Iatrogenic pneumopericardium after therapeutic pericardiocentesis for pericardial effusion: a case report
Yang-Yang ZHU, Ting-Ting WANG, Xiao-Na XU, Jing-Yue XU, Hua-Ying FU, Guang-Ping LI, Tong LIU, Chang-Le LIU?
Tianjin Key Laboratory of Ionic-Molecular Function of Cardiovascular Disease, Department of Cardiology, Tianjin Institute of Cardiology, Second Hospital of Tianjin Medical University, Tianjin, China
Pneumopericardium refers to the presence of air inside the pericardial cavity, which is a rare entity that has been reported clinically.Toledo,et al.[1]classified the causes of pneumopericardium into four categories: iatrogenic, pericarditis, fistula formation between the pericardium and adjacent hollow organs, and trauma.Until now, there have been only a limited number of reports in the literature[2–4]regarding pneumopericardium caused by the need for therapeutic pericardiocentesis due to pericardial effusion.These may be attributed to either a direct pleural-pericardial connection or the entry of air into the pericardial drainage system.[3,5,6]In most cases, iatrogenic pneumopericardium can be absorbed by itself and does not require special treatment.[5]However, in some patients with hemodynamic instability, life-threatening pericardial tamponade may occur if tension pneumopericardium occurs.[4]Therefore, timely identification and urgent treatment are required.Herein, we discuss a case of iatrogenic pneumopericardium diagnosed by chest computed tomography(CT) and transthoracic echocardiography (TTE) after pericardiocentesis due to pericardial effusion.This clinical case analysis aims to summarize the etiology, clinical characteristics, and diagnosis and treatment methods of pneumopericardium to improve the understanding of this rare disease.
We present the case of a 69-year-old male who had been experiencing palpitations for over 10 years, progressive worsening of exertional dyspnea for the past month, and bilateral lower limb edema.A pre-admission outpatient chest CT scan conducted in July 2022 showed a large fluid shadow in the pericardium, indicating pericardial effusion (Figure 1).On physical examination, his hemodynamic status was stable (blood pressure: 134/76 mmHg, pulse rate: 71 beats/min, respiratory rate: 18 per min, and body temperature: 36.5 °C).Heart auscultation revealed a weak heart sound.Six hours after being admitted, the patient experienced a sudden loss of consciousness following urination, accompanied by cyanosis of the lips and absence of arterial pulsation.Fluid replenishment and dopamine were administered to increase blood pressure, and the patient’s consciousness improved after receiving cardiopulmonary resuscitation.At the time of assessment, the patient’s blood pressure was 78/56 mmHg, and heart rate was 88 beats/min.A bedside TTE showed substantial peripheral pericardial effusion, suggesting a cardiac tamponade caused by the large pericardial effusion.An immediate pericardiocentesis was performed, and the puncture point was identified between the xiphoid process and the costal arch edge.Using the Seldinger technique, percutaneous pericardiocentesis was carried out to drain the pericardial effusion.A total of 200 mL of clear yellow fluid was extracted, and the pericardial catheter was fixed to the skin.A vacuum container was used to connect to the closed drainage system under negative pressure.The pericardial effusion was then sent to the laboratory.The laboratory analysis of the pericardial effusion showed a predominance of monocytes, and the leukocyte count was normal.Lactate dehydrogenase was slightly elevated at 395.6 U/L.No malignant tumor cells were found in cytological examination, and acid-fast bacilli and other microbial smears and cultures were negative.The laboratory tests conducted on admission showed normal white blood cell count and percentage of monocytes.Troponin I was within the normal range, while N-terminal-B-type natri-uretic peptide precursor increased to 317.3 ng/L.The patient’s thyroid function was abnormal, with significant decreases in free thyroxine and triiodothyronine, and an increase in thyrotropin.Based on the patient’s clinical symptoms and laboratory tests, we consider the pericardial effusion to be caused by hypothyroidism.Levothyroxine tablets and methylprednisolone were administered for symptomatic treatment.
