Sclerosing Cholangitis after Transcatheter Arterial Chemoembolization:a Case Report
Kai Qu ,Chang Liu *,Qi-fei Wu ,Bo Wang ,Aasef Mohamed Ali Mansoor ,Hao Qin ,Qiang Ma,and Ya-min Liu
1Department of Hepatobiliary Surgery,2Department of Cardiovascular Intervention,the First Affiliated Hospital,Medical School of Xi'an Jiaotong University,Xi'an 710061,China
SCLEROSING cholangitis represents progressing jaundice or/and paroxysmal symptom of cholangitis,finally developing to end-stage of liver disease.When compared with primary sclerosing cholangitis (PSC),there are no apparent differences in pathology and clinical manifestation in secondary sclerosing cholangitis (SSC).But unlike PSC,SSC always has underlying causes,the most common being biliary obstruction,surgical trauma and ischemic injury of bile duct during liver transplantation.1,2Repeated transcatheter arterial chemoembolization (TACE) leading to progressive SSC was rarely reported.Because of its rapid and irreversible progression,once SSC begins,it is difficult to deal with.Therefore,clinicians need to pay more attention to it.
CASE DESCRIPTION
A 23 years old man on physical examination was found to have a neoplastic lesion in the left liver lobe and alpha-fetoprotein (AFP) was 567.3 μg/L on May 2007.Whereafter,left lobe resection was performed and pathology confirmed it was a primary hepatocellular carcinoma (Stage II).One month after surgery the patient was followed up.His AFP level was significantly elevated at 443.0 μg/L,but no positive signs were found in CT scans.Considering hepatic tumor recurrence,we advised this patient to undergo hepatic arterial infusion.
After selective hepatic angiography,chemotherapeutic agents (epirubicin 60 mg and fluorodeoxyuridine 1.25 g dissolved into 150 mL saline solution) were injected.No fever,chills,abdominal pain,diarrhea and jaundice were observed after the procedure.The patient totally underwent another two interventional therapy procedures with a similar approach performed by the same professional radiologist (Table 1).Thirty months after surgery,we performed the 4th TACE and injected emulsion (epirubicin 50 mg+fluorodeoxyuridine 1.0 g+iodized oil 15 mL) and gelfoam particles (diameter,500-1000 μm) for abnormal staining seen in the right hepatic lobe and the caudate lobe(Fig.1).
One month after the 4th TACE,fever and progressive aggravating jaundice were observed in this patient.White blood cell count was elevated and AFP was 240 μg/L.Cholestasis parameters including alkaline phosphatase(1951.4 U/L),γ-glutamyl transpeptadase (828 U/L),total bilirubin (425.8 μmol/L),and direct bilirubin (175.2 μmol/L)were significantly elevated.Autoimmune parameters suchas antinuclear antibody,smooth muscle antibody,antimitochondrial antibody and perinuclear antineutrophil cytoplasmic antibodies were all negative.CT scans after the 4th TACE showed multiple round lesions with central necrosis (Fig.2).Endoscopic retrograde cholangiopancreatography (ERCP) suggested diffuse intrahepatic and extrahepatic bile duct occlusions and rarefaction of the small bile ducts (Fig.3A).Pancreatic ducts were entirely normal.Histological findings of needle biopsy of liver showed that there was an inflammatory response of infiltrated lymphocytes and plasma cells and fibroid degeneration in the portal regions.Cholestasis with interlobular bile duct proliferation was also observed (Fig.4).
