Outcomes of catheter-directed thrombolysis versus systemic thrombolysis in the treatment of pulmonary embolism: a metaanalysis
Huang-Tai MIAO, Ying LIANG, Xiao-Ying LI, Xiao WANG, Hui-Juan ZUO, Zhe-Chun ZENG, Shao-Ping NIE,?
1.Center for Coronary Artery Disease, Beijing Anzhen Hospital, Capital Medical Universisty, Beijing, China; 2.Emergency& Critical Care Center, Beijing Anzhen Hospital, Capital Medical University, Beijing, China; 3.Department of Health Care for Cadres, Beijing Jishuitan Hospital, Beijing, China; 4.Department of Clinical & Community Cardiovascular Disease Prevention, Beijing Institute of Heart Lung and Blood Vessel Disease, Beijing Anzhen Hospital, Capital Medical University, Beijing, China
ABSTRACT OBJECTIVE To evaluate the safety and efficacy of catheter-directed thrombolysis (CDT) versus systemic thrombolysis (ST) in the treatment of pulmonary embolism (PE).METHODS The Cochrane Library, PubMed, and Embase databases were searched to collect the literature on the comparison of the results of CDT and ST in the treatment of PE from the beginning of their records to May 2020, and meta-analysis was performed by STATA software (version 15.1).Using standardized data-collection forms, the authors screened the studies and independently extracted data, and assessed the quality of the studies using the Newcastle-Ottawa Scale for cohort studies.Cohort studies that examined the following results were included in the current study: in-hospital mortality, all-cause bleeding rate, gastrointestinal bleeding rate, intracranial hemorrhage rate, the incidence of shock, and hospital length of stay.RESULTS A total of eight articles, with 13,242 participants, involving 3962 participants in the CDT group and 9280 participants in the ST group were included.CDT compared with ST in the treatment of PE can significantly affect in-hospital mortality rate [odds ratio (OR) = 0.41, 95% CI: 0.30–0.56, P < 0.05], all-cause bleeding rate (OR = 1.20, 95% CI: 1.04–1.39, P = 0.012), gastrointestinal bleeding rate (OR = 1.43, 95% CI: 1.13–1.81, P = 0.003), the incidence of shock (OR = 0.46, 95% CI: 0.37–0.57, P < 0.05), and hospital length of stay [standard mean difference (SMD) = 0.16, 95% CI: 0.07–0.25, P < 0.05].However, there was no significant effect on intracranial hemorrhage rate in patients with PE (OR = 0.70, 95% CI: 0.47–1.03, P = 0.070).CONCLUSIONS CDT is a viable alternative to ST in the treatment of PE, as it can significantly reduce in-hospital mortality rate,all-cause bleeding rate, gastrointestinal bleeding rate, and incidence of shock.However, CDT may prolong hospital length of stay to a certain extent.Further research is needed to evaluate the safety and efficacy of CDT and ST in the treatment of acute PE and other clinical outcomes.
Pulmonary embolism (PE) is a significant cause of cardiovascular death, ranking third after myocardial infarction and stroke.[1]About 25% of sudden death patients were found PE at autopsy.Current guidelines recommend that thrombolytic therapy should be mainly used in patients with hemodynamic instability (IIa); however, for patients with intermediaterisk PE (right ventricular dysfunction or severe myocardial necrosis), thrombolytic therapy is less recommended (IIb).[2]Systemic thrombolysis (ST) treatment has been used to save patients with high-risk PE,[3,4]however,it is still controversial whether ST is used in the treatment of patients with intermediate-risk PE.[5,6]Despite of smallscale evidence supporting the safety and efficacy of catheter-directed thrombolysis (CDT), CDT has been used in the treatment of patients with intermediate- and high-risk PE because it can deliver thrombolytic drugs directly to blood clots, and reduce the total delivery dose and bleeding complications.At present, most of the literature about the safety and efficacy of CDT is limited to small-scale observational studies.Therefore, the evaluation of clinical outcomes including intracranial hemorrhage, massive hemorrhage, and mortality in this literature may be lack of authority.Therefore, before CDT is widely used in PE,there is an urgent need for evidence about the safety of CDT.The purpose of this study is to obtain the safety comparison of CDT and ST in the treatment of PE patients in conjunction with current small-scale studies, to guide clinical diagnosis and treatment.
METHODS
Before the start of the study, we developed and followed a comprehensive protocol and data collection tool that followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations.The study was a retrospective analysis of published research literature only and no humans were involved.Hence, it was exempt from institutional review board approval.
Search Strategy
The Cochrane Library, PubMed, and Embase databases were searched to collect literature on the comparison of the results of CDT and ST in the treatment of PE with no start date to May 2020.Search term: catheter-directed thrombolysis, catheter-directed intervention, catheterdirected therapy, local thrombolysis, systemic thrombolysis, systemic thrombolytic therapy, systemically administered, systemic administration, pulmonary embolism, pulmonary thromboembolisms, etc.The search strategy of literature is shown in Table 1.

Table 1 Search strategy of literature.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) the patients included were those with PE whose diagnostic criteria were clearly described in the literature; (2) the study type was cohort or randomized controlled trial (RCT) study;and (3) the language is limited to Chinese and English.We performed a comprehensive literature search to identify RCTs and cohort studies related to CDT or ST in the treatment of PE from the beginning of available records until May 2020.
The exclusion criteria were as follows: (1) duplicate published studies; (2) no full text; (3) experiments on animals or review articles; and (4) editorials, comments, case studies, and letters to the editor were excluded.The definition of exposure is quite different from that of most literature that were excluded.
Study Selection
Two authors independently reviewed abstracts of all relevant studies resulting from the initial search.In cases of disagreement, a review of the full article will be determined by a third reviewer.The full manuscript of each study passing the relevance screen was independently conducted by two authors.In cases of disagreement, a third reviewer determined inclusion.Data abstraction was implemented using a standard data-collection form for each study identified for final inclusion.