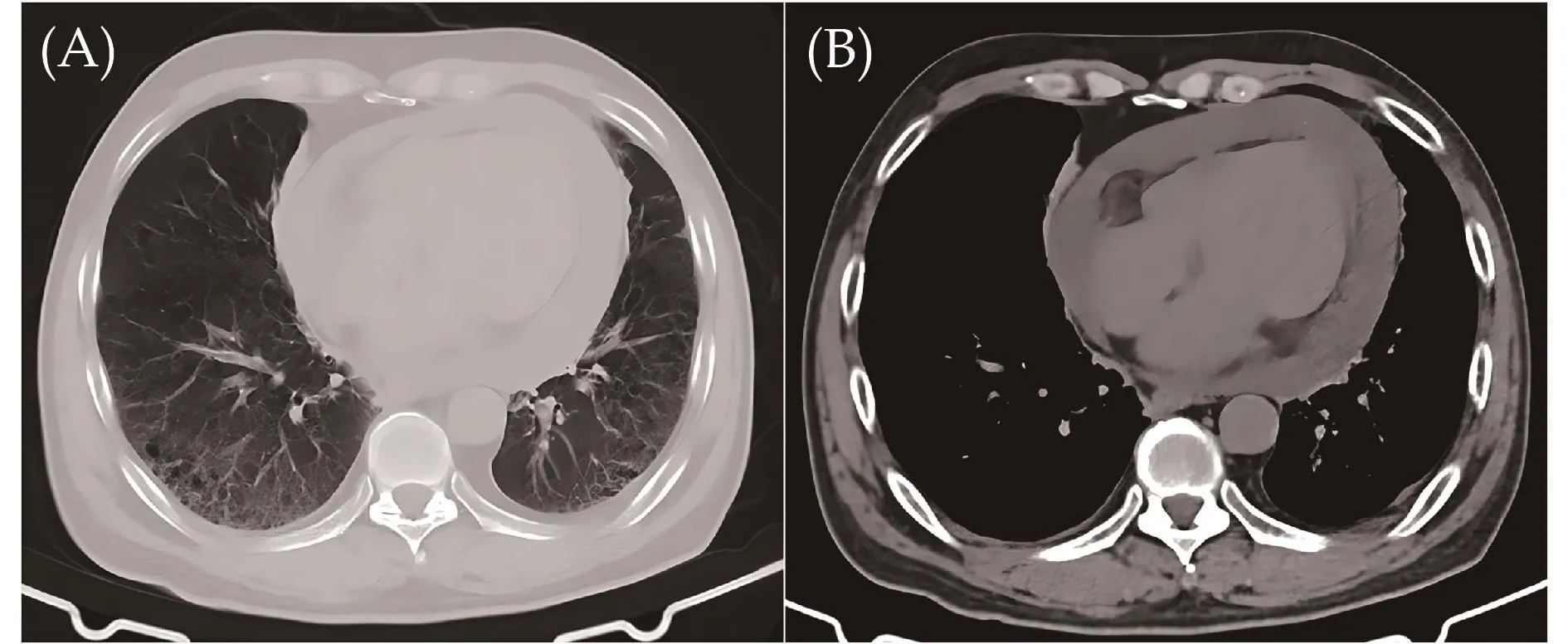
Figure 1 Prior to admission, an outpatient chest CT revealed a significantly enlarged cardiac boundary and widely spaced parietal and visceral layer pericardium.In addition, a fluid density collection involving the heart was observed, suggesting the presence of pericardial effusion, as seen in the axial CT slice viewed at lung parenchymal (A) and mediastinal (B) window settings.CT: computed tomography.
Two days post-operation, the patient reported significant relief in chest tightness and dyspnea symptoms compared to before admission.Physical examination revealed stable vital signs.However, upon re-examination of the chest CT, it was unexpectedly observed that a significant amount of gas density shadow was present in the pericardium, and the effusion shadow was not as clearly shown as before (Figure 2).A TTE was performed, revealing a small amount of pericardial effusion with several small sparkling echogenic spots swirling in the pericardial sac suggestive of micro air bubbles, and a decreased ejection fraction of 48% (Figure 3).The TTE also revealed left atrial dilation (end-diastolic diameter of 41.4 mm), and inferior and posterior wall motion hypokinesis.No evidence of tension pericardial effusion was observed.Due to the patient’s stable hemodynamic status and absence of specific discomfort symptoms, conservative treatment was administered while closely monitoring the patient’s condition.The patient was discharged from the hospital a few days later.A follow-up outpatient chest CT scan conducted a month after discharge revealed a significant reduction in the pericardial gas density shadow (Figure 4).
