Effects of cognitive behavioral therapy on white matter fibers of patients with obsessive-compulsive disorder as assessed by diffusion tensor imaging: study protocol for a parallel group,controlled trial
Xiang-yun Yang, Jia Luo, Jing Liu, Yun Ma, Zhi-hua Guo, Xiao-jie Yang, Zhan-jiang Li,
1 Department of Clinical Psychology, Beijing Key Lab of Mental Disorders, Beijing Anding Hospital, Capital Medical University, and Center of Schizophrenia, Beijing Institute for Brain Disorders, Beijing, China
2 Department of Psychiatry, Qiqihaer Medical University, Qiqihaer, Heilongjiang Province, China
BACKGROUND
Obsessive-compulsive disorder (OCD) is a common,chronic, costly, long-lasting, and disabling disorder, with a lifetime prevalence of 2-3% (Kessler et al., 2005; Goodman et al., 2014). OCD patients often have forced or compulsive behavior, which seriously affects their normalwork, learning, and social interactions. It is estimated by the World Health Organization (2008) that in 2020 OCD-caused disease will be the fourth most common mental illness burden in China.
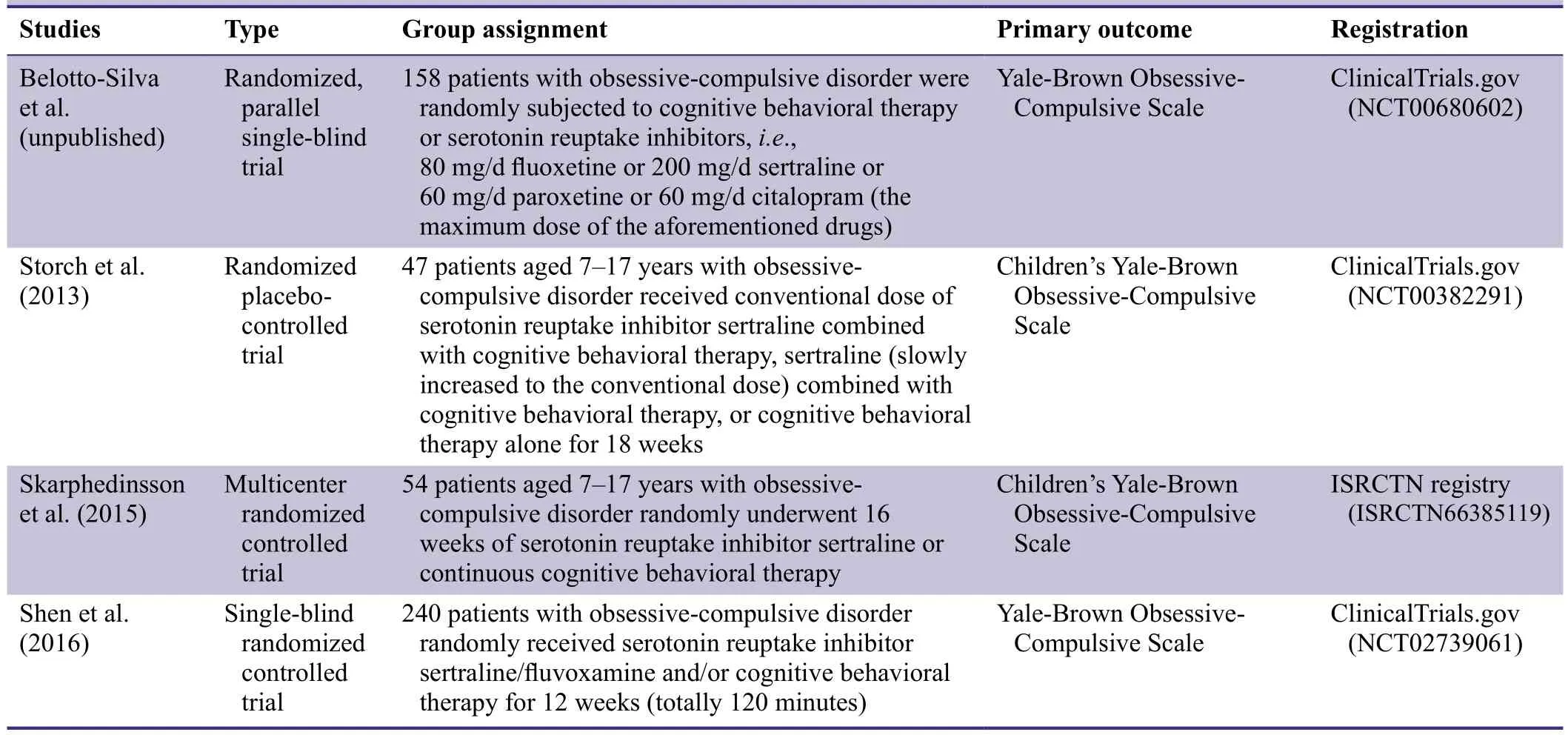
Table 1: Previous clinical studies investigating cognitive behavioral therapy for obsessive-compulsive disorder
Serotonin reuptake inhibitors and cognitive behavioral therapy are the main treatments for OCD. Serotonin reuptake inhibitors work quickly to alleviate the symptoms of OCD, but 40-60% of OCD patients still have some residual symptoms (Luo et al., 2010; Luo and Li, 2010). Li et al.(2004) suggested that OCD is associated with personality characteristics, and psychological and social factors.Short-duration cognitive behavioral therapy is currently recognized as an effective treatment method (Bolton and Perrin, 2008) with a remission rate of 58-76% (Whittal et al., 2005). Previous clinical studies have paid much attention to the effectiveness of behavioral therapy (Table 1).
