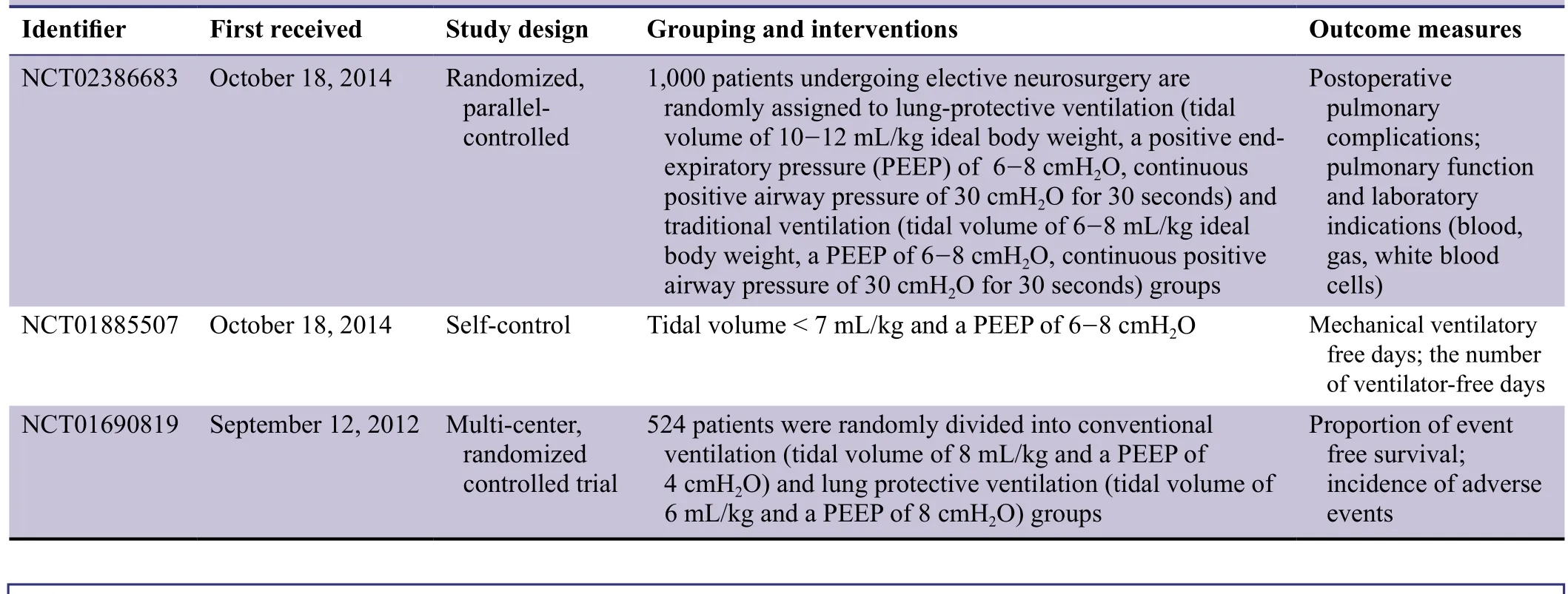
Table 2: Studies, registered in ClinicalTrials.gov, regarding the lung protective ventilation in brain injuries

Figure 1: Flow chart of the trial protocol.
Study participants
Patients scheduled to undergo craniotomy at Anhui Provincial Hospital (Southern District) or Renmin Hospital of Wuhan University, China.
Inclusion criteria
Patients meeting all the following criteria will be considered for admission to the trial:
· Scheduled to undergo craniotomy following CT/MRI examination
· American Society of Anesthesiologists (ASA) Physical Status Scale class I- II (Fitz-Henry, 2011)
· Body mass index 18.5-30 kg/m2
· Normal pre-operative pulmonary function
· Age 18-70 years
Exclusion criteria
Patients with any of the following will be excluded from the trial:
· Bronchial infection
· Severe hypertension or cardiovascular disease
· Liver and kidney dysfunction
Withdrawal criteria
Patients will be withdrawn from the trial under any of the following circumstances:
· Disease aggravation during anesthesia
· Complications or comorbidities likely to in fluence the curative effect evaluation or any safety concerns
Sample size
According to previous studies (Jiao and Cai, 2007; Chen et al., 2013; Wang et al., 2015), the effective sample was determined to be n = 30 per group. Outcomes will be analyzed in accordance with the intention-to-treat principle.
