Multiple Myeloma Mimicking Spondyloarthritis: a Case Report
Ai-chun Liu, Yan-ying Liu, Yan Li, Li Zhang, and Zhan-guo Li*
1Department of Rheumatology and Immunology, Peking University People’s Hospital, Beijing 100044, China
2Department of Rheumatology and Immunology, People’s Hospital, Xinyi 221400, China
MULTIPLE myeloma (MM) is a hematologic malignancy of differentiated plasma cells that accumulate and proliferate in the bone marrow. MM patients often develop bone disease that results in severe bone pain, osteolytic lesions, and pathologic fractures,1presenting with unexplained backache or bone pain in the long bones, ribs, skull, or pelvis.2However, the low backache mimicking spondyloarthritis in MM is uncommon during clinical practice. Spondyloarthritis is a chronic systemic inflammatory disorder of the axial skeleton, mainly affecting the sacroiliac joint and spine causing low backache.3Here we report a patient with MM which was initially misdiagnosed and treated as spondyloarthritis.
CASE DESCRIPTION
A 44-year-old man visited local hospital with one-year history of lower back and buttock pain, with no significant morning stiffness. His motion of the lumbar spine was limited. The chest expansion at the fourth intercostal space was 2 cm. Laboratory test showed elevation of the erythrocyte sedimentation rate (ESR) to 54 mm/hour. The blood counts, calcium, and creatinine levels were normal. The auto-antibodies and human leukocyte antigen-B27 (HLA-B27) were all negative. Serum electrophoresis and immunoglobulin detection was not performed in local hospital. Computed tomography scan of sacroiliac joint showed sacroiliitis at the right region of the joint (Fig.1). A diagnosis of spondyloarthritis was made according to the Assessment of SpondyloArthritis international Society (ASAS) criteria,3and a treatment of full-dose acetaminophen and leflunomide was prescribed, but was discontinued due to inefficacy after 10 months.
The patient experienced Raynaud’s phenomenon 5 months later, along with dizziness, blurring of vision, palpitation and chest distress after walking 200 m. In the meantime he had lost 2.5 kg of weight. He was referred to Peking University People’s Hospital for further evaluation. A physical examination showed positive Patrick’s test, and limited chest expansion and lumbar spine motion. Results of lungs and neurological examination were normal.
Laboratory examinations upon admission revealed hemoglobin at 66 g/L, white blood cell count, platelet count, serum calcium and creatinine levels were normal, ESR at 60 mm/hour, and C-reactive protein at 24.1 mg/L. Twenty-four hour urinary protein excretion was 0.96 g/L. Particularly cold agglutination phenomenon was observed. Rheumatoid factor, anti-nuclear antibody, anti-neutrophil cytoplasmic antibody, anti ds-DNA antibody and HLA-B27 were all negative. Serum electrophoresis showed a thick M band typed to be IgG-κ by immunofixation. Serum IgG was 17.6 g/L (normal: 694-1618 mg/dl), IgA 1260 mg/L (normal: 68-378 mg/dl), IgM 429 mg/L (normal: 60-263 mg/dl). Serum and urine free κ-light chains were 28.4 mg/L (normal: 0-18.5 mg/L) and 37.6 g/L (normal: 6.29-13.50 g/L) respectively. Radiograph also revealed lytic lesions in the skull and pelvis. Atypia was observed in 33% of the plasma cells in the bone marrow (Fig. 2).
According to the criteria for MM established by the International Myeloma Working Group,4he was diagnosed as symptomatic MM with M-protein in serum and urine, bone marrow (clonal) plasma cells >10%, related organ or tissue impairment with bone destruction manifested as back pain, serum hyperviscosity, and anemia. Plasmapheresis and chemical therapy with vincristine, adriamycin, dexamethasone were administered, after which a significant alleviation of signs and symptoms was observed.
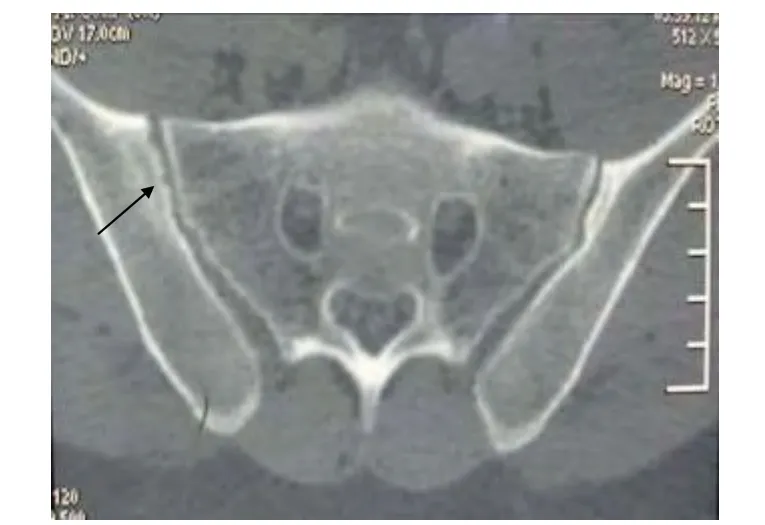
Figure 1. A computed tomographic image of sacroiliac joint shows a single erosion (arrow) in the right sacroiliac joint, particularly in the iliac bone.