The neural mechanisms underlying the effectiveness of cognitive behavioral therapy in treating OCD remain unclear. This leaves some uncertainty in the choice of individual cognitive behavioral therapy for OCD patients.Neuroimaging studies have found changes in cerebral function in OCD patients before and after cognitive behavioral therapy (Nakao et al., 2005; Apostolova et al.,2010; Freyer et al., 2011).
Functional and structural damage has been shown in the frontal-striatal-thalamic circuits, including the prefrontal cortex, anterior cingutate cortex, dorsolateral prefrontal cortex, caudate nucleus, and thalamus (Cannistraro et al.,2007; Menzies et al., 2008; Saito et al., 2008; Garibotto et al., 2010; Fontenelle et al., 2011; Li et al., 2011; Nakamae et al., 2011; Zarei et al., 2011). These cortical and subcortical tissues are connected by white matter fibers, suggesting that the microstructure of white matter fiber bundles is altered in OCD patients. These alterations can enhance information transfer between brain structures leading to dysfunction in these brain regions, such as compulsive behavior or uncontrollable thoughts (Lim and Helpern, 2002). Cognitive behavioral therapy can alter the functions of many brain regions and tissues in OCD patients, resulting in an improvement in symptoms. Because the regions affected are connected by white matter fibers, we hypothesize that cognitive behavioral therapy restores white matter fiber connections in frontal-striatal-thalamic circuits. This in turn in fluences the recovery of functions and structures,and improves compulsive behavior and thinking in OCD patients.
OBJECTIVE
This trial is designed to assess the changes in white matter fibers in OCD patients undergoing cognitive behavioral therapy using diffusion tensor imaging. This will reveal the neural mechanisms underlying the effectiveness of cognitive behavioral therapy in treating OCD, and provide objective data for the selection of individual cognitive behavioral therapy strategies.
METHODS/DESIGN
Study design
A single-blind, parallel group, controlled trial.
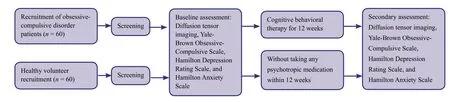
Figure 1: Experimental design.
Study setting
Beijing Anding Hospital, Capital Medical University,China.
Study procedure
A parallel, randomized, controlled trial will be performed to verify the ef ficacy of cognitive behavioral therapy for OCD.
(1) After providing informed consent, eligible participants will be enrolled according to the inclusion and exclusion criteria.
(2) Sixty OCD patients will undergo 12 weeks of cognitive behavioral therapy. An additional 60 healthy controls will form the control group.
(3) Two groups of participants will be assessed before and 12 weeks after treatment. The primary outcome will be fractional anisotropy (FA) values in the frontal-striatal-thalamic circuits assessed by diffusion tensor imaging. The secondary outcomes will be Yale-Brown Obsessive-Compulsive Scale(Y-BOCS), Hamilton Depression Rating Scale (HAM-D),and Hamilton Anxiety Scale (HAM-A) scores. A flow chart of the study design is shown in Figure 1.
Recruitment
Posters with recruitment information will be pasted in the waiting room, lounge, and entrance of Beijing Anding Hospital, Capital Medical University, China. Patients and healthy volunteers will be able to contact the project leader via their attending physician by telephone, email or letter.After providing written informed consent, all potential participants will be screened according to the inclusion and exclusion criteria.
Study participants
The study will investigate a cohort of OCD patients diagnosed at the Beijing Anding Hospital, Capital Medical University, China.
Patients are eligible for the study if they meet all of the in flusion criteria and none of the exclusion criteria.
