Repeatability and comparison of Corvis ST parameters before and after accelerated transepithelial corneal cross-linking in keratoconus eyes
Kai-Li Yang, Yu-Wei Gu, Qi Fan, Li-Yan Xu, Chen-Jiu Pang, Sheng-Wei Ren
Abstract
?KEYWORDS:keratoconus; accelerated transepithelial corneal cross-linking; Corvis ST parameters; repeatability; early corneal biomechanical changes
INTRODUCTION
Keratoconus is a progressive corneal disorder characterized by progressive corneal thinning and increasing conical shape[1]. Previous study reported the disease typically presents in teenage years, and leads to irregular astigmatism and visual impairment[2]. The current options for improving visual acuity mainly included glasses, rigid gas permeable contact lenses (RGP), intracorneal ring segments (ICRS), corneal cross-linking (CXL) and corneal transplantation[3]. As a method halting the progression of keratoconus, CXL method was shown to be an effective procedure for progressive keratoconus by increasing the corneal stiffness[4].
The CXL is a photochemical reaction utilizing ultraviolet (UV), a light and riboflavin as a photosensitizer[5], and induces covalent cross-link bonds between collagen fibers in the corneal stroma[6]. The CXL could halt the progression of keratoconusviaincreasing the corneal biomechanical strength and stability[7]. The accelerated transepithelial CXL (ATE-CXL), in which the epithelium is not removed, was developed to maintain the integrity of the corneal epithelium layer and decrease the risk of postoperative infection[8-9]. Several studies have reported the ATE-CXL was safe and effective in terms of the topographic outcomes of keratoconus[10-11]. Previous study suggested that the dynamic corneal response (DCR) parameters following CXL might be changed before corneal shape modifications[2], but the study related to the efficacy of corneal biomechanical parameters was limited. The Corneal Visualization Scheimpflug Technology (Corvis ST) is a relatively new noncontact tonometer, which is available to measure the corneal biomechanical properties[12-13]. Recent study reported the Corvis ST could detect changes in corneal biomechanical properties after CXL, and these researches mostly assessed the corneal biomechanical changes after conventional CXL or epithelium off CXL in eyes with keratoconus[14-15]. The study reporting the changes of Corvis ST parameters after ATE-CXL remains limited. In addition, previous studies reported that the repeatability of corneal biomechanical parameters were acceptable in normal and keratoconus eyes[16-17]. However, the study evaluating the repeatability of these parameters after ATE-CXL was still limited. Thus, the current study aimed to evaluate the repeatability of Corvis ST parameters preoperative and 1mo postoperative, and further compared the corneal biomechanical changes after ATE-CXL in patients with keratoconus.
SUBJECTS AND METHODS
EthicalApprovalThis study adhered to the Declaration of Helsinki guidelines and all procedures involving human subjects were approved by the Institutional Review Board of Henan Eye Hospital [ethical approval number: HNEECKY-2019(5)]. This study has been registered at Chinese Clinical Trial Register (Registration number: ChiCTR-1900023046), and written informed consent was obtained from all patients or the legal guardian of pediatric keratoconus.
Patients with keratoconus underwent the treatment of ATE-CXL at Henan Eye Hospital & Henan Eye Institute between March 2019 and August 2019. Progressive keratoconus eyes that have increments of a maximal keratometry or an astigmatic degree for at least 1.00 D in the last year were included in the research[10]. Subjects with anterior stromal scar, thinnest corneal thickness (TCT) less than 400 μm, previous other ocular diseases and a history of ocular surgeries were excluded. Finally, thirty eyes of 30 keratoconus patients aged 21.7±4.3 years were recruited in the current prospective study.
ExaminationsThe basic characters of participants were collected through medical records. The ocular examinations, which included best corrected visual acuity (BCVA), slit lamp examination, and ophthalmoscope examination, were performed by one experienced operator between 9:00 and 17:00. The mean endothelium cell density (MCD) was measured by a noncontact specular microscope (Tomey, EM-3000, Tokyo, Japan). The corneal tomographic measurements were performed by swept-source anterior segment optical coherence tomography machine (Casia SS-1000, Tomey, Nagoya, Japan), and the steep keratometry (Ks), flat keratometry (Kf), and mean keratometry (Kmean) and apex corneal thickness (ACT) and TCT were recorded.