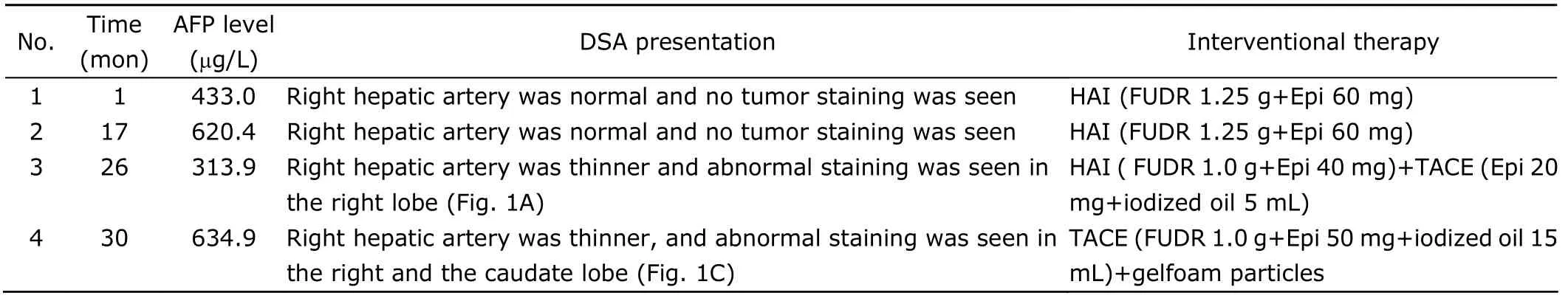
Table 1.Interventional treatment for four times
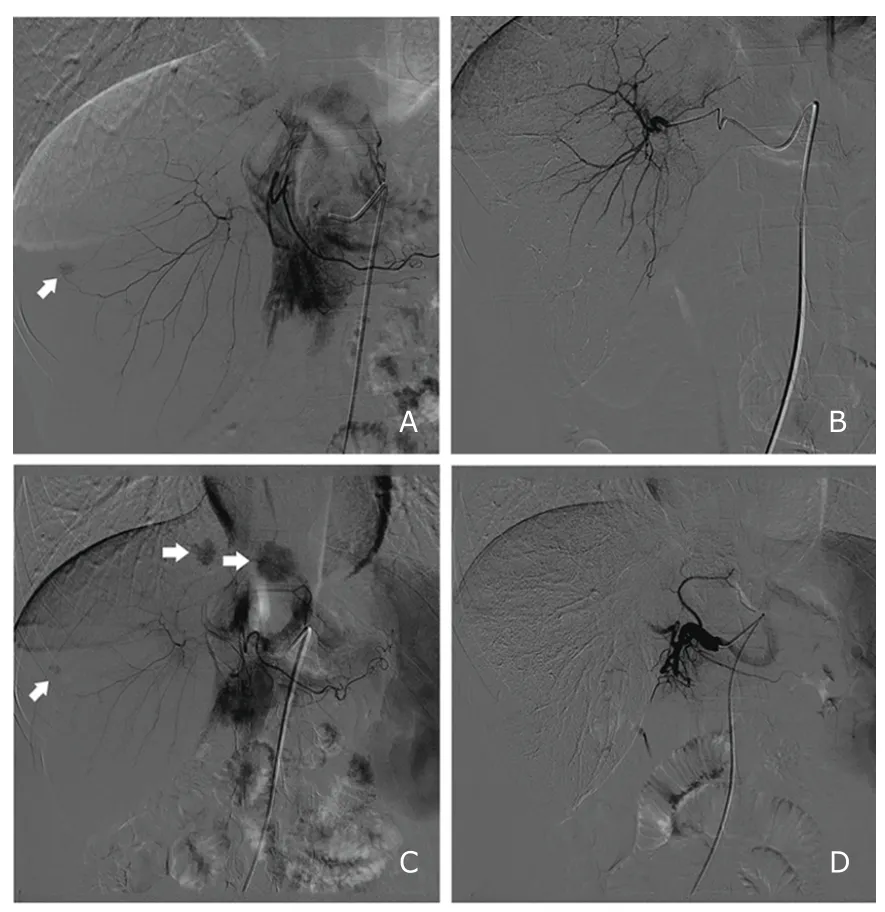
Figure 1.DSA presentations of the 3rd and 4th TACE.
Ursodeoxycholic acid (UDCA) (10 mg/kg body weight)and antibiotics were used in our patient.To relieve jaundice of this patient,we performed endoscopic nasobiliary drainage(ENBD) and flushing of the bile duct with a continuous infusion of saline solution.After ENBD,both clinical manifestation and biochemical values of this patient were mitigated (Fig.5).The patient was discharged on the 15th day after removed ENBD tube and with remarkable improvement of bile duct stricture(Fig.3B).A seventeen months follow-up of patient showed that,at present,he is in a relatively stable condition without clinical sign of hepatic failure.
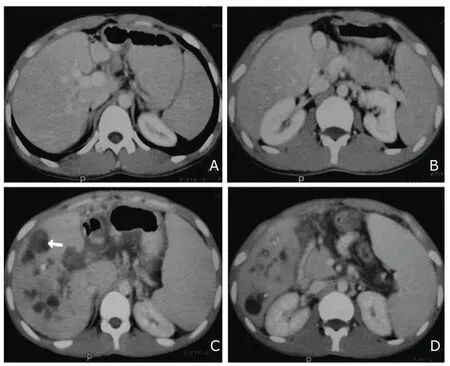
Figure 2.CT scan images pre-and post-4th TACE.