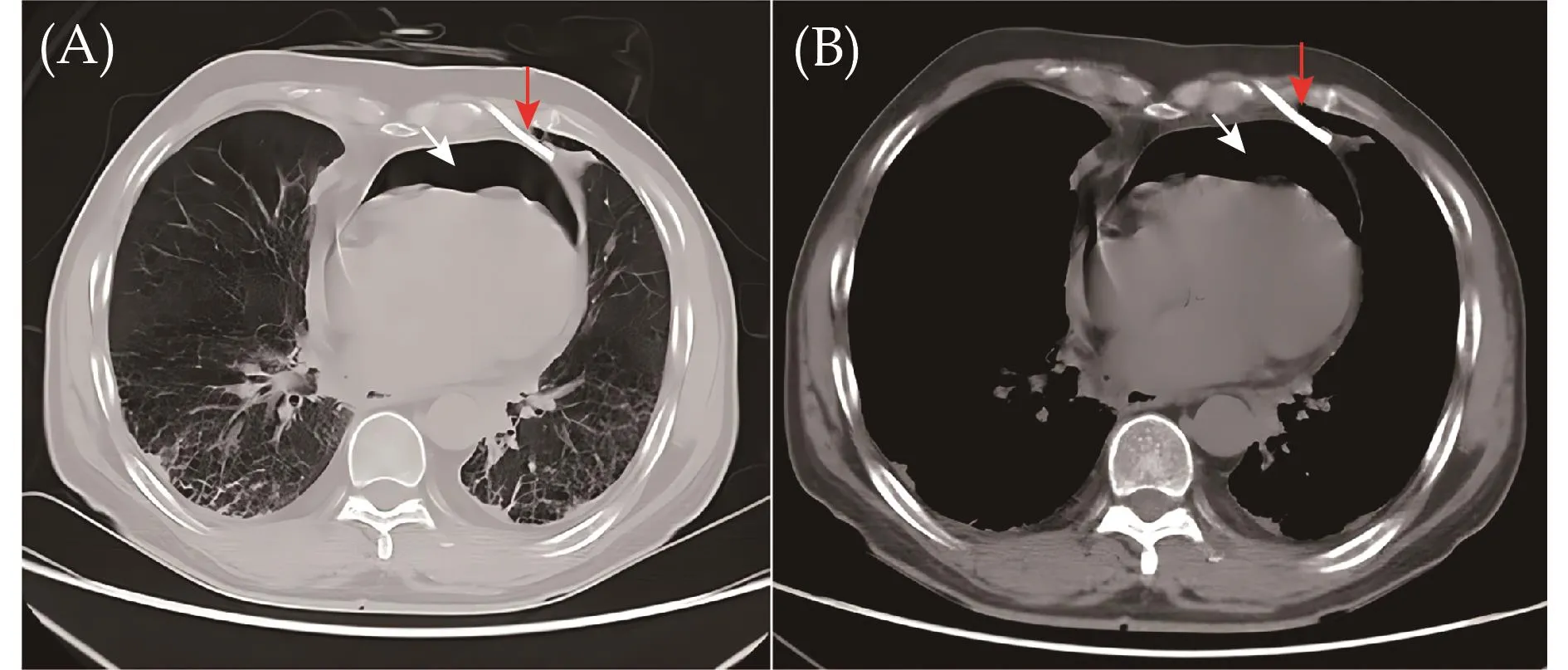
Figure 2 Upon re-examination of the postoperative chest CT, an unexpected amount of pericardial gas density shadow (white arrows) was observed in the axial CT slice viewed at both lung parenchymal (A)and mediastinal (B) window settings.The position of the drainage tube in the postoperative chest CT image is shown by the red arrows.CT: computed tomography.