Corvis ST (Oculus 72100, Wetzlar, Germany) takes Scheimpflug images of the anterior segment at a rate of 4330 frames and collects approximately 140 horizontal section images[18-19]. It captures the corneal curvature changes in space and time with an air pulse. The corneal biomechanical response contains three phases: first applanation, highest concavity and second applanation[20]. The values of applanation times, velocities, deformation amplitude (DA), deflection length (DLL), deflection area (DLAr) and delta arc length (dArcL) at three phases were recorded. In addition, the intraocular pressure (IOP), biomechanical corrected intraocular pressure (bIOP), central corneal thickness (CCT),peak distance (PD), radius and whole eye movement were presented. The new Corvis ST parameters were also added in current study: the maximum value of the ratio between deformation amplitude at the apex 1 mm and 2 mm from central cornea [DA Ratio Max (1 mm), DA Ratio Max (2 mm)], max inverse radius, integrated radius, Ambrósio’s relational thickness horizontal (ARTh), stiffness parameter at the first applanation (SP A1) and Corvis biomechanical index (CBI). The detailed descriptions of parameters were shown in Table 1. Three repeated measurements of preoperative and 1mo postoperative were examined by the same Corvis ST Software and only examinations with good quality scores that enabled calculation of all deformation parameters were included in the analysis. All Corvis ST measurements were performed by a single experienced operator (QF) with 2-5min interval[12].
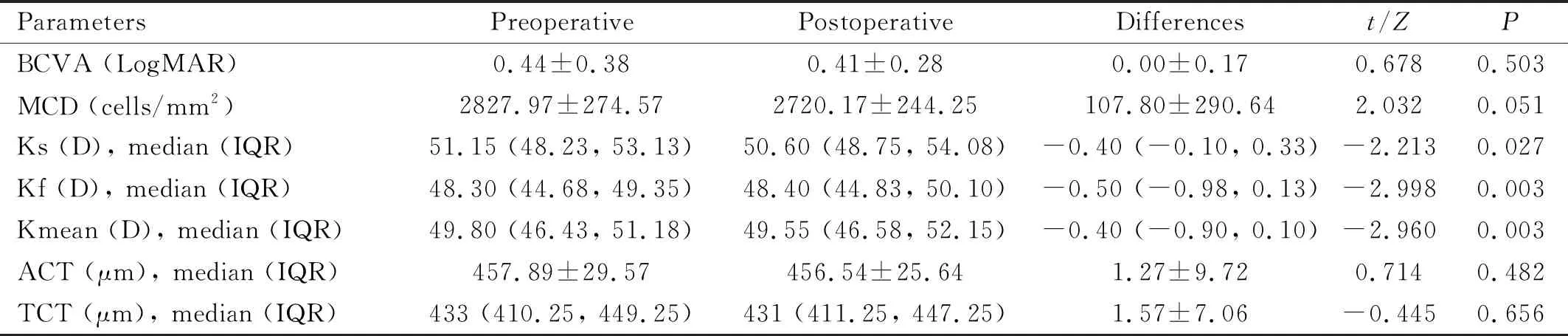
Table 1 The clinical parameters of keratoconus eyes (n=30)
SurgicalTechniqueATE-CXL surgery was performed by one professional ophthalmologist. Before the surgery, topical anesthetic eye drops were applied. After a lid speculum was used, paracel solution (0.25% riboflavin-5-phosphate, hydroxylpropyl methylcellulose, NaCl, ethylenediamine tetraacetic acid, Tris, and benzalkonium chloride) was used every 60s in 4min. The cornea was then continually infiltrated with Vibex-Xtra Solution (riboflavin phosphate 2.80 mg/mL and NaCl) every 60s in 6min. After the cornea was rinsed with balanced salt solution (BBS), UV treatment (irradiation intensity: 45 mW/cm2; pulse irradiation mode: one second on, next second off; total irradiation energy: 7.2J) using Avedro’s KXL System for 320s with BBS used to keep the ocular surface moist. Then, a bandage contact lens was applied after the procedure. The postoperative medications containing levofloxacin (4 times daily for 2wk), 0.1% fluorometholone (4 times per day for 1mo), and artificial tears (4 times daily for 3mo) were used after the surgery completed.