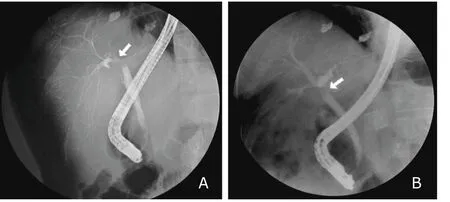
Figure 3.Endoscopic retrograde cholangiopancreatography (ERCP)shows common hepatic duct at the level of the hilum denotes a stricture (about 0.5 cm in length,arrow),and intrahepatic bile ducts are thin and their route is stiffened (A).ERCP shows the stricture becomes wider after endoscopic nasobiliary drainage (B,arrow).
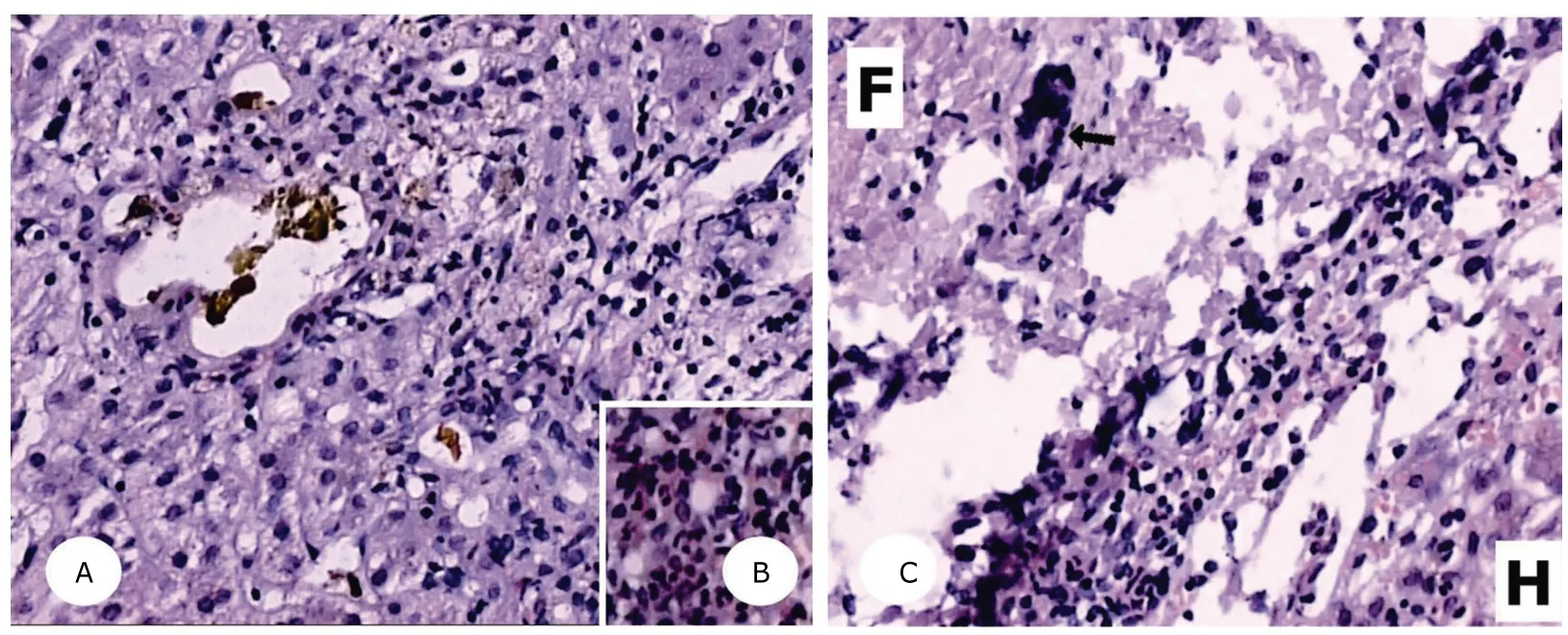
Figure 4.Histological findings of hepatic biopsy.
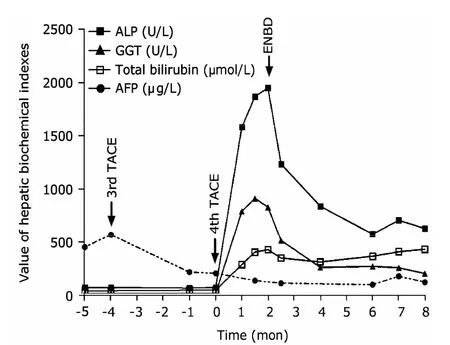
Figure 5.Change of values of hepatic biochemical indexes before and after the 4th TACE.
DISCUSSION
Since 1976 Goldstein reported about how to treat malignant tumors of the liver by TACE,it has been accepted as the primary approach of non-operative treatment.Increased number of complications with the wide use of TACE gradually attracted people’s attention.Other than the common post-embolization syndrome,sclerosing cholangitis secondary to TACE being the most difficult to deal with was rarely reported.3,4Review of the literature,only Richardetet al5has reported two cases of sclerosing cholangitis after TACE whose clinical presentation and images are similar to us.