Quality Assessment
The quality of cohort studies was examined using the Newcastle-Ottawa Scale (NOS).NOS included four items of “research object selection” (4 points), “comparability between groups” (2 points), and “outcome measurement” (3 points).The full score of NOS was 9 points.High-quality literature was classified as ≥ 7 points and low-quality literature was classified as < 7 points.
Statistical Analysis
STATA software (version 15.1) was used to analyze the data.Odds ratio (OR) was used as the effective index for counting data, standard mean difference (SMD) was selected for continuous variables, and 95% CI was used for interval estimation.If the heterogeneity testP-value≥ 0.1,I2≤ 50%, it indicates that the studies are homogeneous, and the fixed effect model is used for combined analysis; IfP-value < 0.1,I2> 50%, it indicates that there is heterogeneity between studies.Sensitivity analysis or subgroup analysis is used to find the source of heterogeneity.If the heterogeneity is still large, the random effect model is used or the results are discarded and the descriptive analysis is used.When more than 10 articles were included in a single outcome index, the publication bias of each index was analyzed by funnel plot and egger’s bias test.
RESULTS
Study Identification
A total of 333 articles were initially identified from the Cochrane Library, PubMed, and Embase databases.After excluding repetitive literature, 176 literature were obtained.After excluding reviews, systematic reviews, animal experiments, and case reports, 127 articles were obtained.After reading the abstract, 12 articles were obtained after excluding the articles whose contents were inconsistent and whose data could not be extracted.After full text browsing, the articles with inconsistent indicators were excluded, and finally, eight articles were obtained for this meta-analysis.
Basic Information
The basic information of the included literatures is shown in Table 2.
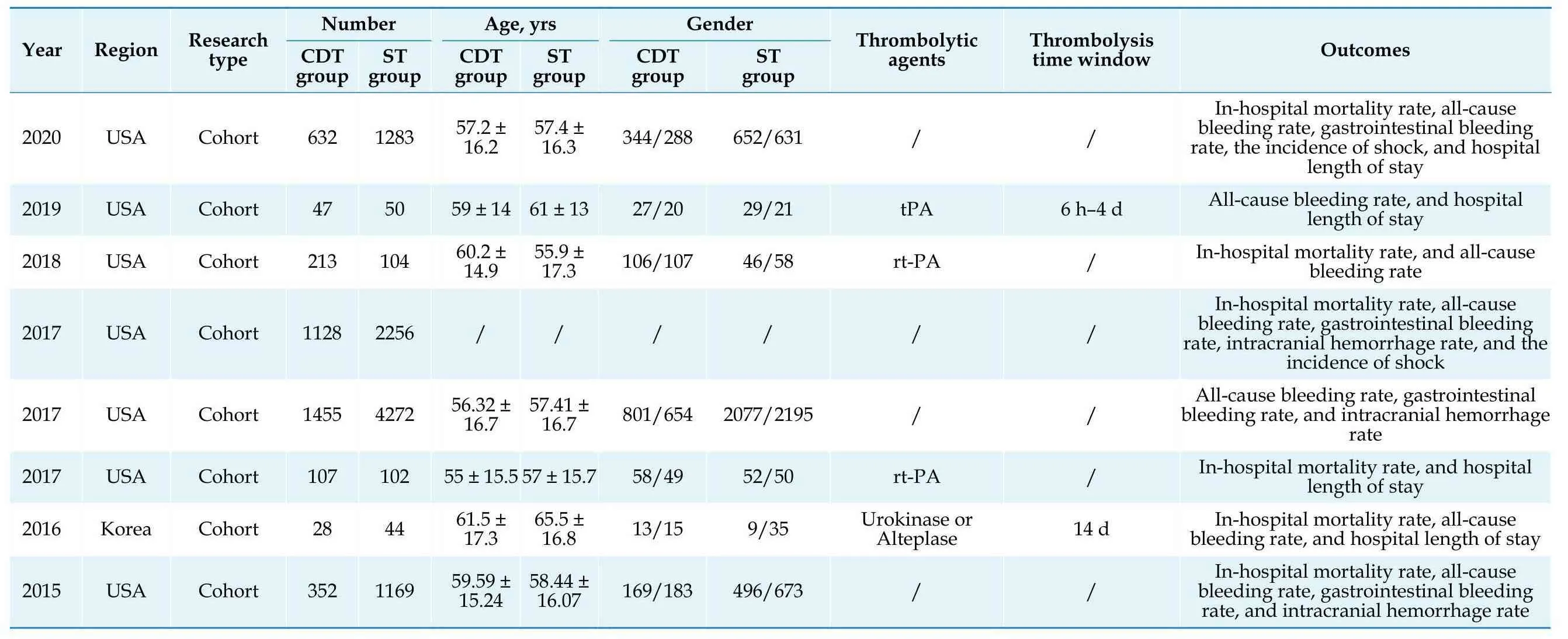
Table 2 Basic informationof literature.
Literature Quality Evaluation
All eight included articles were cohort studies, and their quality was evaluated using the NOS scale.The NOS scores of the included literatures were more than or equal to 7, and the quality of the literatures met the requirements (Table 3).