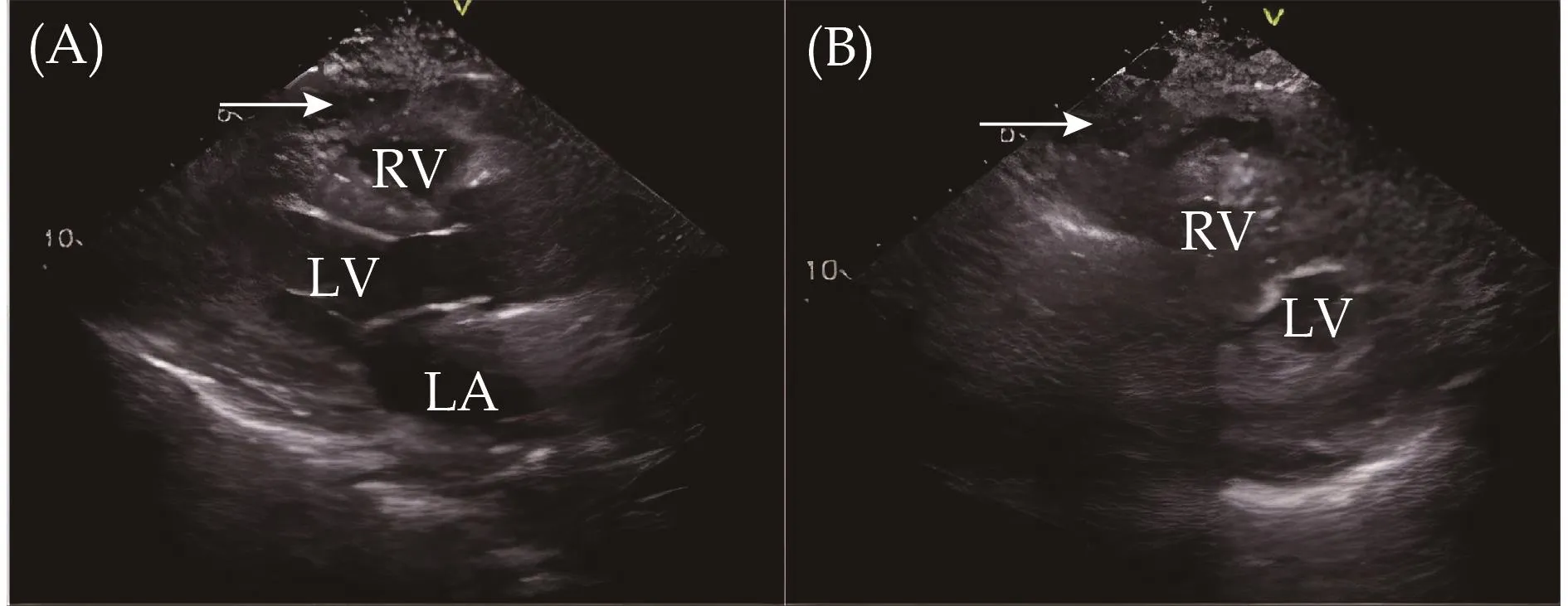
Figure 3 Transthoracic echocardiography revealed a small number of microbubbles (white arrows) in pericardial effusion in the left ventricular long axis section (A) and short axis section (B).LA: left atrium; LV: left ventricle; RV: right ventricle.
