Cytogenetic and Clinical Analysis of 340 Chinese Patients with Primary Amenorrhea
Hong Yu,Xun-min Bian*,Jun-tao Liu,Na Hao,Jing Zhou,and Shan-ying Liu
Department of Obstetric and Gynecology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
PRIMARY amenorrheais defined as the absence of menses by 16 years of age in the presence of normal secondary sexual characteristics or by 14 years of age when there is no visible secondary sexual characteristic development and the adolescent growth spurt.1Considerable cytogenetic studies on primary amenorrhea have been available in the recent literature.These studies have noted certain chromosomal abnormalities as possible causes of primary amenorrhea in addition to functional imbalance of endocrine system.Cytogenetic and clinical features of 340 patients with primary amenorrhea were reported here.
PATIENTS AND METHODS
Patients
From January,2007 to December,2009,340 patients with primary amenorrhea accepted cytogenetic chromosome analyses at Genetic Laboratory of Obstetric and Gynecology Department,Peking Union Medical College Hospital.All patients with primary amenorrhea were social females and diagnosed from age 14 to 34 years.The complaints were absence of the onset of menstruation,no visible secondary sexual characteristic development,short stature and learning difficulty.Short stature is defined as a height less than the 3rd percentile or a value of 2 standard deviations below the mean height.2The clinical data were recorded by physical examination and ultrasound scanning.
Methods
Peripheral blood lymphocytes were taken from the patients and cultured.G banding was done for all cases to facilitate individual chromosome identification,and if specific staining for certain portions of the chromosome was necessary,C banding was used.Routine evaluation of each case involved analysis of 30 random metaphase spreads.Three metaphases were photographed for purposes of karyotyping and saved in computer.When mosaicism was suspected during analysis,more than 50 metaphase spreads were analyzed;cell cultures were always repeated and more than 50 cells were scored.Karyotypes were described using ISCN2005 standard nomenclature of human chromosomes.
Statistical analysis
All the variables were coded as qualitative and introduced into a database for statistical analysis.A descriptive analysis was performed on the entire patient sample using frequency distributions and percentages for qualitative variables.The chi-square test was used to hypothesize the independence of crosstabulated variables.The difference was considered statistically significant when thePvalue was under 0.05.Statistical analyses were performed with the Predictive Analytics Sofeware.
RESULTS
Karyotype in patients with primary amenorrhea
The 340 individuals selected for this study were categorized into 6 groups according karyotype,including 46,XX group,X chromosome aberration group,mosaic X-Y group,X-autosome translocation group,autosome aberration group,and 46,XY group.Of 340 patients with primary amenorrhea,180 (52.94%) patients with normal female karyotype 46,XX and 160 (47.06%) patients with 37 kinds of chromosome abnormalities (Table 1).Of the 160 cases with chromosome abnormalities,105 (65.6%) with X chromosome aberration,45 (28.1%) with 46,XY,5 (3.2%)with autosome aberration,4 (2.5%) with mosaic X-Y,and 1(0.6%) with X-autosome translocation.
Relation of karyotype and clinical manifestations in patients with primary amenorrhea
Clinical manifestations in 340 patients with primary amenorrhea were primordial or absent uterus (n=326,95.9%),invisible secondary sex features (n=234,68.8%),little or absent ovary (n=213,62.6%),short stature(n=102,30.0%),cubitus valgus (n=59,17.4%),low posterior hairline (n=29,8.5%),learning difficulty (n=27,7.9%),and webbed neck (n=24,7.1%).The stature of the 46,XX patients with primary amenorrhea was 156.2±10.7 cm,X chromosome aberration patients was 142.7±8.6 cm,and 46,XY patients was 161.0±10.1 cm.The incidence of short stature in patients with X chromosome aberration (46%,69/150),was higher than that of 46,XX(9.44%,17/180) and 46,XY patients (6.67%,3/45;χ2=146.25,P=0.000).Five patients with deletion or breakpoint at Xp11.1-11.4 were short stature.