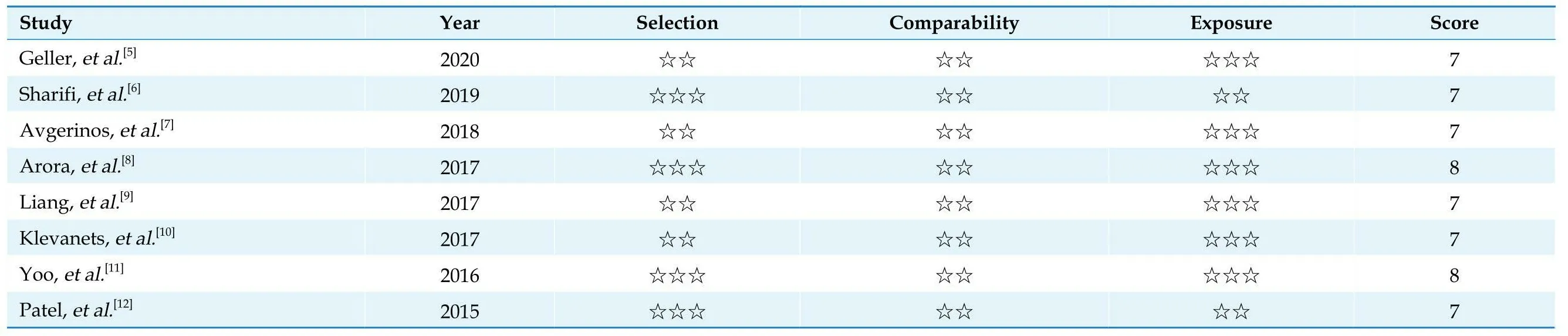
Table 3 Evaluationof literature quality.
Results of Meta-analysis
In-hospital mortalityThere was slight heterogeneity in the heterogeneity test of six studies (I2= 48.1%,P=0.086) (Figure 2), and no literature that had a great impact on the results was found by sensitivity analysis (Figure 8); so the combined random effect (OR = 0.41, 95% CI: 0.30–0.56,P< 0.05), the difference was statistically significant.These results indicate that catheter directed thrombolysis can significantly reduce the in-hospital mortality rate.
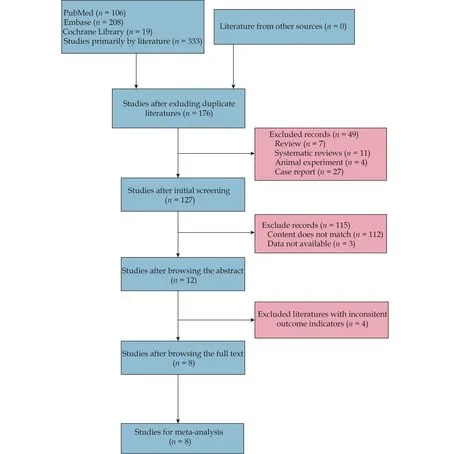
Figure 1 Flow chart of literature screening.
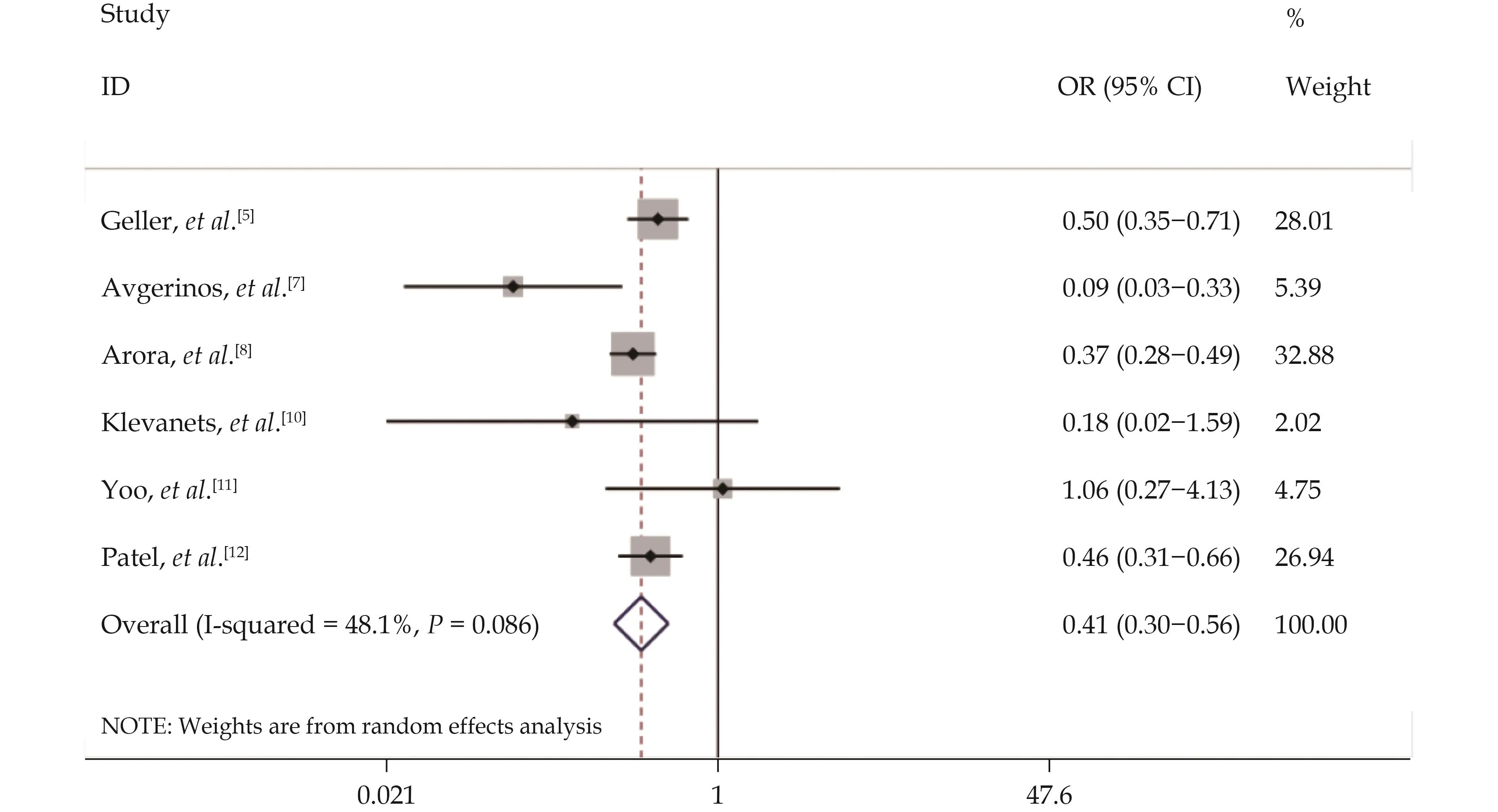
Figure 2 Comparative forest plot of in-hospital mortality rate between catheter-directed thrombolysis and systemic thrombolysis for pulmonary embolism.