Recruitment
Potential patients from the wards and clinics in Anhui Provincial Hospital (Southern District) and Renmin Hospital of Wuhan University, China will be recruited into this study.After receiving written informed consent from patients or their relatives, each patient will be screened according to the inclusion and exclusion criteria above.
Grouping
A cohort of 60 patients will be assigned to either the protective ventilation group or conventional mechanical ventilation group. Group allocation will be blinded to patients and outcome assessors.
Interventions
All patients will have preoperative preparation 60 minutes before surgery. Prior to anesthesia, blood oxygen saturation(SpO2), non-invasive blood pressure and electrocardiogram measurements, followed by intravenous administration of 10-15 mL/kg Ringer lactate solution, will be performed. Each patient’s heart rate and mean arterial pressure will be monitored through the use of multi-parameter monitors(Philips HP50, the Netherlands) and radial arterial puncture for arterial blood gas analysis will be performed. Intravenous sufentanil (0.4 μg/kg), vecuronium bromide (0.12 mg/kg) and etomidate (0.2 mg/kg) will be administered to facilitate tracheal intubation for mechanical ventilation. Intravenous sufentanil (Cp 3-4 ng/mL), vecuronium bromide (4 mg/h),sevo flurane (1.0%) and propofol (Cp 3-4 μg/mL) will be used to maintain anesthesia and muscle relaxation.
The brain surgery required will be performed on each patient, while maintaining the following ventilation conditions:
Protective ventilation: 6 mL/kg tidal volume, 10 cmH2O PEEP, and respiratory frequency 15 breaths/min.
Conventional mechanical ventilation: 10 mL/kg tidal volume and respiratory frequency 12 breaths/min.
Outcome measures
Primary outcomes
Dynamic lung compliance will be evaluated from just prior to changing the ventilation mode to immediately after extubation. Dynamic lung compliance is de fined as a change in lung volume at de fined units of transpulmonary pressure. It is an important parameter used to evaluate alveolar ventilation ef ficacy and pulmonary function impairment as it re flects the degree of dif ficulty in pulmonary expansion under unit pressure and generally re flects lung tissue elasticity (Dixon et al., 1979). Dynamic lung compliance = tidal volume/Pplat.
Secondary outcomes
The following outcomes will be assessed throughout the procedure, from just prior to changing the ventilation mode before surgery, until immediately after extubation:
(1) Respiratory index: This re flects pulmonary ventilation and oxygen exchange function (Sganga et al., 1985;Hodgkins et al., 1990). Respiratory index = alveolar-arterial oxygen tension difference (PA-aDO2)/arterial PaO2. PA-aDO2= 713 × FiO2- 1.25 × PaCO2- PaO2. FiO2is inhaled oxygen concentration.
(2) Pmean: This reveals the mean airway pressure during the entire respiratory cycle that indirectly indicates the mean alveolar pressure (Luecke et al., 2003). The effects of ventilation methods on hemodynamics and gas exchange are closely related to the occurrence of air pressure injury.
(3) Pplat: This reveals the airway pressure measured after a 0.5-second pause at the end of inspiration (inspiratory and expiratory valves closed, gas flow rate of 0 (L/min) and it is closely related to alveolar peak pressure (Kallet, 2005).The following will be assessed just prior to changing the ventilation mode, and then again immediately following extubation:
(4) Alveolar and plasma markers of in flammation including tumor necrosis factor-alpha (TNF-α), interleukin (IL)-6, -8,and -10 (Bhatia and Moochhala, 2004; Wilson et al., 2005;Shen et al., 2011; Lederer et al., 2013; Hiroshima et al., 2014;Wang et al., 2014). A fiber optic bronchoscope will be placed as far as possible into the trachea. After a continuous drip infusion of 20 mL of physiological saline, bronchoalveolar lavage fluid will be collected, and then centrifuged at 200× g for 10 minutes. The supernatant and 3 mL of peripheral venous blood will be preserved at -80°C for later detection of TNF-α, IL-6, -8, and -10 levels by ELISA method.
(5) Alveolar and plasma markers of oxidative stress:Malondialdehyde and superoxide dismutase will be detected by colorimetric assays (Lu et al., 2015; Tsikas et al., 2016).
Other outcomes
Heart rate, mean arterial pressure, duration of surgery,duration of ventilation, and adverse events will be monitored from the time of change of ventilation mode to after extubation.Patient’s baseline data and the timing for outcome assessments are shown in Tables 3 and 4, respectively.