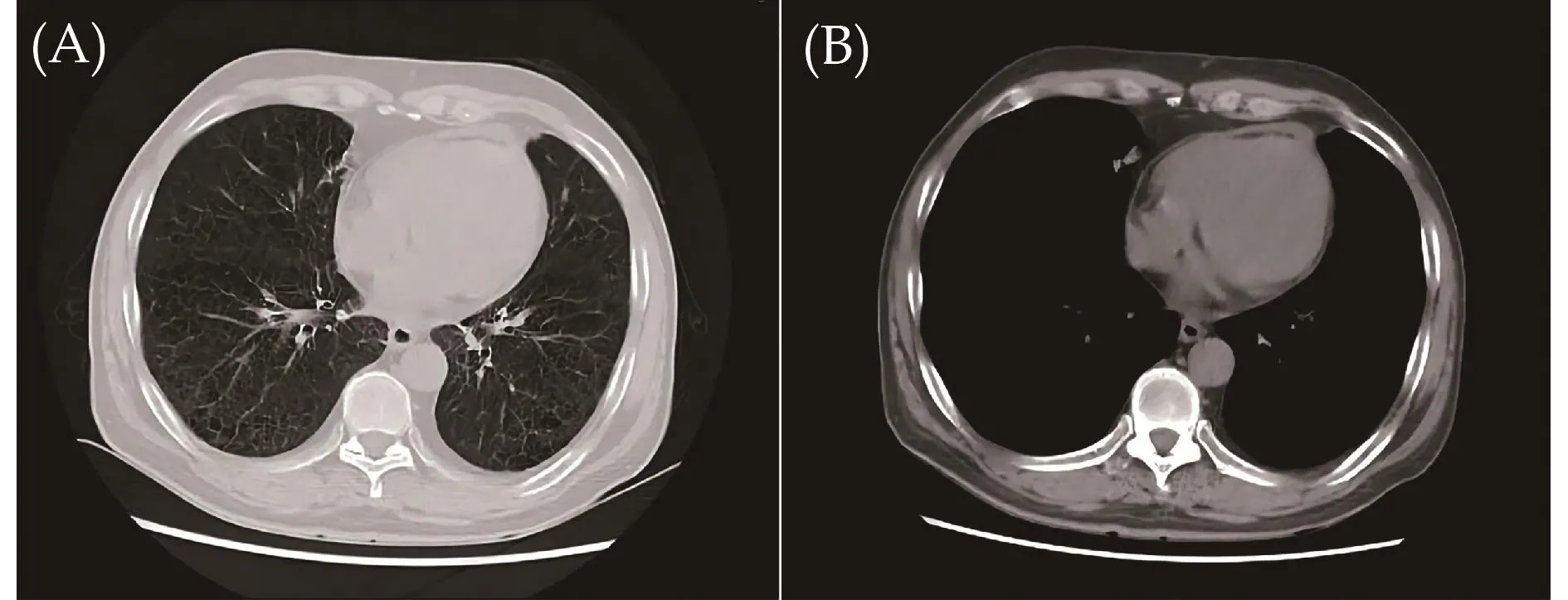
Figure 4 Chest CT scan of outpatient follow-up revealed that a basically normal cardiac boundaries and normal spaced parietal and visceral layer pericardium and illustrated that the pericardial gas density shadow had almost disappeared in the axial CT slice viewed at lung parenchymal (A) and mediastinal (B) window settings compared with Figure 2.CT: computed tomography.
Pneumopericardium is characterized by the presence of air within the pericardial cavity.The patient in this case presented to the hospital with symptoms of palpitation and shortness of breath.Prior to admission, the patient underwent outpatient chest CT and echocardiography, which revealed a significant amount of pericardial effusion.After admission, the patient experienced a sudden loss of consciousness, decreased blood pressure,and disappearance of large artery pulse.Cardiopulmonary resuscitation was successfully performed, and pericardial puncture was subsequently carried out to extract 200 mL of yellow clear fluid, confirming that the cardiac arrest was caused by pericardial tamponade due to a large amount of pericardial effusion.The patient was thenfitted with a pericardial effusion drainage tube.Upon reexamination of the chest CT, it was observed that a significant amount of gas density shadow was present in the pericardium, and the effusion shadow was not as clearly shown as before.The difference in the results of the two CT reports before and after pericardial puncture suggests that pneumopericardium occurred during or after therapeutic pericardiocentesis.In recent years, iatrogenic pneumopericardium has been reported in a few studies,[6–11]mainly related to various clinical invasive procedures such as thoracentesis,[10]pericardiocentesis,[11]pacemaker implantation[12]and radical resection of gastric and esophageal cancer.[13]The occurrence can be attributed to either direct pleural-pericardial connection or air leakage to the pericardial drainage system.[3,5,6]For this patient, based on the position of the drainage tube observed on postoperative chest CT imaging (Figure 2, red arrows), the accumulation of pericardial gas may have been caused by adjacent lung tissue injury during the puncture, resulting in a direct pleural-pericardial connection.It has been reported that during the puncture procedure, if the patient takes a deep breath when the syringe is removed from the center of the puncture needle to extract the guide wire, external air may be sucked into the pericardial cavity from the center of the needle,[6]resulting in iatrogenic pneumopericardium.For this patient, this situation cannot be ruled out.At the same time, it cannot be completely ruled out that the drainage tube may have caused air to enter the pericardial cavity.To prevent this complication, it is crucial to ensure correct needling insertion direction and appropriate depth, avoid strenuous aspiration or coughing,close all drainage system connections at the time of puncture, and apply surgical gel to the skin surrounding the drainage to create a seal.[2,14]Performing pericardiocentesis under the guidance of bedside echocardiography can also significantly reduce the risk of this complication.