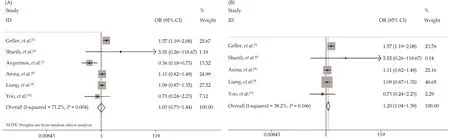
Figure 3 Forest plot of all cause bleeding rate comparison between catheter-directed thrombolysis and systemic thrombolysis in the treatment of pulmonary embolism (A, before sensitivity analysis) and (B, after sensitivity analysis).
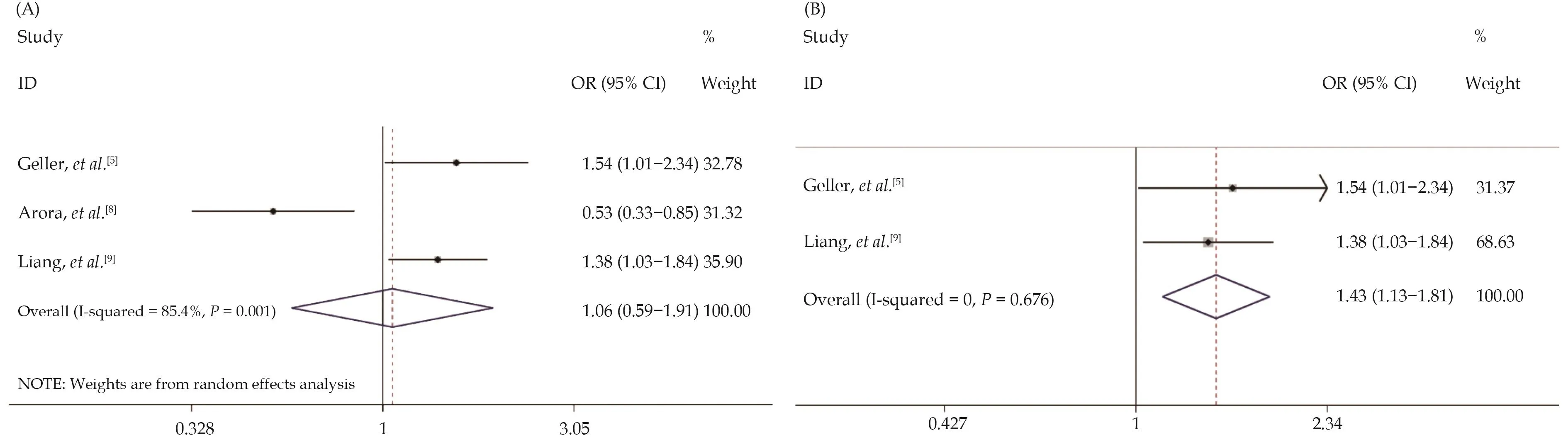
Figure 4 Forest plot of gastrointestinal bleeding rate comparison between catheter-directed thrombolysis and systemic thrombolysis in the treatment of pulmonary embolism (A, before sensitivity analysis) and (B, after sensitivity analysis).
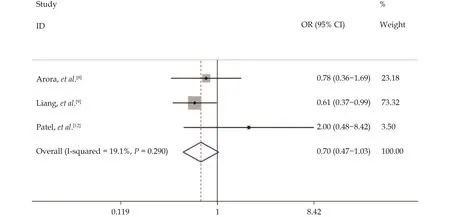
Figure 5 Forest plot of comparison of intracranial hemorrhage rate between catheter-directed thrombolysis and systemic thrombolysis in the treatment of pulmonary embolism.