Inclusion criteria
Patients meeting all of the following criteria will be considered for admission to the trial:
· Meeting the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders-IV (DSM-IV)for OCD (American Psychiatric Association, 1994)
· Scoring more than 16 on the Y-BOCS (Goodman et al.,1989a, b; Zhang et al., 1996)
· Scoring less than 18 on the HAM-D (Hamilton, 1960)
· Age between 20 and 45 years
· Right handedness
· No serotonin reuptake inhibitor treatment within 4 weeks before the trial
· Provision of informed consent regarding the trial procedure
Exclusion criteria
Patients presenting with any of the following will be excluded from the trial:
· Refractory OCD: symptoms not improved following 8 weeks of treatment with two different serotonin reuptake inhibitors (Y-BOCS score of < 25%) (Denys et al., 2004)
· Suicidal ideation or a desire to hurt others
· History of organic brain disease or major physical illness
· History of schizophrenia, affective disorders, or depression
· Drug dependence or psychoactive substance use
· Meeting the diagnostic criterion of DSM-IV Axis II Personality Disorders (American Psychiatric Association, 1994)
· Pregnant or lactating
Withdrawal criteria
Patients will be withdrawn from the trial if one of the following conditions occurs:
· Withdrawal of informed consent and declining to continue treatment
· Aggravation of their condition during treatment, such that it is necessary to combine antipsychotic drugs or replacement therapy
· Complications affecting ef ficacy and safety of judgment Control participants must meet the following criteria:
Inclusion criteria
· No previous or family history of mental illness
· No major physical disease or meeting the diagnostic criteria for mental illness
· Age between 20 and 45 years, of either sex
· Right handedness
· Junior high school degree or above
· Provision of informed consent regarding the trial procedure
Exclusion criteria
Control subjects meeting the diagnostic criteria of the DSMIV Axis II Personality Disorders (American Psychiatric Association, 1994) will be excluded from the trial.
Sample size
The trial will include an OCD group and a normal control group. In line with previous studies (Simpson et al.,2013; Li et al., 2014; Yang et al., 2015) and preliminary experiments, the minimum sample size will be 30 in each group. To allow for an estimated drop-out rate of 20%and an expected percentage of useable radiographic images of 90% (it is estimated that large head movements in 10% of subjects will result in image analysis failure),each group will need at least 40 samples. Therefore, the trial will commence with 60 participants in each group.The trial results will be analyzed according to intent-totreat analysis.
Interventions
OCD group: Cognitive behavioral therapy sessions will be conducted 14 times within 12 weeks (Whittal et al., 2005;Wilson and Chambless, 2005): Twice in weeks 1 and 2 and once a week in weeks 3 to 12. Each session will last approximately 50 minutes, with a total duration of treatment of 700 minutes.
Specific details of the cognitive behavioral therapy protocol are as follows:
First to third sessions: (1) Establishing the therapeutic relationship. (2) Collecting patient’s data (including childhood experiences, life background, social support, and predisposing factors) and performing psychological assessments (evaluating obsessions, intrusive thoughts, compulsive symptoms, safe behavior, and treatment power). (3)Psychological education allowing the patient to understand the relationships between ideas, emotions, and behaviors and to understand the role of cognitive behavioral therapy in OCD treatment. (4) Normalization of the negative emotions of intrusive thinking and anxiety.
Fourth to sixth sessions: (1) Identifying distorted cognition (using Socratic questions, such as exaggerating the danger, confused thinking and behavior, and controlling thinking). We will then conduct cognitive correction, planning and arranging behavioral trials to correct the distorted cognition. (2) Case analysis: We will connect the patient’s main issues with childhood experiences, family environment, important relationships, genetic factors, ideas, emotions, behavior, and distorted perception, analyzing the causes and the formation of the OCD. We will share this analysis with patients in verbal and graphical forms, allowing the patient to understand the causes of their symptom formation and the maintaining factors.
Seventh to twelfth sessions: Exposure and response prevention will be conducted with the help of the therapist.(1) Information collection: Monitoring ritual behavior,focusing on the time, frequency, and the scene or object of the ritual behavior. (2) Assessing the patient’s degree of discomfort, induced by the scene or object, and rating this on an anxiety discomfort scale from mild to severe(0-100%). Site or imagination exposure and ritual behavior prevention will be used. This will start with a scene or object of medium dif ficulty, and anxiety discomfort will be evaluated every 11 minutes. In imagined exposure therapy, the relevant stimulus will be recorded and listened to by the patient at home. (3) Exposure and response prevention completed by the patient themselves:Self-monitoring of symptoms and thoughts, and listening to treatment recordings.
Thirteenth and fourteenth sessions: Recalling treatment,and relapse prevention.
Patients will not take any psychotropic-related medication during treatment.
Normal control group: participants will not take any psychotropic-related medication or cognitive behavioral therapy.
Outcome measures
Data will be assessed at baseline and 12 weeks after treatment.
Primary outcomes
Diffusion tensor imaging: (1) Changes in FA values in the frontal-striatal-thalamic circuits will be assessed using a 3T MR scanner (Siemens, Erlangen, Germany):localization images, axial 49 layers, thickness 2.5 mm,without space, repetition time = 7,200 ms, echo time = 10 ms, resolution 128 × 128, total 8 minutes. (2) Sixty-four diffusion-weighted images in gradient direction, one b0 image (no diffusion weighting) and 3D-T1 images of thewhole brain (sagittal, 189 layers, thickness 1 mm, repetition time = 2,530 ms, echo time = 3 ms, resolution 128× 128). (3) Pretreatment: FSL4.19 software (Analysis Group, FMRIB, Oxford, UK) will be used to perform eddy current correction, skull removal correction, and direction correction. DTI Studio 2.41 software (Johns hopkins University, Baltimore, MD, USA) will be used to calculate and trace data. (4) Statistical Parametric Mapping 8 (SPM8) software (Wellcome Department of Imaging Neuroscience at University College London, London,UK) will be used to conduct template registration, and data and image processing.