Data collection, management, analysis, and open accesss
Data collection
Case report forms with accurate, complete and timely filled data will be reported by the clinical researchers. The original paper forms will be preserved. To ensure the validity of the data, the date of, and the time taken for, form completion will be provided. The data manager will be responsible for the data input and management. The data will be recorded in an electronic database using a double-data entry strategy by two data managers and collated. The case report forms will be completed by the researchers and the data managers will modify the data according to the researchers’ responses.A modi fied question form will be generated by the data managers if necessary.
Data management
Following blinded peer review, the electronic database will be locked by the researchers in charge and statisticians, and will not be altered. Paper and electronic data regarding screening,informed consent, and clinical outcomes will be preserved at each study center. After completion of the study, the original data will be preserved in the lead center and copies of the data stored at each center. All paper-based data will be permanently preserved.
Data analysis
The electronic database will be made available to a professional statistician for statistical analysis. An outcome analysis report will be made by the statistician and submitted to the lead researchers.
Data open access
Anonymized trial data will be published at http://www.figshare.com.
Statistical analysis
All data will be analyzed using SPSS 11.0 software (SPSS,Chicago, IL, USA). Baseline information will be evaluated using Fisher’s exact test. Normally distributed data will be expressed as the mean ± SD. Paired t-tests will be used for comparisons between groups, and repeated measures analysis of variance for comparisons