StatisticalAnalysisThe normality of continuous data was tested by Kolmogorov-Smirnov test. The mean ± standard deviation (SD) was applied to described normally distributed data, and median (IQR, interquartile range) for not. The repeatability is defined as the SD observed upon multiple measurements of the same eye. It is considered as a method to evaluate the reliability and precision of Corvis ST measurements[21]. The interclass correlation coefficient (ICC) and 95% confidence interval (CI), Cronbach’ α, repeatability coefficient (RC), and coefficient of variation (CV) were used to evaluate the repeatability of Corvis ST parameters. The ICC ≥ 0.75 means good to excellent repeatability, and ICC ≥ 0.60 means moderate, and ICC <0.60 means poor repeatability[22]. The RC was calculated as 2.77 × within-subject SD (Sw)[23]. The pairedt-test or Wilcoxon rank test was used to evaluate the differences between preoperative and postoperative data. All statistical analysis was performed using SPSS 23.0 software package, andP<0.05 (two-tailed) was considered as statistically significant.
RESULTS
TheClinicalParametersinEyeswithKeratoconusNo postoperative complications were found at 1mo follow up of ATE-CXL. The clinical parameters of keratoconus patients were shown in Table 1. There were no significant differences in BCVA, MCD, ACT and TCT before and after ATE-CXL over the 1mo postoperatively (P>0.05). The values of Ks, Kf and Kmean changed from 51.15 (48.23, 53.13), 48.30 (44.68, 49.35) and 49.80 (46.43, 51.18) preoperatively to 50.60 (48.75, 54.08), 48.40 (44.83, 50.10), and 49.55 (46.58, 52.15) postoperatively, respectively (allP<0.05).
RepeatabilityoftheCorvisSTParametersinEyeswithKeratoconusThe CV, Cronbach’ α, ICC (95%CI),Swand RC values of each parameter were shown in Table 2 (preoperative) and Table 3 (1mo postoperative). At preoperative, 26 (66.67%) of 39 parameters showed good to excellent repeatability (ICC ≥0.75), 6 (15.38%) showed moderate (ICC ≥0.60), and 7 (17.95%) showed poor repeatability (ICC <0.60). Similarly, 34 (87.18%) showed good to excellent repeatability, 3 (7.69%) showed moderate, and 2 (5.13%) showed poor repeatability at 1mo ATE-CXL follow up. The RC values of integrated radius and SP A1 were 3.76 and 22.85 at preoperative, and decreased to 2.35 and 16.53 at 1mo ATE-CXL follow up, separately.
ComparisonofCorvisSTMeasurementsBetweenPreoperativeand1moPostoperativeThe IOP and bIOP measured by Corvis ST Software increased from 12.87±2.14, 14.61±1.93 preoperatively to 14.08±2.35, 15.99±2.22 postoperatively (Table 4,P<0.05). The A1T, Radius,A1DA, HCDLL and SP A1 increased, while A2T, DA Ratio Max (2 mm) and integrated radius decreased after ATE-CXL (P<0.05).