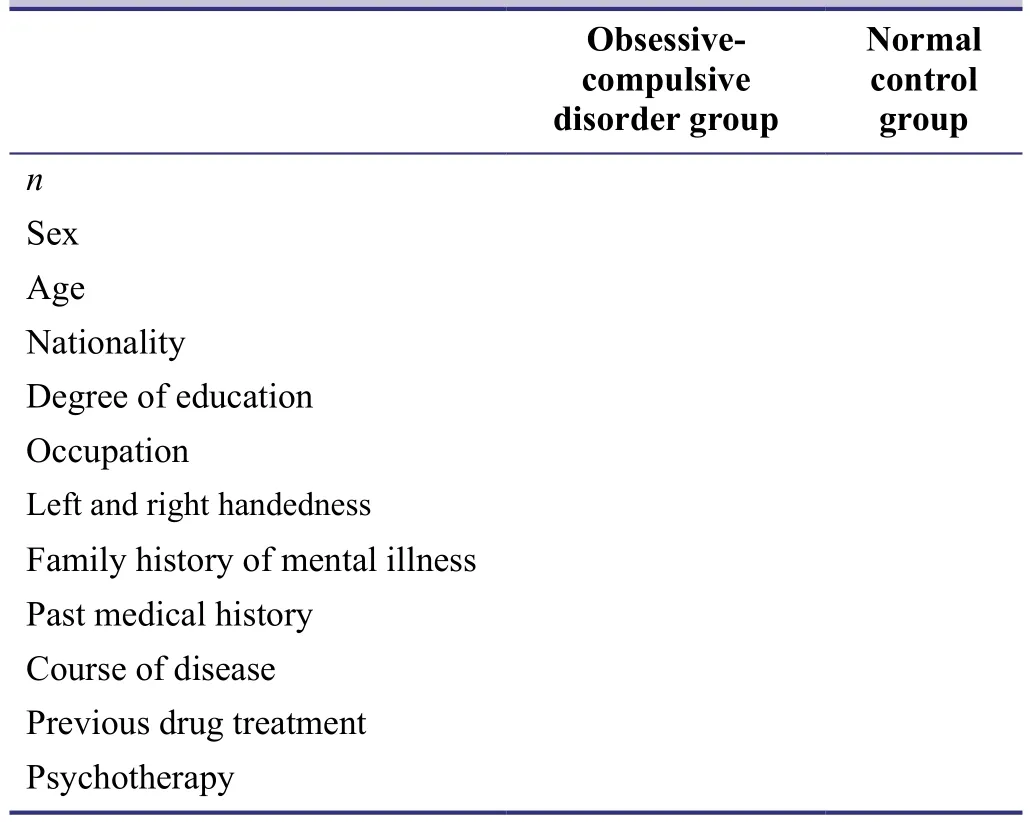
Table 2: Baseline patient data
Secondary outcomes
Y-BOCS scores: Y-BOCS was formulated by Goodman et al. (1989a, b) according to the diagnostic criteria of DSM-III-R, and has been modi fied by Zhang et al. (1996).It consists of 19 items, five grades, and four scores. The first 10 items are used to assess obsessive-compulsive symptoms and for calculating scores: Items 1-5 indicate obsessive thinking and items 6-10, compulsive behavior.The last nine items are ungraded supplementary parts of the scale assisting with a comprehensive assessment of the condition. The Y-BOCS reliability for clinical diagnosis/testing is r = 0.75 (P < 0.01), and the retest reliability is r= 0.91 (P < 0.001).
HAM-D (Hamilton, 1960): This scale sensitively re flects changes in depressive symptoms and has good reliability and validity, with a reliability coef ficient between raters of 0.88 and 0.99. For evaluating depression, the authenticity coef ficient, re flecting the severity of clinical symptoms, is 0.92. The total score better re flects the severity of the disease, with lower and higher total scores re flecting milder and more severe disease, respectively. Severe depressionis de fined as scores >24, moderate depression as 17-24,and no depression < 7.
