Lichen Planus Pigmentosus Inversus: Two Case Reports
Se Hoon Lee, Minah Cho, Yu Jin Han, Yu Ri Woo, Sang Hyun Cho, Jeong Deuk Lee,Hei Sung Kim,2,*
1Department of Dermatology, Incheon St. Mary’s Hospital, The Catholic University of Korea, Seoul, South Korea; 2Department of Biomedicine & Health Sciences, The Catholic University of Korea, Seoul, South Korea.
Abstract
Keywords: lichen planus pigmentosus, lichen planus pigmentosus inversus
Introduction
Lichen planus pigmentosus inversus (LPPI) is a rare variant of lichen planus characterized by gray to brown macules and patches with predominant localization in flexural areas such as the axillae,groin,abdominal folds,and antecubital and popliteal areas.1We herein present two cases of this unusual entity with a brief review of the literature.
Case presentation
Case 1:A 64-year-old woman presented with a 12-month history of slightly pruritic brown lesions on the right breast. Physical examination revealed scaly reticulated brown to gray macules on the lateral side of the right breast(Fig.1A).Dermoscopic examination revealed brown-gray globules and dots (Fig. 1B). Histopatho-logically, the specimen showed orthokeratosis, epidermal atrophy,vacuolar changes in the basal layer, mild perivascular lymphocytic infiltration in the upper dermis,and pigmentary incontinence (Fig. 1C). The patient was prescribed 0.1%methylprednisolone aceponate and 0.1%tacrolimus ointment, which she alternately applied once a day for 1 month.There was some improvement in her pruritus,but the lesions remained stationary at the 2-month follow-up.Case 2: A 49-year-old woman presented with a 2-year history of asymptomatic brownish macules on her intertriginous areas. Physical examination revealed numerous gray to brownish macules and patches on the bilateral axillae, inframammary folds, and inguinal folds. Dermoscopic examination revealed diffuse reticulated brown pigmentations. Histopathologically, orthokeratosis with atrophy of the epidermis, vacuolar changes in the basal layer, and dense perivascular lymphocytic infiltration were observed in the upper dermis with pigmentary incontinence.The patient was prescribed oral tranexamic acid (1g/day) with 0.12% retinal cream, which were applied once daily for 1month.At the time of this writing,the patient was undergoing follow-up.

Figure 1. Clinical and histopathological features of the patient with lichen planus pigmentosus inversus.(A)A 64-year-old woman with slightly pruritic scaly reticulated gray to brownish patches. (B) Dermoscopic image showed brown-gray globules and dots. (C) Microscopic examination revealed hyperkeratosis,hypergranulosis,and hydropic degeneration of the epidermis as well as mild lymphocyte infiltration with pigmentary incontinence in the papillary dermis (hematoxylin and eosin, ×400).
The patients have given their consents for their images and other clinical information to be reported in the journal.
Discussion
So far, Lichen planus pigmentosus inversus has been reported in 72 cases from 35 reports in PubMed(https://pubmed.ncbi.nlm.nih.gov/),Google Scholar(https://schol ar.google.com/), and Korea Journal of Dermatology(https://kjd.derma.or.kr/)databases using the search term“l(fā)ichen planus pigmentosus inversus”. The onset age ranged from 5 to 84 years,and the average was 53.3.Of all,only 4 cases were under the age of 18. There is a predominance in female (2.08:1). The disease duration ranged from 2weeks to 15 years,and the average was 14.67 months. Symptom, pruritus, was present in 52.7% of patients.Clinically,Lichen planus pigmentosus inversus is characterized by grey to dark brown hyperpigmented macules and patches predominantly located in the intertriginous and flexural areas. The axillae and groin are the most commonly affected areas, followed by the inframammary folds in women and the neck and face in men.Lesions were bilateral in 79.7%of patients.(Table 1).
Reported biopsy findings have been all similar,showing hyperkeratosis with basal vacuolization of epidermis,lichenoid infiltration of lymphocytes and histiocytes,and pigmentary incontinence.The pathological features are in accordance with those in lichen planus pigmentosus.
The cause of lichen planus pigmentosus inversus in unclear. External mechanical stimuli, such as friction(koebners phenomenon), tight underclothes,1-3exposure to metallic dust and fume,4and previous radiotherapy5have been suggested as causes.