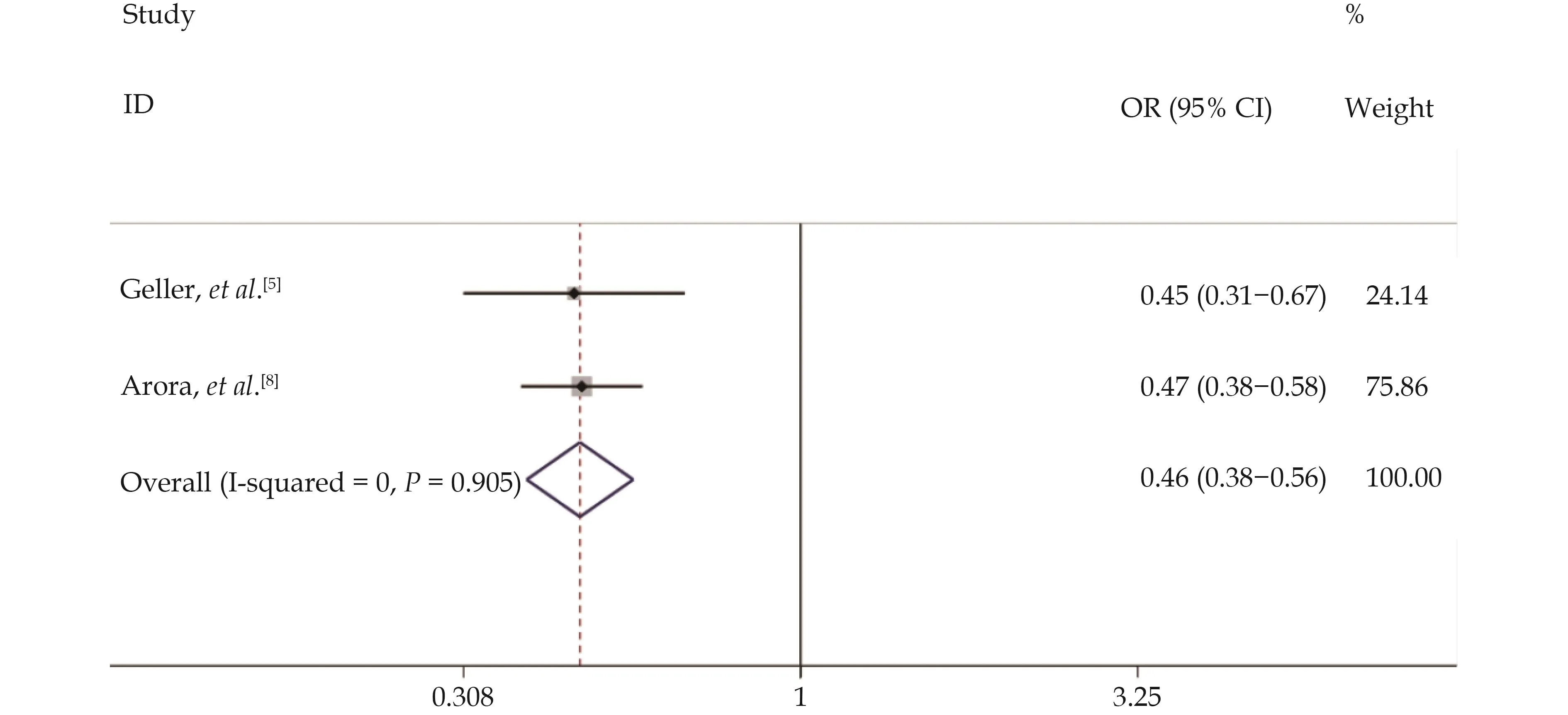
Figure 6 Forest plot of shock incidence in catheter-directed thrombolysis versus systemic thrombolysis for pulmonary embolism.
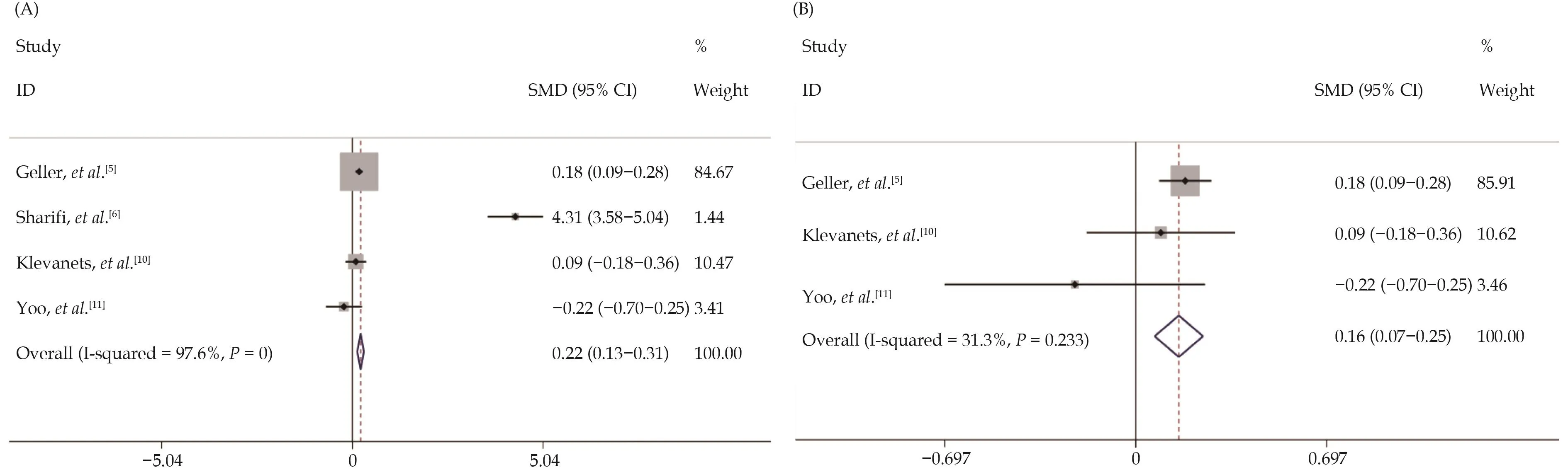
Figure 7 Forest plot of length of hospital stay for catheter-directed thrombolysis versus systemic thrombolysis for pulmonary embolism (A, before sensitivity analysis) and (B, after sensitivity analysis).
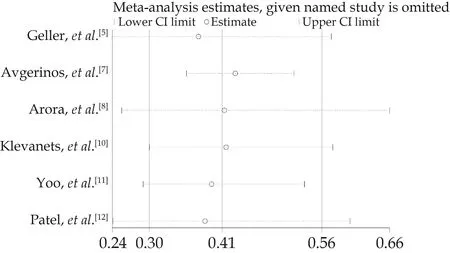
Figure 8 Sensitivity analysis of in hospital mortality rate comparison between catheter-directed thrombolysis and systemic thrombolysis in the treatment of pulmonary embolism.