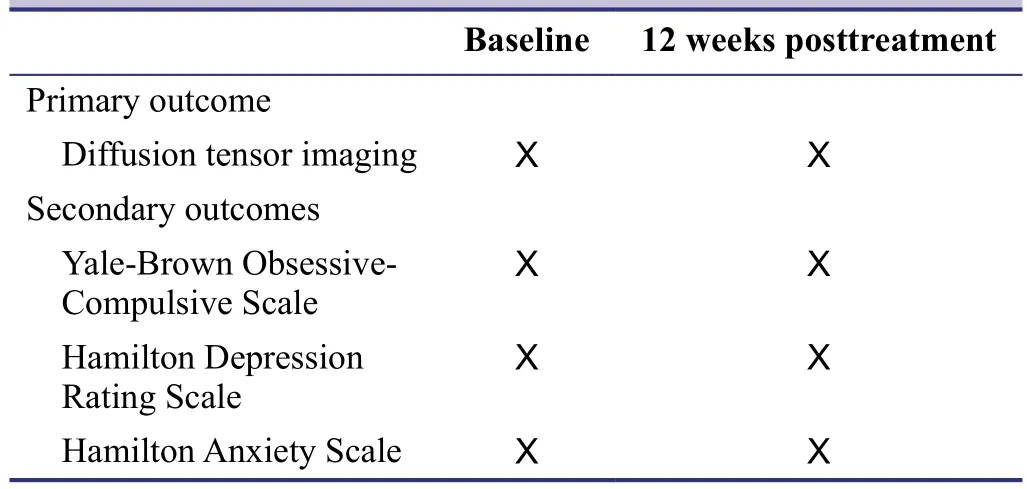
Table 3: Timing of outcome measure assessment
HAM-A (Hamilton, 1959): This scale contains 24 items and five grades (0-4). 0 = no symptoms, 1 = mild, 2 =moderate, 3 = severe, 4 = very severe. The reliability coefficient of the total score is 0.93. The individual reliability coef ficients of each item range between 0.83 and 2.00 (P <0.01), with a validity coef ficient of 0.36 (P < 0.05).
The baseline evaluation is shown in Table 2 and the timing of the outcome measure assessment in Table 3.
Data collection, management, analysis, and open access
Data collection
All data will be collected on case report forms and collated.A research associate will recheck the data and forward it to the data management unit. Data that are lost, logically contrary, mistaken, or uncon firmed will be questioned and notes recorded in the data management form by the data manager. The completed data management form will be delivered to researchers for rechecking and to answer outstanding questions. The database will be rechecked and modi fied by the data manager in response to the researcher’s answers. The data will be questioned again if necessary.
Data management
After blind review and database con firmation, the database will be locked by the researcher in charge. The locked database will not be altered and will be preserved, along with the original records, by Beijing Anding Hospital, Capital Medical University, China.
Data analysis
The database will be made available to a statistician for analysis. The results of these statistical analyses will be reported to a researcher and used to prepare the research report. The whole trial procedure will be monitored by a data monitoring committee.
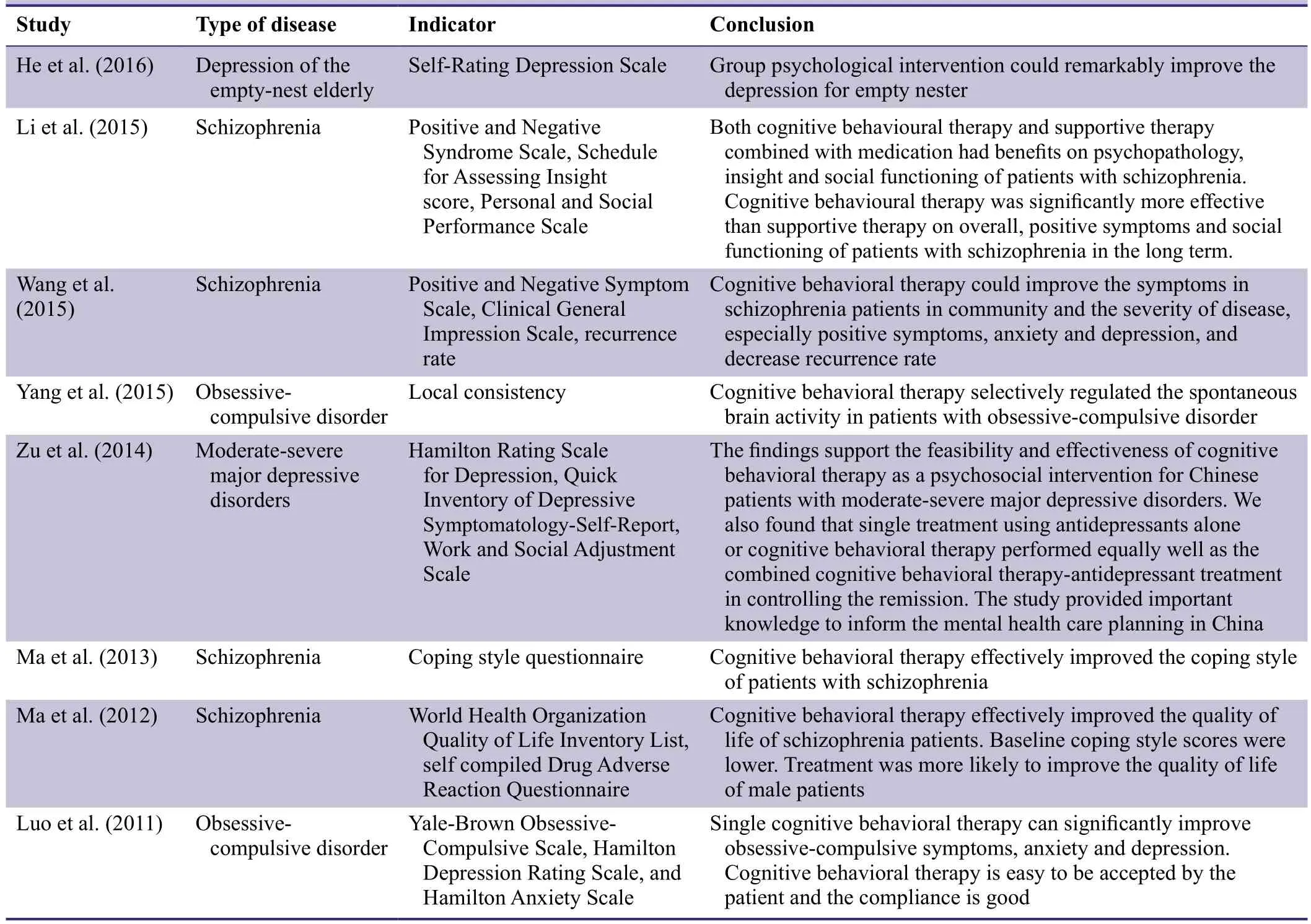
Table 4: Previous cognitive behavioral therapy studies by the investigators
Open access
All trial data will be published on the open access forum www. figshare.com.