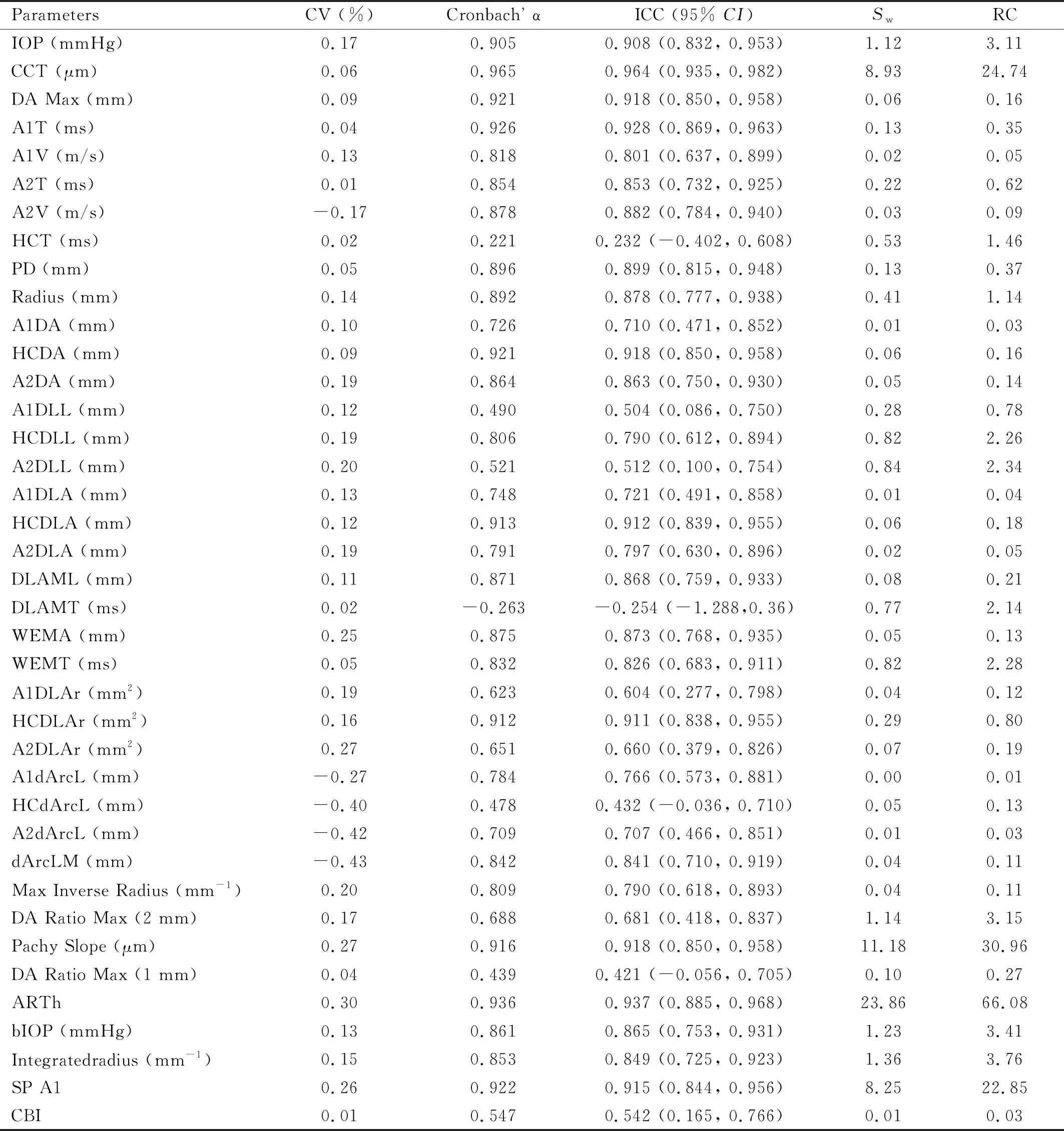
Table 2 Repeatability of Corvis ST parameters at preoperative (n=30)
DISCUSSION
The early changes of DCR parameters following ATE-CXL occurred before shape modifications, and could be detected by Corvis ST Software. The current study demonstrated that the repeatability of Corvis ST parameters before and after ATE-CXL 1mo were both acceptable. The parameters of IOP, bIOP, A1T, Radius, A1DA, HCDLL, SP A1 increased,while Ks, Kf, Kmean, A2T, DA Ratio Max (2 mm), and integrated radius decreased at 1mo ATE-CXL.