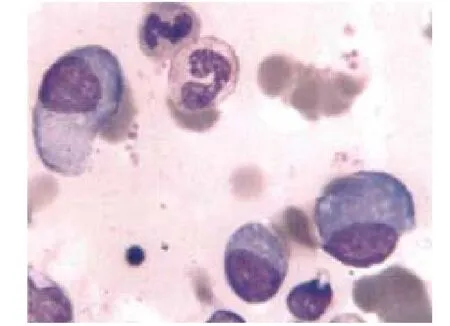
Figure 2. Bone marrow aspiration shows atypical plasma cell infiltration. (Wright's staining ×1000)
DISCUSSION
Though this patient met the criteria of spondyloarthritis, many of his abnormities could not be explained by spondyloarthritis. In this case, we noticed the following differences with spondyloarthritis: 1) the low backache was persistent, and could not be eased by lying, rest, or exercise; 2) adequate nonsteroidal anti-inflammatory drug was ineffective; 3) the symptoms developed quickly in a short time; 4) the red flags including anemia, loss of weight were present. Low backache with spondyloarthritis usually has morning stiffness, and could be improved by exercise.5The activity limitation of spine in spondyloarthritis is caused by ossification of spine ligament and zygapophyseal joint rigidity and will occur several years after onset of low back pain.6Anemia (Hb <90 g/L) and weight loss are rare in spondyloarthritis. Thus, if adequate dose of NSAIDs cannot improve the symptoms and HLA-B27 is negative, misdiagnosis and some rare diseases such as malignancy diseases should be considered.
MM is a B-cell malignancy characterized by the neoplastic proliferation of a plasma cell clone that produces a monoclonal immunoglobulin.1The median age at diagnosis is 66 years.7The clinical manifestations of MM are hetero- geneous, including bone complications, symptoms of impaired hemopoiesis and hyperviscosity, renal dysfunction, infections, peripheral neuropathy and extramedullary disease.8In this case, the patient also developed Raynaud’s phenomenon and heart failure symptoms of MM with hyperviscosity. Blood hyperviscosity is an uncommon complication in MM, with the incidence being 2%-6% in IgG MM, which causes a variety of clinical manifestations including bleeding from mucosal membranes, congestive heart failure, retinopathy, and neurologic features like dizziness and visual changes. Pathogenic factors for hyperviscosity are due to excessive production of abnormal clonal gamma globulins or paraproteins.9At the same time, cryoglobulinemia was observed. The presence of cryoglobulinemia can result in a strikingly temperature-dependent elevation of blood viscosity.10This phenomenon appears like Raynaud’s phenomenon. Plasmapheresis promptly relieves the symptoms and should be done regardless of the viscosity level if the patient has signs or symptoms of hyperviscosity.9In this case, the patient accepted plasmapheresis and a significant relief in neurological and heart failure-related signs and symptoms was observed.
In conclusion, MM with low backache as the initial manifestation can be misdiagnosed as spondyloarthritis. The diagnosis of MM may be challenging for the physicians, even the hematologist. Careful observation of the clinical course and the awareness of a possibility of MM are essential for the accurate diagnosis of and timely treatment for MM.
1. Oranger A, Carbone C, Izzo M, et al. Cellular mechanisms of multiple myeloma bone disease. Clin Dev Immunol 2013 [cited 2013 Dec 1]. Available from: http://www. hindawi.com/journals/jir/2013/289458/.
2. Southerst D, Dufton J, Stern P. Multiple Myeloma presenting as sacroiliac joint pain: a case report. J Can Chiropr Assoc 2012; 56: 94-101.
3. Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009; 68:ii1-44.
4. International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol 2003; 121:749-57.
5. Calin A. Seronegative spondyloarthritides. Med Clin North Am 1986; 70:323-36.
6. Deng XL, Liu XY, Xu N. Comparative study on low back pain misdiagnosed as spondyloarthropathy. Clin Rheumatol 2009; 28: 893-8.
7. Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003; 78:21-33.
8. Dimopoulos MA, Terpos E. Multiple myeloma. Ann Oncol 2010; 21:vii143-50.
9. Kwaan HC. Hyperviscosity in plasma cell dyscrasias. Clin Hemorheol Microcirc 2013; 55:75-83.
10. Stone MJ, Bogen SA. Evidence-based focused review of management of hyperviscosity syndrome. Blood 2012; 119:2205-8.
 Chinese Medical Sciences Journal2014年4期
Chinese Medical Sciences Journal2014年4期
- Chinese Medical Sciences Journal的其它文章
- Inhibition of Xanthine Oxidase Activity by Gnaphalium Affine Extract
- Evaluation of Risk Factors for Arytenoid Dislocation after Endotracheal Intubation: a Retrospective Case-control Study
- Non-enhanced Low-tube-voltage High-pitch Dual-source Computed Tomography with Sinogram Affirmed Iterative Reconstruction Algorithm of the Abdomen and Pelvis
- Primary Combined Intra-articular and Extra-articular Synovial Osteochondromatosis of Shoulder: a Case Report
- Squamous Cell Carcinoma of Small Intestine: a Case Report△
- BRAF V600E Mutation as a Predictive Factor of Anti-EGFR Monoclonal Antibodies Therapeutic Effects in Metastatic Colorectal Cancer: a Meta-analysis