The pathogenesis of SSC is still unknown,but ischemic injury caused by damage of the peribiliary capillary plexus during TACE procedure may be the fundamental cause.6Animal experimental studies showed that occlusion of arteries less than 200 μm in diameter rather than larger arteries may cause ischemic cholangiopathy.7,8Some clinical survey showed that a few predisposing factors of this patient such as history of hepatocellular carcinoma without cirrhosis,repeated TACE procedures and prior liver resection lead to high risk of bile duct complications.9,10Interestingly,all of these predisposing factors were related with microvascular abnormality.In the following TACE treatment,embolic agent acted as an embolus and contributed to ischemic injury of the peribiliary capillary plexus that developed sclerosing cholangitis finally.
So far,therapy options for SSC patients are limited and continuous drainage of bile duct is the key treatment.Endoscopic therapy including ENBD as an effective method of palliation is recommended11and was also proved by this case.Clinical manifestation and biochemical values usually improve after the foregoing treatment.Therefore although endoscopic treatment will only improve liver function temporarily,but it should be considered as a primary treatment protocol even if we are unsure if it has any beneficial effect on the disease prognosis.Complications with biliary tract infection should be treated with antibiotics and doses should be high enough that an effective concentration is maintained in the bile duct.Besides high-dose UDCA seems reasonable in some clinical drug trials.12For this patient,long-term treatment of high-dose UDCA combined with ENBD had showed good effect.
1.Ruemmele P,Hofstaedter F,Gelbmann CM.Secondary sclerosing cholangitis.Nat Rev Gastroenterol Hepatol 2009;6:287-95.
2.Abdalian R,Heathcote EJ.Sclerosing gholangitis:a focus on secondary causes.Hepatology 2006;44:1063-74.
3.Xia J,Ren Z,Ye S,et al.Study of severe and rare complications of transarterial chemoembolization (TACE) for liver cancer.Eur J Radiol2006;59:407-12.
4.Sakamoto I,Iwanaga S,Nagaoki K,et al.Intrahepatic biloma formation (bile duct necrosis) after transcatheter arterial chemoembolization.Am J Roentgenol 2003;181:79-87.
5.Richardet JP,Lons T,Sibony M,et al.Secondary sclerosing cholangitis and chemoembolization with lipiodol.Gastroenterol Clin Biol 1994;18:168-71.
6.Kobayashi S,Nakanuma Y,Terada T,et al.Postmortem survey of bile duct necrosis and biloma in hepatocellular carcinoma after transcatheter arterial chemoembolization therapy:relevance to microvascular damages of peribiliary capillary plexus.Am J Gastroenterol 1993;88:1410-5.
7.Deltenre P,Valla DC.Ischemic cholangiopathy.J Hepatol 2006;44:806-17.
8.Kemeny MM,Battifora H,Blayney DW,et al.Sclerosing cholangitis after continuous hepatic artery infusion of FUDR.Ann Surg 1985;202:176-81.
9.Chung JW,Park JH,Han JK,et al.Hepatic tumors:Predisposing factors for complications of transcatheter oily chemoembolization.Radiology 1996;198:33-40.
10.Yu JS,Kim KW,Jeong MG,et al.Predisposing factors of bile duct injury after transcatheter arterial chemoembolization (TACE) for hepatic malignancy.Cardiovasc Intervent Radiol 2002;25:270-4.
11.Alazmi WM,McHenry L,Watkins JL,et al.Chemotherapy-induced sclerosing cholangitis:long-term response to endoscopic therapy.J Clin Gastroenterol 2006;40:353-7.
12.Lindor KD,Kowdley KV,Luketic VA,et al.High-dose ursodeoxycholic acid for the treatment of primary sclerosing cholangitis.Hepatology 2009;50:808-14.
 Chinese Medical Sciences Journal2011年3期
Chinese Medical Sciences Journal2011年3期
- Chinese Medical Sciences Journal的其它文章
- Sutureless Intestinal Anastomosis with a Novel Device of Magnetic Compression Anastomosis△
- Choroidal Tuberculoma in an ImmunocompetentYoung Patient
- Influence of Deleted in Colorectal Carcinoma Gene on Proliferation of Ovarian Cancer Cell Line SKOV-3 In Vivo and In Vitro
- Cytogenetic and Clinical Analysis of 340 Chinese Patients with Primary Amenorrhea
- Serum HIF-1α and VEGF Levels Pre-and Post-TACE in Patients with Primary Liver Cancer
- Effect of Multiple Coatings of One-step Self-etching Adhesive on Microtensile Bond Strength to Primary Dentin