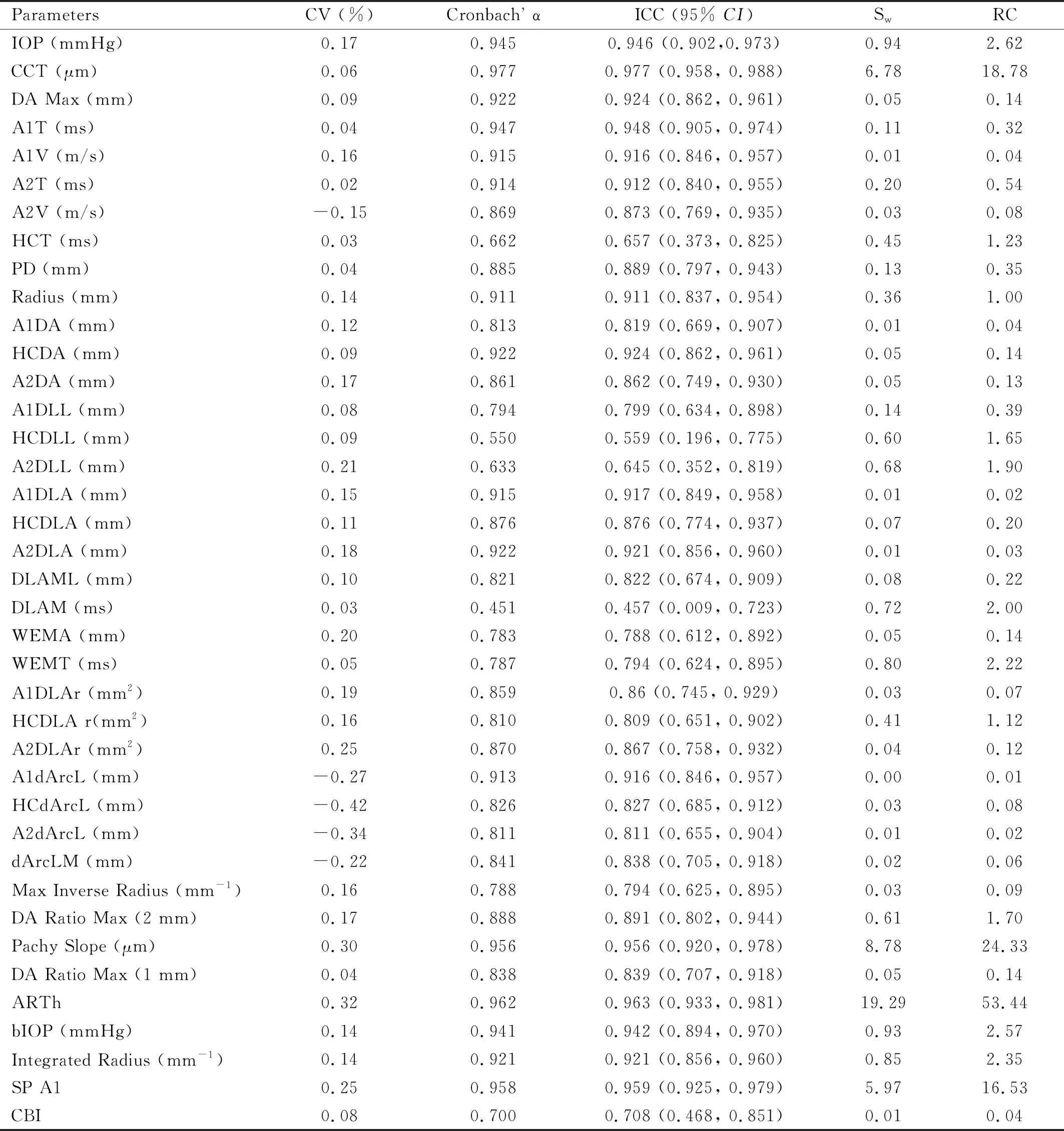
Table 3 Repeatability of Corvis ST parameters at 1mo postoperatively (n=30)
The Corvis ST reports a variety of biomechanical parameters correlated with the applanation events[24-25]. Recent studies have assessed the repeatability of Corvis ST parameters, and the results showed that Corvis ST parameters were reliable in normal eyes and keratoconus eyes[17,26]. Compared to Yeetal[26]study that reported the ICC values of IOP, CCT, A1DLL, A2DLL, A1V, A2V, PD and Radius were 0.78, 0.98, 0.30, 0.32, 0.81, 0.50, 0.56 and 0.20, separately, the current study had higher ICC values of above parameters in keratoconus eyes. The current study found 26 parameters showed good to excellent repeatability, which was similarly to previous finding that 28 parameters showed good to excellent repeatability[17]. The discrepancy of ICC values in different studies might be attributed to the sample size, and a multi-center study should be conducted in future. After ATE-CXL, the ICC values of PD, HCDLL, HCDLA, DLAML, WEMA, WEMT, HCDLAr and dArcLM after ATE-CXL were lower than that preoperatively, while other parameters were higher. In addition, we found the repeatability of Corvis ST parameters after ATE-CXL have a larger percentage of good than that at preoperative, which indicated the measurements of Corvis ST after ATE-CXL were also reliable.