DISCUSSION
Karyotype and clinical features of patients with primary amenorrhea
Primary amenorrhea is often associated with anomalies of the sex and autosomal chromosome.In this study,180 patients with primary amenorrhea had normal female karyotype 46,XX.About 94% carriers of 46,XX showed dysgenetics,Turner Syndrome phenotypes.The pathogenisis of primary amenorrhea in 46,XX females is not very clear.Many researches have certified autosomal recessive disorders,micro deletions in X chromosome and concealing mosaic 45,X cell line undetected by cytogenetic technology affect ovarian differentiation and stature development.3The percentage of the Chinese patients with an abnormal karyotype varied from 35.2% to 58.6%4and that of our cohort was 47.06% (Table 1).It is necessary for the patients with primary amenorrhea to undergo cytogenetic analysis.We found the karyotype of 28.0% caseswith Turner Syndrome was pure 45,X and 49.1% cases with a 45,X mosaic cell line.The results in our study were similar to those of the previous study.5However,Elsheikhet al6reported the karyotype of 48% Turner Syndrome patients were pure 45,X and 18% cases showed 45,X mosaic cell line.This might explain the difference in Turner Syndrome mechanism between Chinese and Western patients.The loss or structural abnormality of X chromosome during cleavage division of a normal zygote might result in Turner Syndrome in Chinese,and the complete or partial deletion of X chromosome during embryo development might lead to Turner Syndrome in Western patients.
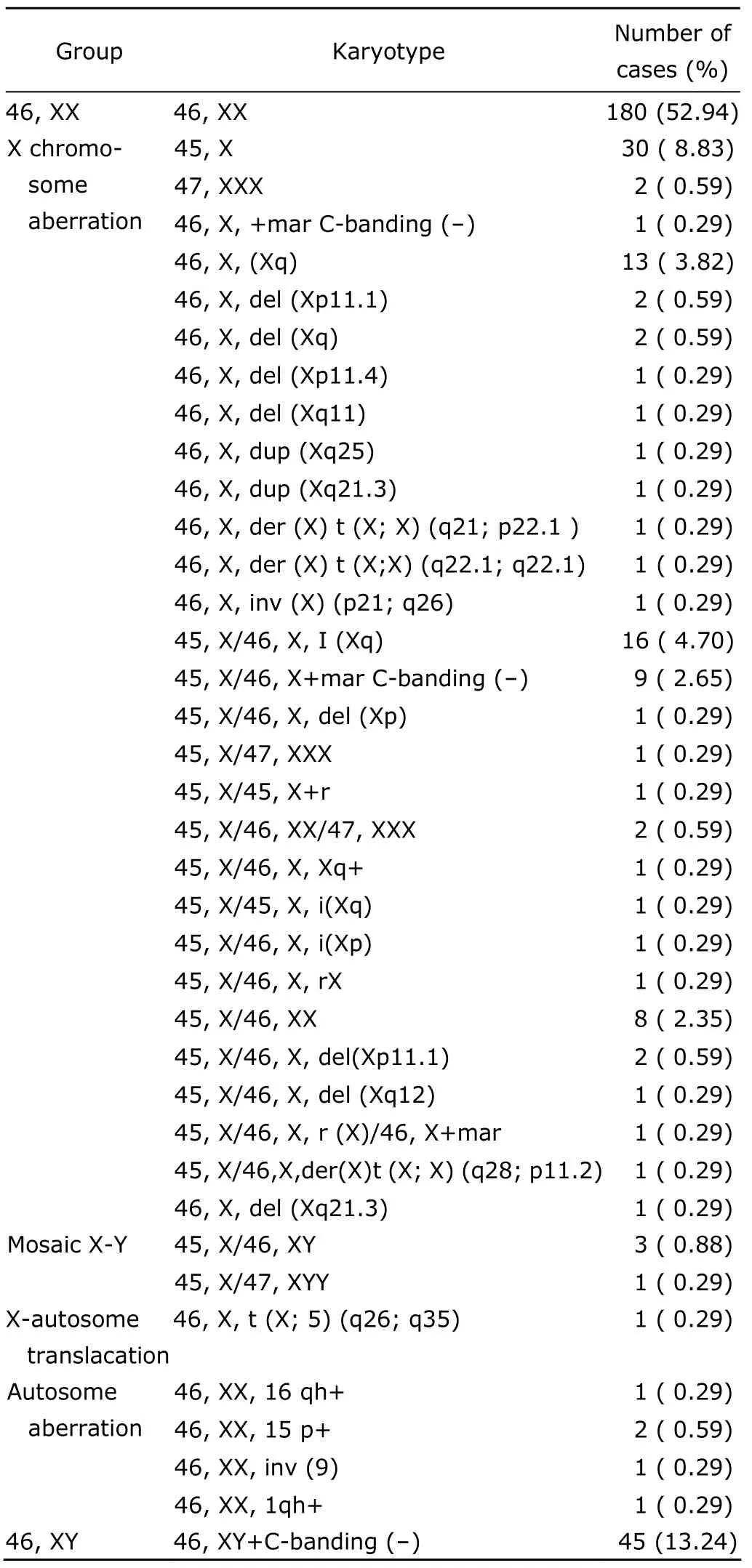
Table 1.Results of cytogenetic analysis of 340 patients with primary amenorrhea
Most patients in our study showed clinical signs of Turner Syndrome,including short stature,low posterior hairline,and ovarian digenesis.Especially those patients with structural alterations of the X chromosome,such as deletions,isochromosomes,rings and Xq segmental duplications all showed primary amenorrhea and almost gonad digenesis.It