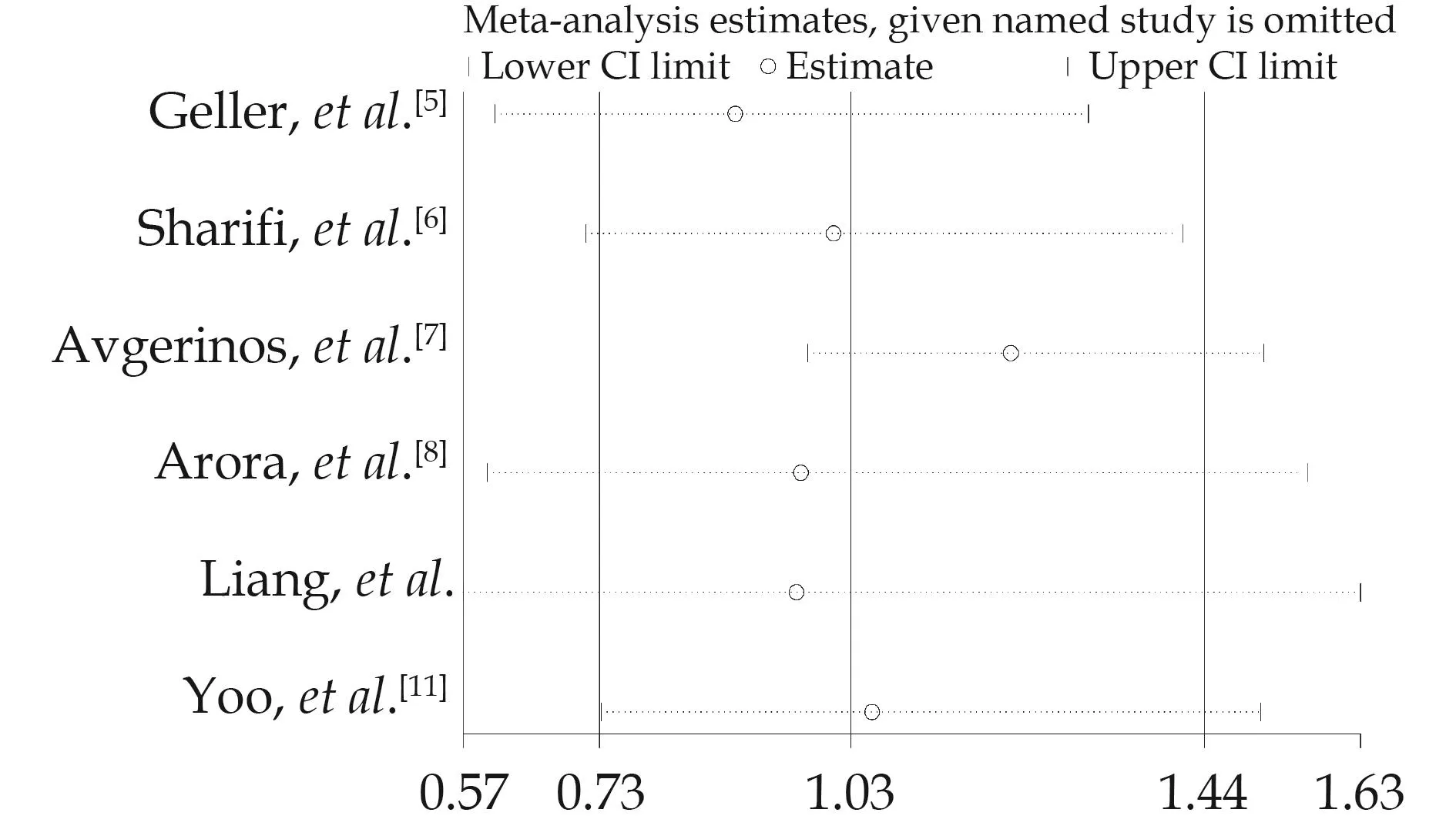
Figure 9 Sensitivity analysis of all-cause bleeding rate comparison between catheter-directed thrombolysis and systemic thrombolysis in pulmonary embolism.
All-cause bleeding rateThere was obvious heterogeneity in the heterogeneity test of six studies (I2= 71.2%,P= 0.004) (Figure 3A), which shows that there is a high degree of heterogeneity in this study.After sensitivity analysis, excluding the study of Avgerinos,et al.[7](I2= 38.2%,P= 0.166) (Figure 3B), there was no obvious heterogeneity.After combining with fixed effect quantity (OR = 1.20,95% CI: 1.04–1.39,P= 0.012), the difference was statistically significant.These results suggest that catheter directed thrombolysis can significantly reduce the all-cause bleeding rate.
Gastrointestinal bleeding rateThe heterogeneity test of three studies (I2= 85.4%,P= 0.001) shows that there is a high degree of heterogeneity in this study (Figure 4A).After sensitivity analysis (Figure 10), excluding the study of Arora,et al.[8](I2= 0,P= 0.676) (Figure 4B), there is no heterogeneity.After combining with fixed effect quantity (OR = 1.43, 95% CI: 1.13–1.81,P= 0.003), the difference was statistically significant.These results suggest that catheter directed thrombolysis can significantly reduce the gastrointestinal bleeding rate.