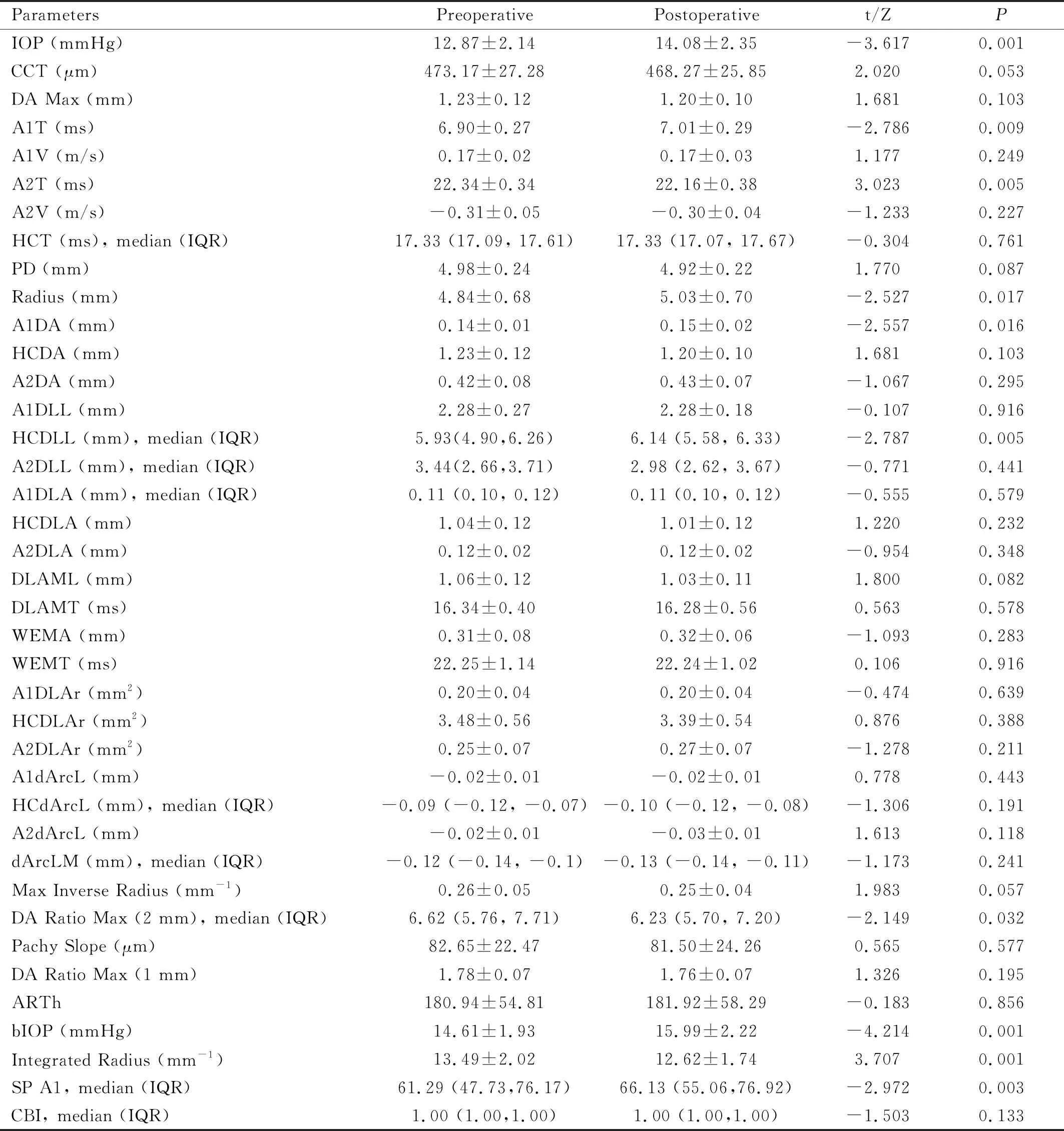
Table 4 Comparison of Corvis ST measurements between preoperative and 1mo postoperative
Our study indicated the Ks, Kf and Kmean values were decreased after ATE-CXL in 30 keratoconus eyes, which was partly consistent with other studies. Tianetal[10]reported that ATE-CXL was a safe and effective treatment in children with progressive keratoconus. Aixinjueluoetal[27]found the keratometry was decreased in 12mo follow-up, and no complications of ATE-CXL in 30 keratoconus eyes were investigated. Huangetal[28]demonstrated that the 2y topographic outcomes of ATE-CXL remained unchanged and the densitometry values of the full corneal thickness may decrease to normal levels at 2y after ATE-CXL. Besides the changes of keratometry, several studies have reported the changes of BCVA and corneal thickness, which were not statistically different from our study. A study included 26 keratoconus eyes indicated the BCVA and Kmax were improved at 12mo after ATE-CXL[29]. Huangetal[28]reported that the corneal thickness values decreased slightly at 12mo but increased at 24mo postoperatively when comparing to preoperative status. The BCVA of 18 keratoconus eyes improved from 0.64 preoperatively to 0.69 at 1y after ATE-CXL, while the BCVA increment and the corneal thickness decrement were not statistically at 1mo follow up[10]. Kohetal[30]reported that both the uncorrected and corrected distance visual acuity enhanced in moderate keratoconus through 1y of CXL follow up. The inconsistent results of topographic parameters and BCVA might be related to the discrepancy of sample size and follow up time among different studies. Thus, the long term efficacy of ATE-CXL would be continued to study in future.
The current study found the parameters of IOP, bIOP, A1T, Radius, A1DA, HCDLL and SP A1 increased, while A2T, DA Ratio Max(2 mm), and integrated radius decreased after 1mo ATE-CXL. The changes of IOP, bIOP, SP A1, Radius and Integrated radius after ATE-CXL were consistent with that after CXL or epithelium off CXL procedure. Several studies evaluated the changes of Corvis ST parameters at different follow-up visits after CXL[12,31]. Bak-Nielsenetal[32]recruited 27 keratoconus eyes and found HCT, A2T and DA parameters were significantly changed at 97d after CXL. Steinbergetal[33]demonstrated the IOP increased 3 mmHg, CCT decreased 35 μm, A1T increased 0.12 ms, and A2T decreased 0.37 ms at 3mo after CXL. However, the changes of these