between different time points in the same group. Non-normally distributed data will be expressed as medians (interquartile range) [M(IQR)].The Mann Whitney U test will be used for comparisons between two groups and the Wilcoxon signed-rank test for comparisons between different time points in the same group. The chi-square test will be used to compare numeration data between the groups. A level of P < 0.05 will beconsidered statistically signi ficant.
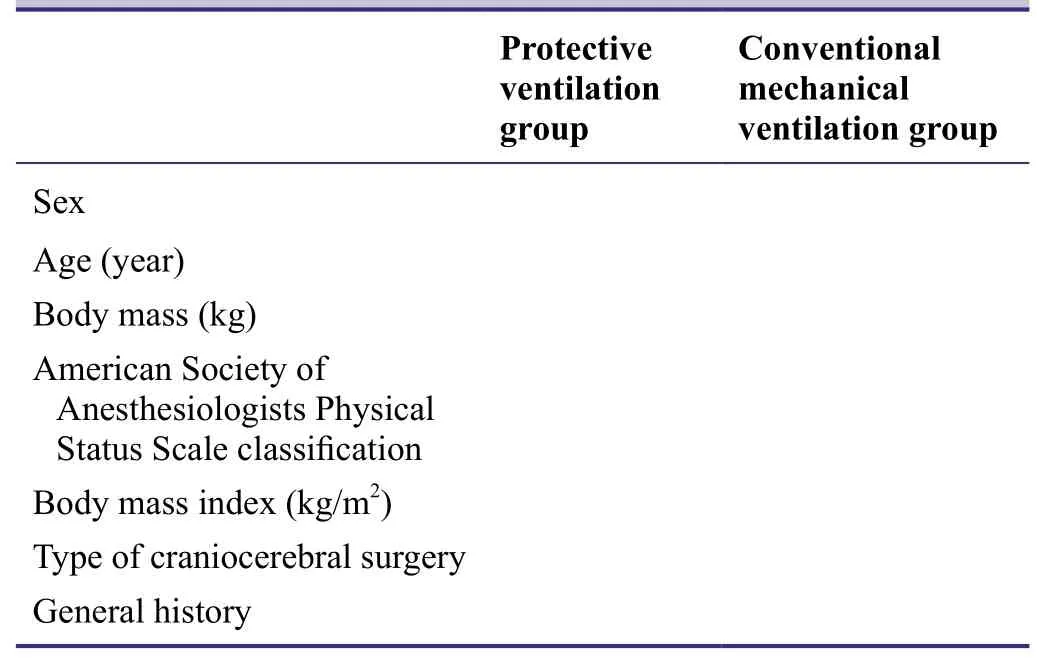
Table 3: Baseline information of included patients
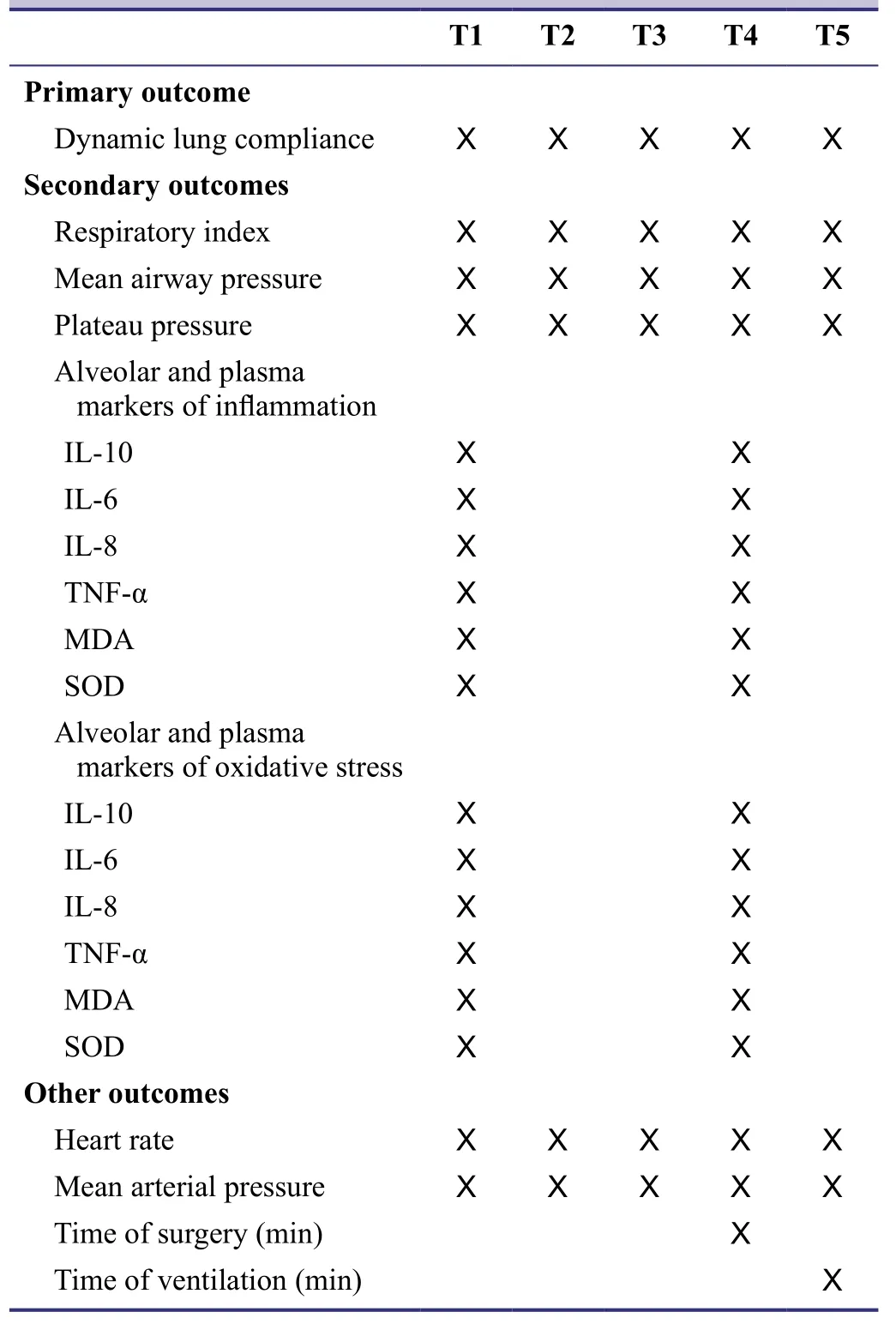
Table 4: Timing of outcome assessment
Auditing
Trial progression will be reported to the ethics committee of Anhui Provincial Hospital (Southern District), China every 6 months and the trial’s status will be updated at Chinese Clinical Trial Registry.
Confidentiality
Any data provided by the sponsors, including protocol design, performance, outcomes, case report forms, and informed consent will be preserved in secure, locked facilities and not disclosed to any non-authorized people.
DISCUSSION
In this study, we will elucidate the safety of lung protective ventilation strategy used in craniocerebral surgeries by investigating dynamic lung compliance, respiratory index,Pmean, Pplat, alveolar and plasma markers of in flammation, and oxidative stress. Because of the small sample size, a large age range, both sexes, short observation times, limited precision of measuring instrument, differences in craniocerebral surgery type and duration of surgery, and other indices, such as intrapulmonary shunt rate, will be not monitored in this study. Some uncertainties, such as the precise ventilation parameters and individualized lung ventilation protocols,will be investigated in future studies aiming to determine the optimal lung protective ventilation strategy.