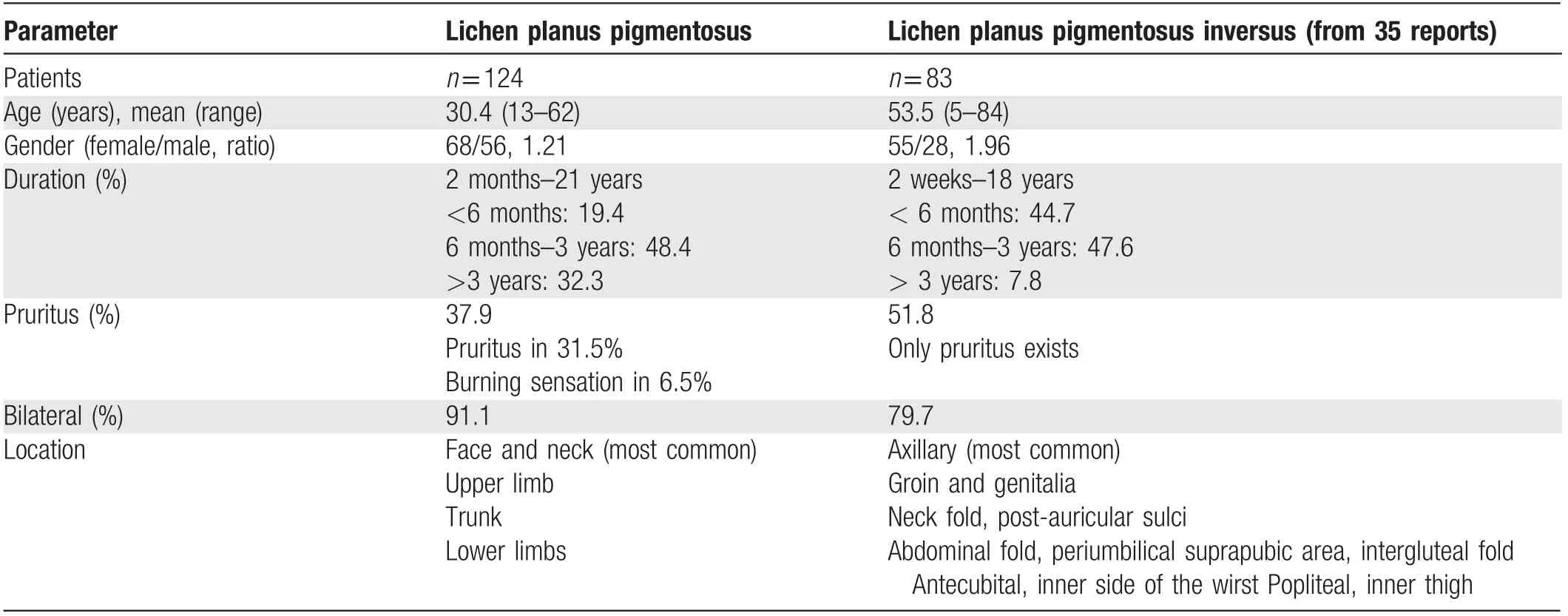
Table 1 Clinical and demographic features of lichen planus pigmentosus and lichen planus pigmentosus inversus.
The differential diagnosis of lichen planus pigmentosus inversus includes candidial intertrigo, acanthosis nigricans, postinflammatory hyperpigmentation, pigmented contact dermatitis, fixed drug eruption and other lichenoid dermatosis.6
Therapeutic management is often challenging.The most commonly used treatments are topical calcineurin inhibitors and medium to high potency topical corticosteroids,but only few cases have shown improvement. In adolescent patients,there was a case where narrow-band ultraviolet treatment was effective.7In a few cases spontaneous healing was reported.1
- 國際皮膚性病學(xué)雜志的其它文章
- Radiofrequency in Facial Rejuvenation
- Liponeurofibroma
- Successful Treatment of Severe Pityriasis Rubra Pilaris with Cyclosporine A in An Infant
- Toe Absence Related to Verrucous Carcinoma
- Dermatoscopy in the Diagnosis of Vulvar Basal Cell Carcinoma: A Case Report
- Skin Organoid Research Progress and Potential Applications