parameters did not show statistically differences at 6mo follow-up visit after CXL. Also, they further found the PD decreased 0.5 mm while Radius increased 0.5 mm in 24 keratoconus eyes[34]. Tomitaetal[35]included 48 eyes with keratoconus and found PD was significantly increased while no significant changes of DA and Radius were found at 1y after CXL. Vinciguerraetal[14]conducted a prospective study of 34 eyes and found the corneal stiffness was improved following CXL 1mo regarding to the SP A1 increased, inverse concave integrated radius and DA ratio decreased. In their other study which included 66 eyes, the increment of corneal stiffness was verified again at the same follow up[31]. The increments of IOP and bIOP could due to the corneal stiffness increment, which was verified in other study[36]. The SP A1 value reflects the corneal resistance to deformity and a high value stands for a stiffer biomechanically cornea[15,37-38]. Integrated radius is a stiffness parameter that calculated by the integrated area under the curve of the inverse radius of curvature at the highest concavity, and the change after CXL might be related to the Kmean in a 5 mm zone of the steepest point[15]. The low value of the integrated radius and high value of radius are associated with a stiffer cornea[37]. The A1DA stands for deformation amplitude at the first applanation, and HCDLL means deflection length at the maximum deformation. The changes of A1DA and HCDLL after CXL were limited, and further study should be conducted to certify the changes in later.
Our study found the corneal stiffness was improved at1mo post-ATE-CXL, and the results provide some references in evaluating the effect of CXL on biomechanical parameters. However, there were several limitations. Firstly, the current study recruited 30 keratoconus patients, which is relatively small, and might decrease the statistical power. Further multi-center and large sample study will be conducted in a later study. Secondly, our study mainly evaluated the corneal biomechanical changes within a relatively short postoperative period of 1mo. The long term efficacy of the ATE-CXL would continue to be observed in later research.
In conclusion, the study indicated that the repeatability of the Corvis ST parameters before and after ATE-CXL was both acceptable. In addition, the corneal stiffness was improved 1mo after ATE-CXL. However, multi-center study and long term effects of ATE-CXL needs to be conducted in future.