Statistical analysis
All data will be analyzed using SPSS 13.0 software (SPSS,Chicago, IL, USA). Intention-to-treat analysis will be performed. FA values from diffusion tensor imaging will be expressed as the mean ± SD. Paired t-tests will be used to compare the difference in the connection and integrity of white matter fibers between the OCD and control groups.Paired sample t-tests will be used to compare the differences in the connections and integrity of white matter fibers before and after treatment in OCD patients. Constituent ratios of count data of Y-BOCS, HAM-D and HAM-A results will be analyzed using chi-square test. The overall ef ficiency between the groups will be compared by using Mann-Whitney U test. Multiple linear regression analysis will be used to analyze the relationship between the changes in connection and integrity of white matter fibers and clinical symptoms in OCD patients (α = 0.05). P < 0.05 will be considered statistically signi ficant.
Auditing
Trial progression will be reported to the ethical committee every 6-12 months, and progress will be updated in the registered database (Chinese Clinical Trial Registry) at the same time.
Confidentiality
Identi fied information will be preserved by the Beijing Anding Hospital of Capital Medical University of China, and only accessed by the Ethics Committee of Beijing Anding Hospital of Capital Medical University of China, the Food and Drug Supervision and Management Department, and the test executors. No data will be disclosed to any unauthorized party. The findings will be published for scientific purposes without revealing any patients’ identities, except as required by law.
DISCUSSION
Cognitive behavioral therapy is a widely used psychological treatment. Our team has accumulated much experience and scientific research in this area (Table 4). Our previous research has con firmed that this method can effectively improve the symptoms of OCD patients, but any underlying effect on brain tissue is not clear. This parallel, randomized, controlled trial will compare white matter fibers between OCD patients and normal controls. Our findings will provide information revealing the mechanisms of cognitive behavioral therapy in OCD, and a theoretical basis for the effectiveness of cognitive behavioral therapy in the clinic. However, this trial lacks the advantage of a follow-up, so we will perform a large-sample multi-center trial investigating cognitive behavioral therapy for OCD and including follow-up in future investigations. Also,in clinical practice, the majority of patients also receive pharmacological treatment, so it will be necessary to carry out future research on the combined effect of medication and cognitive behavioral therapy.
Trial status
Data processing and in-depth analysis are ongoing at the time of submission.
Conflicts of interest
None declared.
Author contributions
ZJL designs the study, and performs experiments. XYY screens and assesses participants, analyzes data and writes the manuscript. JL YM, ZHG, and XJY perform cognitive behavioral therapy. All authors approve the final version of this manuscipt.
We are very grateful to the State Key Laboratory of Cognitive Neuroscience and Learning of Beijing Normal University of China for technical support.
Plagiarism check
This paper was screened twice using CrossCheck to verify originality before publication.
Peer review
This paper was double-blinded and stringently reviewed by international expert reviewers.
American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders.
Apostolova I, Block S, Buchert R, Osen B, Conradi M, Tabrizian S,Gensichen S, Schr?der-Hartwig K, Fricke S, Rufer M, Weiss A,Hand I, Clausen M, Obrocki J (2010) Effects of behavioral therapy or pharmacotherapy on brain glucose metabolism in subjects with obsessive-compulsive disorder as assessed by brain FDG PET. Psychiatry Research: Neuroimaging 184:105-116.
Bolton D, Perrin S (2008) Evaluation of exposure with responseprevention for obsessive compulsive disorder in childhood and adolescence. J Behav Ther Exp Psychiatry 39:11-22.
Cannistraro PA, Makris N, Howard JD, Wedig MM, Hodge SM,Wilhelm S, Kennedy DN, Rauch SL (2007) A diffusion tensor imaging study of white matter in obsessive-compulsive disorder.Depress Anxiety 24:440-446.
Denys D, Zohar J, Westenberg HG (2004) The role of dopamine in obsessive-compulsive disorder: preclinical and clinical evidence.J Clin Psychiatry 65 Suppl 14:11-17.