Trial status
Recruitment of participants is ongoing at the time of submission.
Conflicts of interest
None declared.
Author contributions
CLT, JL and ZYX conceive and design the protocol. CLT,BZ and JBH are responsible for data collection. All authors approve the final version of this manuscript for publication.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
Bhatia M, Moochhala S (2004) Role of in flammatory mediators in the pathophysiology of acute respiratory distress syndrome. J Pathol 202:145-156.
Bouadma L, Dreyfuss D, Ricard JD, Martet G, Saumon G (2007)Mechanical ventilation and hemorrhagic shock-resuscitation interact to increase in flammatory cytokine release in rats. Crit Care Med 35:2601-2606.
Bouadma L, Schortgen F, Ricard JD, Martet G, Dreyfuss D, Saumon G (2004) Ventilation strategy affects cytokine release after mesenteric ischemia-reperfusion in rats. Crit Care Med 32:1563-1569.
Brégeon F, Roch A, Delpierre S, Ghigo E, Autillo-Touati A, Kajikawa O, Martin TR, Pugin J, Portugal H, Auffray JP, Jammes Y (2002) Conventional mechanical ventilation of healthy lungs induced pro-in flammatory cytokine gene transcription. Respir Physiol Neurobiol 132:191-203.
Brueckmann B, Villa-Uribe JL, Bateman BT, Grosse-Sundrup M,Hess DR, Schlett CL, Eikermann M (2013) Development and validation of a score for prediction of postoperative respiratory complications. Anesthesiology 118:1276-1285.
Chen XS, Fang JJ, Wang R, Gu LB (2013) The impact of different levels of low tidal volume ventilation on high pressure on traumatic brain injury induced ARDS. Zhongguo Xiandai Yisheng 51:22-23, 26.
Dixon M, Jackson DM, Richards IM (1979) The effects of H1- and H2-receptor agonists and antagonists on total lung resistance,dynamic lung compliance and irritant receptor discharge in the anaesthetized dog. Br J Pharmacol 66:203-209.
Duggan M, Kavanagh BP (2005) Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 102:838-854.
Fitz-Henry J (2011) The ASA classi fication and peri-operative risk.Ann R Coll Surg Engl 93:185-187.
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM,Rana R, St Sauver JL, Lymp JF, Afessa B, Hubmayr RD (2004)Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 32:1817-1824.
Hess DR (2011) Approaches to conventional mechanical ventilation of the patient with acute respiratory distress syndrome. Respir Care 56:1555-1572.
Hiroshima Y, Hsu K, Tedla N, Chung YM, Chow S, Herbert C, Geczy CL (2014) S100A8 induces IL-10 and protects against acute lung lnjury. J Immunol 192:2800-2811.
Hodgkins P, Chadha D, Iles P, B. (1990) The respiratory index as a prognostic measure of lung damage. Hum Exp Toxicol 9:109-110.
Jiao HN, Cai HW (2007) Effect of mechanical ventilation with different tidal volumes on the respiratory function during general anesthesia. Zhongnan Daxue Xuebao: Yixue Ban 32:706-709.
Kallet RH (2015) The complexity of interpreting plateau pressure in ARDS. Respir Care 60:147-149.
Lachmann B (1992) Open up the lung and keep the lung open. Intensive Care Med 18:318-321.
Lederer W, Stichlberger M, Hausdorfer J, Fuchs D, Mutz NJ, Wiedermann FJ (2013) Alveolar neopterin, procalcitonin, and IL-6 in relation to serum levels and severity of lung injury in ARDS. Clin Chem Lab Med 51:e213-215.
Lu X, Wang C, Liu B (2015) The role of Cu/Zn-SOD and Mn-SOD in the immune response to oxidative stress and pathogen challenge in the clam Meretrix meretrix. Fish Shell fish Immunol 42:58-65.
Luecke T, Meinhardt JP, Herrmann P, Weisser G, Pelosi P, Quintel M (2003) Setting mean airway pressure during high-frequency oscillatory ventilation according to the static pressure--volume curve in surfactant-de ficient lung injury: a computed tomography study. Anesthesiology 99:1313-1322.