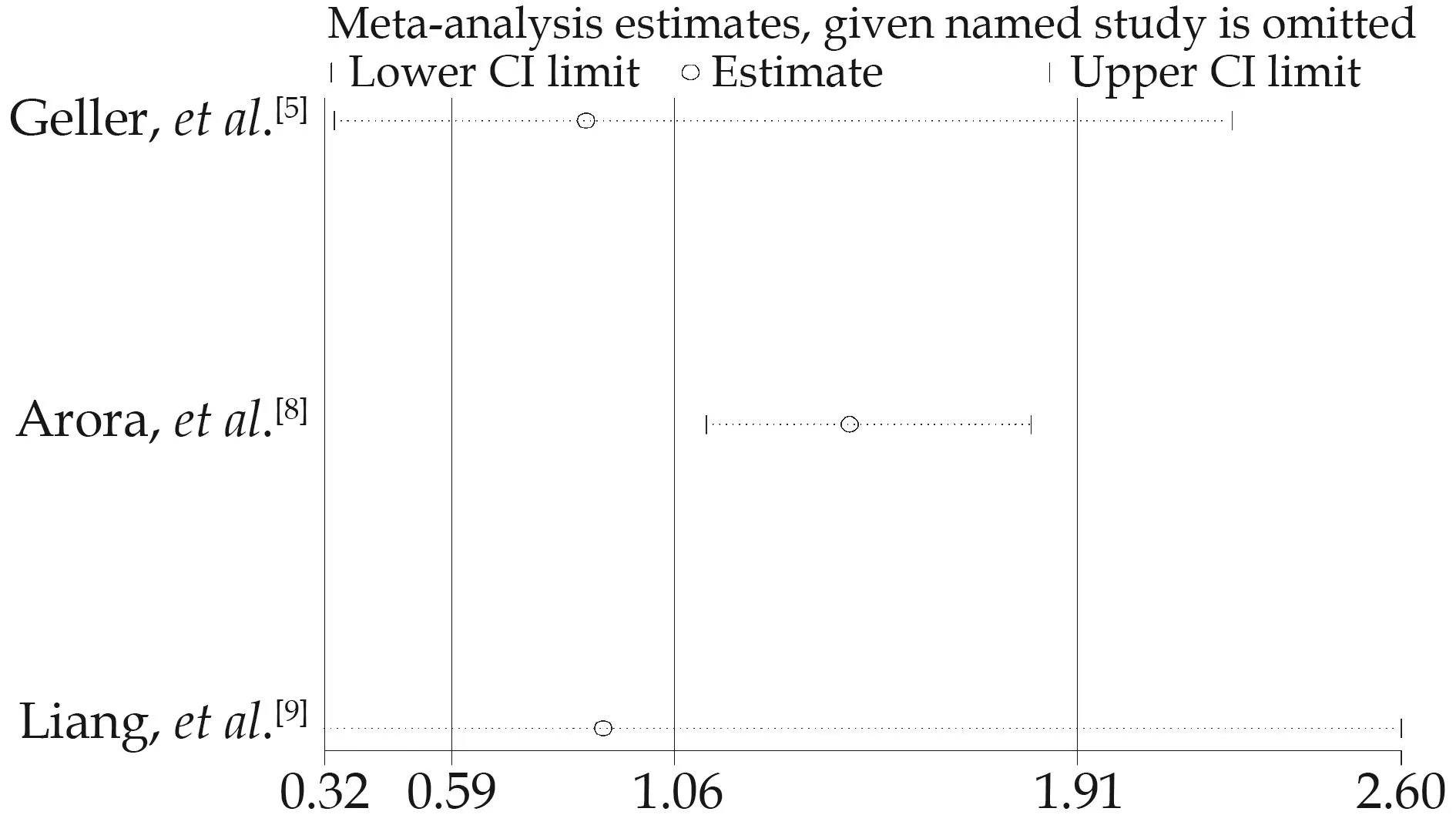
Figure 10 Sensitivity analysis of gastrointestinal bleeding rate comparison between catheter-directed thrombolysis and systemic thrombolysis for pulmonary embolism.
Intracranial hemorrhage rateIn the heterogeneity testof six studies (I2= 19.1%,P= 0.290) (Figure 5), there was no obvious heterogeneity.Through sensitivity analysis (Figure 11), no literature that had a great impact on the results was found.The combined fixed effect (OR = 0.70, 95%CI: 0.47–1.03,P= 0.070), and the difference was not statistically significant.The results showed that catheter directed thrombolysis had no significant effect on the intracranial hemorrhage rate of patients with PE.
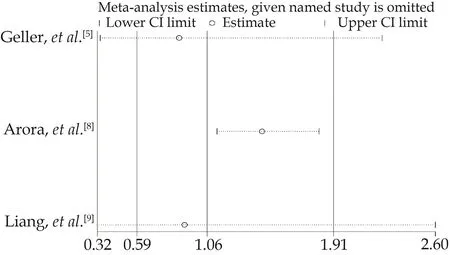
Figure 11 Sensitivity analysis of intracranial hemorrhage rate comparison between catheter-directed thrombolysis and systemic thrombolysis in pulmonary embolism.
Incidence of shockTwo studies were tested for heterogeneity (I2= 0,P= 0.905) (Figure 6), there was no heterogeneity.The combined fixed effect (OR = 0.46, 95% CI:0.38–0.56,P< 0.05), and the difference was statistically significant.It shows that catheter directed thrombolysis can significantly reduce the incidence of shock in PE.
Hospital length of stayThe heterogeneity test of four studies (I2= 97.6%,P< 0.05) (Figure 7A) showed that there was a high degree of heterogeneity in this study.After the study of Sharifi,et al.[6]was excluded from the sensitivity analysis (Figure 12), there was no significant heterogeneity (I2= 31.3%,P= 0.233) (Figure 7B), and the combined fixed effect (SMD = 0.16, 95% CI: 0.07–0.25,P< 0.05).It shows that catheter directed thrombolysis can significantly increase the hospitalization time of patients with PE.
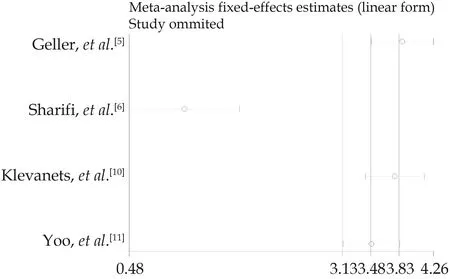
Figure 12 Sensitivity analysis of comparison of hospital stay between catheter-directed thrombolysis and systemic thrombolysis in the treatment of pulmonary embolism.
Sensitivity analysisBased on the sensitivity analysis of in-hospital mortality and intracranial hemorrhage rate,none of the papers had much influence on the results (Figures 8 & 11).The sensitivity analysis on all-cause bleeding rate indicated that the study of Avgerinos,et al.[7]had a great impact on the results and is excluded (Figure 9).In the sensitivity analysis of this study on gastrointestinal bleeding rate is shown that the study of Arora,et al.[8]had a great impact on the results, so it was removed (Figure 10).The sensitivity analysis on the hospital length of stay of this study indicated that the study of Sharifi,etal.[6]has a great impact on the results, which should be excluded (Figure 12).