The clinical manifestations of pneumopericardium are diverse and can include chest tightness, palpitation, shortness of breath, and fatigue.Chest CT scan is the main diagnostic tool for pneumopericardium.[5]In this case, postpericardiocentesis chest CT scan showed obvious pneumopericardium (Figure 2), compared to the pre-pericardiocentesis image of pericardial effusion (Figure 1).TTE can show two characteristic signs of pneumopericardium: the “air gap sign” and the “swirling bubbles sign”.The former refers to the periodic disappearance of the heart shape, which is related to the circulation of air in the pericardium, while the latter refers to the continuous movement of small bubbles in the pericardial cavity due to cardiac activity.[2]The clinical manifestation of pneumopericardium is generally related to the amount and speed of gas accumulation.[4,12,15]If there is a large amount of gas in the pericardial cavity in a short time,pericardial tamponade can occur rapidly, leading to a decrease in ventricular diastolic filling and a significant decrease in cardiac output.This can result in shock symptoms such as loss of consciousness and decreased blood pressure in a short time.Therefore, pericardiocentesis is needed to quickly restore hemodynamic stability.In the absence of acute and life-threatening tension pericardial pneumatosis, a vigilant wait for spontaneous absorption of air under close monitoring can be considered.[12,15]In this case, although the chest CT indicated that the gas accumulation was large, the patient’s hemodynamics were relatively stable.Therefore, no additional treatment was given for the patient’s pneumopericardium.The followup results of CT in the outpatient clinic confirmed that the patient’s pneumopericardium had basically disappeared.We remind that pneumopericardium accumulation can be naturally absorbed over time, but it requires close monitoring and observation.[5,15]When suspicious symptoms occur, the possibility of cardiac tamponade should be ruled out urgently and the corresponding clinical treatment such as pericardiocentesis or surgical decompression should be performed promptly.[5]
In conclusion, iatrogenic pneumopericardium is a rare yet potentially life-threatening complication of pericardiocentesis.Diagnose can be made by imaging examinations such as chest CT and TTE.Pneumopericardium presents with a range of clinical symptoms, from asymptomatic cases to those with hemodynamic instability and pericardial tamponade.Although most cases resolve spontaneously, some require urgent intervention to prevent further complications.Our reported case emphasizes the importance of considering pneumopericardium as a possible complication of pericardiocentesis, and highlights the significance of early recognition and management to improve patient outcomes.This novel case draws attention to the occurrence and clinical significance of pneumopericardium.By highlighting this uncommon complication,healthcare professionals can become more aware of its possibility, and appropriate measures should be taken to minimize the occurrence of this complication.When managing patients who have undergone pericardiocentesis,it is essential to consider pneumopericardium in the diffe-rential diagnosis.A multidisciplinary approach, involving radiologists, cardiologists, and cardiac sonographers,is crucial for optimal management of this rare condition.Further research is necessary to identify risk factors for developing pneumopericardium after pericardiocentesis and establish guidelines for its prevention and management.
ACKNOWLEDGMENTS
This study was supported by the Tianjin Key Medical Discipline (Specialty) Construction Project (TJYXZDXK-029A).All authors had no conflicts of interest to disclose.
 Journal of Geriatric Cardiology2023年6期
Journal of Geriatric Cardiology2023年6期
- Journal of Geriatric Cardiology的其它文章
- Status of cardiovascular disease in China
- Unraveling the mechanisms of a giant coronary sinus
- Target versus sub-target dose of renin–angiotensin system inhibitors on survival in elderly patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis
- Outcomes of catheter-directed thrombolysis versus systemic thrombolysis in the treatment of pulmonary embolism: a metaanalysis
- Nocturnal hypertension and riser pattern are associated with heart failure rehospitalization in patients with heart failure with preserved ejection fraction
- Down-regulation of the Smad signaling by circZBTB46 via the Smad2-PDLIM5 axis to inhibit type I collagen expression