Fontenelle LF, Bramati IE, Moll J, Mendlowicz MV, de Oliveira-Souza R, Tovar-Moll F (2011) White matter changes in OCD revealed by diffusion tensor imaging. CNS Spectr 16:101-109.
Freyer T, Kl?ppel S, Tüscher O, Kordon A, Zurowski B, Kuelz AK,Speck O, Glauche V, Voderholzer U (2011) Frontostriatal activation in patients with obsessive-compulsive disorder before and after cognitive behavioral therapy. Psychol Med 41:207-216.
Garibotto V, Scifo P, Gorini A, Alonso CR, Brambati S, Bellodi L,Perani D (2010) Disorganization of anatomical connectivity in obsessive compulsive disorder: a multi-parameter diffusion tensor imaging study in a subpopulation of patients. Neurobiol Dis 37:468-476.
Goodman WK, Grice DE, Lapidus KA, Coffey BJ (2014) Obsessive-compulsive disorder. Psychiatr Clin North Am 37:257-267.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P,Heninger GR, Charney DS (1989a) The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch Gen Psychiatry 46:1012-1016.
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS (1989b) The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability.Arch Gen Psychiatry 46:1006-1011.
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50-55.
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56-62.
He ML, Long AL, An FR, Ma Y, Guo ZH, Li ZJ, Cheng XM (2016)The effect of group psychological intervention on depression for empty nester. Zhongguo Huli Guanli 16:10-13.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593-602.
Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB,American Psychiatric Association (2007) Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry 164:5-53.
Li F, Huang X, Yang Y, Li B, Wu Q, Zhang T, Lui S, Kemp GJ,Gong Q (2011) Microstructural brain abnormalities in patients with obsessive-compulsive disorder: diffusion-tensor MR imaging study at 3.0 T. Radiology 260:216-223.
Li Z, Ji W, Li D, Li X, Feng W (2014) Microstructural abnormality in left nucleus accumbens predicts dysfunctional beliefs in treatment-resistant obsessive-compulsive disorder. Med Sci Monit 20:2275-2282.
Li ZJ, Guo ZH, Wang N, Xu ZY, Qu Y, Wang XQ, Sun J, Yan LQ,Ng RM, Turkington D, Kingdon D (2015) Cognitive-behavioural therapy for patients with schizophrenia: a multicentre randomized controlled trial in Beijing, China. Psychol Med 45:1893-1905.
Li ZJ, Wang JS, Qiu BW (2004) Psychosocial risk factors and integrated model of obsessive-compulsive symptoms in adolescents.Int J Psychol 39:S602.
Lim KO, Helpern JA (2002) Neuropsychiatric applications of DTI -a review. Nmr Biomed 15:587-593.
Luo J, Li ZJ (2010) Research progress of cognitive behavioral therapy for obsessive-compulsive disorder. Zhonghua Shenjing Ke Zazhi 43:123-125.
Luo J, Guo ZH, Li ZJ (2010) Brain functional imaging study of obsessive compulsive disorder. Guoji Shenjingbing Xue Zazhi 37:157-159.
Luo J, Li ZJ, Han HY, Xu ZY, Guo ZH, Liu J, Xiong HF (2011) Efficacy of single cognitive behavioral therapy for obsessive-compulsive disorder patients without medication. Zhongguo Xinli Weisheng Zazhi 25:910-914.
Ma Y, Li ZJ, Xu ZY, Guo ZH, Qu Y, Wang XQ, David K (2012) Effects of cognitive behavioral therapy on quality of life in patients with schizophrenia: a single blind randomized controlled study.Zhongguo Xinli Weisheng Zazhi 26:801-807.
Ma Y, Li ZJ, Xu ZY, Guo ZH, Qu Y, Wang XQ, David K (2013)Effects of Cognitive Behavioral Therapy on Coping Style for Patients with Schizophrenia. Zhongguo Xinli Weisheng Zazhi 21:801-807.
Menzies L, Williams GB, Chamberlain SR, Ooi C, Fineberg N,Suckling J, Sahakian BJ, Robbins TW, Bullmore ET (2008) White matter abnormalities in patients with obsessive-compulsive disorder and their first-degree relatives. Am J Psychiatry 165:1308-1315.
Nakamae T, Narumoto J, Sakai Y, Nishida S, Yamada K, Nishimura T, Fukui K (2011) Diffusion tensor imaging and tract-based spatial statistics in obsessive-compulsive disorder. J Psychiatr Res 45:687-690.
Nakao T, Nakagawa A, Yoshiura T, Nakatani E, Nabeyama M, Yoshizato C, Kudoh A, Tada K, Yoshioka K, Kawamoto M, Togao O, Kanba S (2005) Brain activation of patients with obsessivecompulsive disorder during neuropsychological and symptom provocation tasks before and after symptom improvement: A functional magnetic resonance imaging study. Biol Psychiatry 57:901-910.