has been pointed out that about 95% of females with deletion in Xp11 showed primary or secondary amenorrhea,but the females with deletion in Xp22.3-Xpter had normal menstruation.The critical growth developmental gene SHOX was located at Xp11-Xp22.7The patients with deletion or breakpoint in Xp11.1-11.4 presented short stature in our study,so the integrity of this region was very important to growth development.Turner Syndrome is usually underdiagnosed in young girls with growth impairment,if these girls treated with growth hormone were an average of 5 cm taller and significantly less obese than untreated group.8
Small supernumerary marker chromosomes (sSMC)are extra,abnormal chromosomes whose origin can not typically be determined by conventional chromosomebanding techniques.SMC can be observed not only in a numerically normal ‘basic karyotype’,but also in numerically abnormal one like in a ‘Turner-syndrome karyotype’(sSMCT).sSMCTare very rare in the general population,however,they can be observed 45 and even 60 times more frequent in infertile and developmentally and/or mentally retarded patients,respectively.9We found 1 sSMC case,12 sSMCTor r(X) cases.All patients with sSMC,sSMCTor r(X)showed ovarian digenesis.The incidence of mental retardation or learning difficulties with sSMC,sSMCTor r(X)patients was almost 30%,which was higher than that of Turner Syndrome patients.The additional features can be partially explained by the status of X inactivation,size,origin and replication timing of the ring,genes affected by copy number variations,and the percentage of mosaics.The patients with development delay should undergo cytogenetic analysis,especially for cases of missing optimal growing stage.
The i (Xq) was present in mosaic or non-mosaic form and similar to individuals with Turner Syndrome in the study.It is not surprising because the classical mechanism for isochromosome formation,centromere misadvising,would result in an i (Xq) with no Xp material present.