Maslow AD, Stafford TS, Davignon KR, Ng T (2013) A randomized comparison of different ventilator strategies during thoracotomy for pulmonary resection. J Thorac Cardiovasc Surg 146:38-44.
PROVE Network Investigators for the Clinical Trial Network of the European Society of Anaesthesiology, Hemmes SN, Gama de Abreu M, Pelosi P, Schultz MJ (2014) High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet 384:495-503.
Schilling T, Kozian A, Huth C, Bühling F, Kretzschmar M, Welte T,Hachenberg T (2005) The pulmonary immune effects of mechanical ventilation in patients undergoing thoracic surgery. Anesth Analg 101:957-965.
Severgnini P, Selmo G, Lanza C, Chiesa A, Frigerio A, Bacuzzi A,Dionigi G, Novario R, Gregoretti C, de Abreu MG, Schultz MJ,Jaber S, Futier E, Chiaranda M, Pelosi P (2013) Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology 118:1307-1321.
Sganga G, Siegel JH, Coleman B, Giovannini I, Boldrini G, Pittiruti M (1985) The physiologic meaning of the respiratory index in various types of critical illness. Circ Shock 17:179-193.
Shen Y, Wang D, Wang X (2011) Role of CCR2 and IL-8 in acute lung injury: a new mechanism and therapeutic target. Expert Rev Respir Med 5:107-114.
Slutsky AS (1993) Mechanical ventilation. Chest 104:1833-1859.
The Acute Respiratory Distress Syndrome Network (1999) International consensus conferences in intensive care medicine: Ventilator-associated Lung Injury in ARDS. This of ficial conference report was cosponsored by the American Thoracic Society, The European Society of Intensive Care Medicine, and The Societé de Réanimation de Langue Fran?aise, and was approved by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 160:2118-2124.
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301-1308.
Tsikas D, Rothmann S, Schneider JY, Suchy MT, Trettin A, Modun D, Stuke N, Maassen N, Fr?lich JC (2016) Development, validation and biomedical applications of stable-isotope dilution GCMS and GC-MS/MS techniques for circulating malondialdehyde(MDA) after penta fluorobenzyl bromide derivatization: MDA as a biomarker of oxidative stress and its relation to 15(S)-8-isoprostaglandin F2α and nitric oxide (NO). J Chromatogr B Analyt Technol Biomed Life Sci 1019:95-111.
Wang R, Li J, Kang F, Niu CS (2015) Application of low tidal volume ventilation strategy in patients under going craniotomy. Liti Dingxiang he Gongnengxing Shenjing Waike Zazhi 28:87-90.
Wang Y, Ji M, Wang LE, Chen L, Li J (2014) Xuebijing injection improves the respiratory function in rabbits with oleic acid-induced acute lung injury by inhibiting IL-6 expression and promoting IL-10 expression at the protein and mRNA levels. Exp Ther Med 8:1593-1598.
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR, Gawande AA (2008) An estimation of the global volume of surgery: a modelling strategy based on available data.Lancet 372:139-144.
Wilson MR, Choudhury S, Takata M (2005) Pulmonary in flammation induced by high-stretch ventilation is mediated by tumor necrosis factor signaling in mice. Am J Physiol Lung Cell Mol Physiol 288:L599-607.
 Asia Pacific Journal of Clinical Trials:Nervous System Diseases2016年3期
Asia Pacific Journal of Clinical Trials:Nervous System Diseases2016年3期
- Asia Pacific Journal of Clinical Trials:Nervous System Diseases的其它文章
- Evaluation of cardiac autonomic status using QTc interval in patients with leprosy
- Efficacy of spontaneous laughter in the post-operative treatment of pain and anxiety in children: study protocol for a randomized controlled trial
- Effect of pre-incisional anterior scalp block on intraoperative opioid consumption in adult patients undergoing elective craniotomy to remove tumor: study protocol for a randomized double-blind trial
- Effects of cognitive behavioral therapy on white matter fibers of patients with obsessive-compulsive disorder as assessed by diffusion tensor imaging: study protocol for a parallel group,controlled trial
- Migraine prevention by noninvasive electrical fastigial nucleus stimulation: a multi-center, randomized, double-blind,sham-controlled trial
- Scalp acupuncture twisting manipulation for treatment of hemiplegia after acute ischemic stroke in patients: study protocol for a randomized, parallel, controlled, single-blind trial