Saito Y, Nobuhara K, Okugawa G, Takase K, Sugimoto T, Horiuchi M, Ueno C, Maehara M, Omura N, Kurokawa H, Ikeda K,Tanigawa N, Sawada S, Kinoshita T (2008) Corpus callosum in patients with obsessive-compulsive disorder: diffusion-tensor imaging study. Radiology 246:536-542.
Simpson HB, Foa EB, Liebowitz MR, Ledley DR, Huppert JD, Cahill S, Vermes D, Schmidt AB, Hembree E, Franklin M, Campeas R, Hahn C-G, Petkova E (2008) A randomized, controlled trial of cognitive-behavioral therapy for augmenting pharmacotherapy in obsessive-compulsive disorder. Am J Psychiatry 165:621-630.
Simpson HB, Foa EB, Liebowitz MR, Huppert JD, Cahill S, Maher MJ, McLean CP, Bender J, Marcus SM, Williams MT, Weaver J, Vermes D, Van Meter PE, Rodriguez CI, Powers M, Pinto A, Imms P, Hahn CG, Campeas R (2013) Cognitive-behavioral therapy vs risperidone for augmenting serotonin reuptake inhibitors in obsessive-compulsive disorder: a randomized clinical trial.JAMA psychiatry 70:1190-1199.
Skarphedinsson G, Weidle B, Thomsen PH, Dahl K, Torp NC, Nissen JB, Melin KH, Hybel K, Valderhaug R, Wentzel-Larsen T,Compton SN, Ivarsson T (2015) Continued cognitive-behavior therapy versus sertraline for children and adolescents with obsessive-compulsive disorder that were non-responders to cognitivebehavior therapy: a randomized controlled trial. Eur Child Adolesc Psychiatry 24:591-602.
Storch EA, Bussing R, Small BJ, Geffken GR, McNamara JP, Rahman O, Lewin AB, Garvan CS, Goodman WK, Murphy TK (2013)Randomized, placebo-controlled trial of cognitive-behavioral therapy alone or combined with sertraline in the treatment of pediatric obsessive-compulsive disorder. Behav Res Ther 51:823-829.
Wang ZQ, Guo ZH, Han GL, Wang J, Li ZJ (2015) The Effects of Cognitive Behavioral Therapy for Schizophrenia in Community.Zhongguo Jiankang Xinlixue Zazhi 23:16-19.
Whittal ML, Thordarson DS, McLean PD (2005) Treatment of obsessive-compulsive disorder: cognitive behavioral therapy vs. exposure and response prevention. Behav Res Ther 43:1559-1576.
Wilson KA, Chambless DL (2005) Cognitive therapy for obsessivecompulsive disorder. Behav Res Ther 43:1645-1654.
World Health Organization (2008) The Global Burden of Disease:2004 Update.
Yang XY, Sun J, Luo J, Zhong ZX, Li P, Yao SM, Xiong HF, Huang FF, Li ZJ (2015) Regional homogeneity of spontaneous brain activity in adult patients with obsessive-compulsive disorder before and after cognitive behavioural therapy. J Affect Disord 188:243-251.
Zarei M, Mataix-Cols D, Heyman I, Hough M, Doherty J, Burge L,Winmill L, Nijhawan S, Matthews PM, James A (2011) Changes in gray matter volume and white matter microstructure in adolescents with obsessive-compulsive disorder. Biol Psychiatry 70:1083-1090.
Zhang Y, Meng FQ, Cui YH, Gan XD, Guo W (1996) A study on the reliability and validity of the modi fied Yale-Brown Obsessive Compulsive Scale. Zhongguo Xinli Weisheng Zazhi 10:205-207.
Zu S, Xiang YT, Liu J, Zhang L, Wang G, Ma X, Kilbourne AM,Ungvari GS, Chiu HF, Lai KY, Wong SY, Yu DS, Li ZJ (2014)A comparison of cognitive-behavioral therapy, antidepressants,their combination and standard treatment for Chinese patients with moderate-severe major depressive disorders. J Affect Disord 152-154:262-267.
 Asia Pacific Journal of Clinical Trials:Nervous System Diseases2016年3期
Asia Pacific Journal of Clinical Trials:Nervous System Diseases2016年3期
- Asia Pacific Journal of Clinical Trials:Nervous System Diseases的其它文章
- Evaluation of cardiac autonomic status using QTc interval in patients with leprosy
- Efficacy of spontaneous laughter in the post-operative treatment of pain and anxiety in children: study protocol for a randomized controlled trial
- Effect of pre-incisional anterior scalp block on intraoperative opioid consumption in adult patients undergoing elective craniotomy to remove tumor: study protocol for a randomized double-blind trial
- Effects of lung protective ventilation on pulmonary function,inflammation, and oxidative stress in patients undergoing craniotomy: study protocol for a multi-center, randomized,parallel, controlled trial
- Migraine prevention by noninvasive electrical fastigial nucleus stimulation: a multi-center, randomized, double-blind,sham-controlled trial
- Scalp acupuncture twisting manipulation for treatment of hemiplegia after acute ischemic stroke in patients: study protocol for a randomized, parallel, controlled, single-blind trial