We found two cases of Xq duplications.One patient with 46,X,dup (X) (q25) showed mental retardation and the other patient with 46,X,dup(X) (q21.3) showed normal mentality.Prevalence of Xq duplications remains unknown and cytogenetically visible duplication of Xq is rare.They more often implicate the distal Xq27-qter region.The most frequent manifestations found in these patients are short stature,developmental delay,facial dysmorphism,gonadal dysgenesis and mental retardation.The clinical manifestations of the chromosome imbalances vary depending on the X-inactivation patterns and on the gene content of the duplicated segment,10such as MECP2 gene in Xq28,which is the most important dosage-sensitive gene responsible for neurologic impairment in patients with duplications of the distal part of chromosome Xq.10
Y chromosome and primary amenorrhea
We found 28.1% cases with 46,XY and 3.8% cases with Y chromosome in Turner Syndrome patients in our study.Those patients showed pure gonadal dysgenesis and some patients had lower serum testosterone levels,which maybe have relationship with the mutations of sex-determining region Y (SRY),steroidogenic factor-1 (SF-1),and luteinizing hormone (LH) genes.11Many etiological factors can cause abnormal female fetal development leading to pure gonadal dysgenesis with 46,XY,such as X-linked recessive syndrome,autosome genetic disorders,SRY,DAX1,WT-1,SOX9,SF-1,NR5A1 gene mutations,et al.All 46,XY patients with pure gonadal dysgenesis in this study had normal or tall stature.The Y chromosome in Turner Syndrome patients is structurally abnormal showing deletions,inversions,dicentrics and ring forms.And this makes Y chromosome unstable,resulting in 45/XO karyotype.Some reported the incidences of tumors such as gonadoblastomas,dysgerminomas,and yolk sac tumors vary from 30% to 75% for all females with pure gonadal dysgenesis and from 7% to 10% for Turner Syndrome patients.12,13Because of the high risk of neoplastic transformation,it is generally advised that the dysgenetic gonads be surgically removed by gonadectomy as soon as the diagnosis is made.Y-located testis-specific protein encoded on Y (TSPY) and SRY genes are believed to be associated with gonadoblastomas and gonadal dysgerminomas.Recently more researchers recommended that gonadectomy should be considered for those patients.Y chromosome in 3%-6%cells often triggers development of gondoblastoma,especially in gonade,but Y mosaicism varies across the tissues.Thus the numbers of cells with Y chromosome are unable to be accurately identified.The studies on Turner women imply that only a small group of females with Y chromosome material develop gonadal tumors and the role of the Y chromosome in tissues of the Turner Syndrome patients remains a murky proposition.14So treatment of XY females still remain unanswered.
X-autosome translocation,chromosomal polymorphism and primary amenorrhea
X-autosome translocations [t(X;A)]are rare rearrangements estimated to occur in 1/10 000 to 3/10 000 live birth.15It belongs to special subgroup of reciprocal chromosome translocations because X chromosome inactivation can additionally affect the phenotype,as primary amenorrhea,spreading to the autosomal segment and/or generating functional imbalance.During 1997 to 2009,39 types of t (X;A) were reported and breakpoints at Xq22-27 in China.16One carrier of 46,X,t (X;5)(q26;q35) with ovarian dysgenesis and short stature reported in our study.The pattern of X-chromosome inactivation is usually associated with an abnormal phenotype and in about 95% of balanced t (X;A),and the normal X chromosome is inactivated in all cells.8It may be explained that interruption of the critical region in Xq26 causes many genes involving premature ovarian failure 1 (POF1) to escape inactivation,which leading to especial genesic phenotypes.
Five cases showed chromosomal polymorphism in our study,involving secondary constriction region of chromosomes 1 and 16,pericentric inversion of chromosomes 9,and satellite increases in chromosome 15.Wanget al17has pointed out that chromosomal polymorphisms affected reproductive functions and had relationship with abortion,still birth and infertility.
Generally,one of the main reasons of primary amenorrhea is chromosome abnormities,especially heterosome abnormalies.Patients with primary amenorrhea should undergo routine cytogenetic karyotyps examination.
1.Zhang MY,Li GG,Cai HD,et al.Sterility and reproductive endocrinology.2nd ed.Beijing∶Peking University Medical Press;2005.p.71-5.