Publication biasThe results of this study are basicallynon-heterogeneous after sensitivity analysis, and the results are relatively stable, but there are still the following limitations: due to the limitations of language and search strategy, the search may not be comprehensive enough;as the number of literature is less than 10, the bias test cannot be carried out, so no publication bias can be guaranteed; the literature included in this study were all cohort studies, lacking large RCT studies, which may also lead to certain selection bias.
DISCUSSION
ST has been established as the treatment standard for patients with high-risk PE, but the role of CDT in PE is unclear.[7,8]Our study included eight literature reviews with 13,242 participants, including 3962 participants in the CDT group and 9280 participants in the ST group, aimed at comparing the outcomes of CDT and ST in treating PE.Results show that compared to ST, CDT can significantly reduce in-hospital mortality, incidence of shock, and bleeding caused by various factors, especially the gastrointestinal bleeding rate, while also moderately extending the length of hospital stay.
Previous studies have shown that thrombolytic therapy can improve the mortality of patients with intermediate- and high-risk PE,[9]while reducing the incidence of chronic thromboembolic pulmonary hypertension and maintaining exercise tolerance.[10,11]Since then, more and more evidence has proved the advantages of CDT in thrombolysis.In 2014, the United States Food and Drug Adm-inistration approved the EkoSonic intravascular system for ultrasound-assisted CDT to treat PE.[12]Recent studies have shown that CDT can significantly improve in-hospital mortality in patients with PE compared with ST.[13,14]However, there is still a lack of large RCTs demonstrating the efficacy of CDT.The existing literature is mostly limited to relatively small retrospective studies.By combining the current studies, our study also obtained the result that CDT can significantly reduce the in-hospital mortality(OR = 0.41, 95% CI: 0.30–0.56,P< 0.05), which may be attributed to the fact that CDT can directly direct thrombolytic drugs to the pulmonary circulation, thus significantly improving the efficacy of thrombolytic drugs in the resolution of the clot.[15,16]
In the PEITHO (Pulmonary Embolism International THrOmbolysis) study, the patients with intermediate-risk PE who received ST had fewer deaths or hemodynamic decompensation than those who received anticoagulant therapy (2.6%vs.5.6%,P= 0.02).However, ST had more bleeding complications than anticoagulant therapy.Based on the debate on the use of ST in the patients with intermediate-risk PE, ST is primarily used in patients with right cardiac insufficiency who are expected to undergo clinical deterioration and have a low risk of bleeding.[7,17,18]The risk of bleeding complications or hemodynamic instability prevents some PE patients from choosing ST treatment, and the emergence of CDT provides a reliable alternative treatment for patients at high risk of bleeding complications.In one study, CDT was shown to be effective in improving hemodynamics, reducing bleeding complications, and saving PE patients who had failed ST treatment.[19]The ULTIMA (Ultrasound Accelerated Thrombolysis of Pulmonary Embolism) trial compared heparin anticoagulant therapy with CDT to reverse right ventricular dilatation.The results of this randomized trial showed that CDT was superior to heparin alone without increasing the risk of bleeding.[20]In addition, the results of the PERFECT (Pulmonary Embolism Response to Fragmentation, Embolectomy,and Catheter Thrombolysis) trial, which included 101 patients with intermediate- and high-risk PE, also showed that CDT improved hemodynamics and increased clinical success without serious complications.[21]Similarly, our study showed that CDT significantly reduced shock (hemodynamic instability) and all-cause bleeding, including gastrointestinal bleeding.CDT relies on a low doses of thrombolytic drugs and a low systemic circulation flushing rate, which may be the main reason for the low incidence of shock and bleeding complications in CDT.[22,23]
However, our study also revealed some limitations of CDT, including a longer hospital stay compared to ST(SMD = 0.16, 95% CI: 0.07–0.25,P< 0.05).This longer stay may be due to the time-consuming operating room preparation required for CDT, which can increase medical costs for patients.While CDT offers a safe and effective alternative to ST for high-risk patients, the potential increase in hospital stay and associated costs should be considered in treatment decision-making.
The significant reduction in mortality and major complications of patients with PE with CDT compared to ST suggests that CDT may have broader applications in clinical diagnosis and treatment in the future.
CONCLUSIONS
CDT has demonstrated a significant reduction in inhospital mortality, all-cause bleeding rate, gastrointestinal bleeding rate, and incidence of shock compared to ST.However, it may lead to a longer hospital stay.To further evaluate the safety and efficacy of CDT and ST in the treatment of acute PE and other clinical outcomes, larger multicenter, RCT are needed.
ACKNOWLEDGMENTS
This study was supported by the National Natural Science Foundation of China (No.82270258), the National Key R&D Program of China (2020YFC2004800), the Beijing Hospitals Authority Incubating Program (PZ2022004), and the Beijing Municipal Science and Technology Committee (Z221100003522027).All authors had no conflicts of interest to disclose.The authors thank Jin-Wen WANG (Department of Community Health Research, Beijing Anzhen Hospital, Beijing Institute of Heart Lung and Blood Vessel Diseases, Capital Medical University, Beijing, China) for statistical analysis assistance.
 Journal of Geriatric Cardiology2023年6期
Journal of Geriatric Cardiology2023年6期
- Journal of Geriatric Cardiology的其它文章
- Status of cardiovascular disease in China
- Unraveling the mechanisms of a giant coronary sinus
- Iatrogenic pneumopericardium after therapeutic pericardiocentesis for pericardial effusion: a case report
- Target versus sub-target dose of renin–angiotensin system inhibitors on survival in elderly patients with heart failure with reduced ejection fraction: a systematic review and meta-analysis
- Nocturnal hypertension and riser pattern are associated with heart failure rehospitalization in patients with heart failure with preserved ejection fraction
- Down-regulation of the Smad signaling by circZBTB46 via the Smad2-PDLIM5 axis to inhibit type I collagen expression