2.Wang WP.Pediatrics.Beijing∶High Education Press;2004.p.327-31.
3.Modi D,Bhartiya D.Y chromosome mosaicism and occurrence of gonadoblastoma in cases of Turner syndrome and amenorrhoea.Reprod Biomed Online 2007;15∶547-53.
4.Li DM,Gan TH,Ou S,et al.Cytogenetic analysis of 115 patients with amenorrhea.Guangxi Med J 2009;31∶1124-5.
5.Zhao X,Shen GM,Feng Q,et al.Cytogenetic studies of 131 patients with primary amenorrhea (including three novel abnormal karyotypes).Hereditas 2008;30∶996-1002.
6.Elsheikh M,Dunger DB,Conway GS,et al.Turner’s syndrome in adulthood.Endocr Rev 2002;23∶120-40.
7.Zinn AR,Ross JL.Molecular analysis genes on Xp controlling Turner syndrome and premature ovarian failure(POF).J Semin Reprod Med 2001;19∶141-6.
8.McCarthy K,Bondy CA.Turner syndrome in childhood and adolescence.Expert Rev Endocrinol Metab 2008;3∶771-5.
9.Sheth F,Ewers E,Kosyakova N,et al.A small supernumerary marker chromosome present in a Turner syndrome patient not derived from X-or Y-chromosome∶a case report.Mol Cytogenet 2009;2∶22.
10.Sanlaville D,Schluth-Bolard C,Turleau C,et al.Distal Xq duplication and functional Xq disomy.Orphanet J Rare Dis 2009;4∶4.
11.Philibert P,Leprieur1 E,Zenaty D,et al.Steroidogenic factor-1 (SF-1) gene mutation as a frequent cause of primary amenorrhea in 46,XY female adolescents with low testosterone concentration.Reprod Biol Endocrinol 2010;8∶28.
12.Jorgensen PB,Kjartansdottir KR,Fedder J,et al.Care of women with XY karyotype∶a clinical practice guideline.Fertil Steril 2010;91∶105-13.
13.Behtash N,Karimi Zarchi M.Dysgerminoma in three patients with Swyer syndrome.World J Surg Oncol 2007;5∶71-6.
14.Premi S,Srivastava J,Panneer G,et al.Startling mosaicism of the Y-chromosome and tandem duplication of the SRY and DAZ genes in patients with Turner Syndrome.PLoS One 2008;3∶e3796.
15.Binkert F,Spreiz A,H?ckner M,et al.Parental origin and mechanism of formation of a 46,X,der(X)(pter-->q21.1∶∶p11.4-->pter)/45,X karyotype in a woman with mild Turner syndrome.Fertil Steril 2010;94∶350.e12-5..
16.Yu XY,Huang YH,Song JP.et al.Cytogenetics analysis of 287 patients with amenorrhea.Chin J Reprod Health 2009;20∶50-1.
17.Wang XR,Deng JX,Li JJ.et al.The relationship between clinical outcomes of reproductive abnormalities and chromosome polymorphism.Hereditas 2007;29∶1362-6.
 Chinese Medical Sciences Journal2011年3期
Chinese Medical Sciences Journal2011年3期
- Chinese Medical Sciences Journal的其它文章
- Sclerosing Cholangitis after Transcatheter Arterial Chemoembolization:a Case Report
- Sutureless Intestinal Anastomosis with a Novel Device of Magnetic Compression Anastomosis△
- Choroidal Tuberculoma in an ImmunocompetentYoung Patient
- Influence of Deleted in Colorectal Carcinoma Gene on Proliferation of Ovarian Cancer Cell Line SKOV-3 In Vivo and In Vitro
- Serum HIF-1α and VEGF Levels Pre-and Post-TACE in Patients with Primary Liver Cancer
- Effect of Multiple Coatings of One-step Self-etching Adhesive on Microtensile Bond Strength to Primary Dentin
