Aspergillus infection of pacemaker in an immunocompetent host: a case report
Yuan GAO, Rong-Fang LAN, Ning ZHANG, Shao-Xian WANG, Zhong-Lin HAN, Wei XU
Nanjing Drum Tower Hospital, Clinical College of Nanjing Medical University, Nanjing, China
Keywords: Aspergillus flavus; Device explantation; Pacemaker infection
The incidence of CIED (Cardiac Implantable Electronic Devices) infections is 0.13%-8.0%.[1,2]Fungal organisms account for up to 10% and Aspergillus infections are extremely rare. Here, we present a case of CIED-related Aspergillus infection in an immunocompetent patient.
A 53-year-old man with past medical history notable for poorly controlled type 2 diabetes mellitus, persistent left superior vena cava, status post permanent pace maker placement for sick sinus syndrome came to our hospital for routine evaluation of his device. Interrogation of his device revealed a recent increase in his atrial pacing threshold (3.5 v/0.4 ms) and several episodes of non-capture. During the initial attempt to replace his generator, he was found to have a large amount of cheese-like necrotic material in his generator pocket.
On physical examination, he was afebrile. There is no swelling or tenderness around the pocket area. Cardiac examination revealed no abnormal murmurs. The ventricular pacing threshold was normal and pacemaker was programmed to VVI mode. The patient denied intravenous drug use, blood transfusion, malignancy or any use of immunosuppressive agents. The laboratory data were remarkable for Serum Beta-D-glucan Assay of 385.5 pg/mL, CRP of 23.9 mg/L, hemoglobin of 124 g/L (Normal range 130-175 g/L). HIV test was negative. His chest X-ray and transthoracic echocardiogram failed to show any abnormalities. Transesophageal echocardiography revealed a 30 × 28 mm vegetation adherent to one of the pacing leads (Figure 1A). Contrast-enhanced CT of the chest revealed large filling defect from the level of aortic arch to right atrium. We assumed the filling defect is due to the necrotic substance(Figure 1B).
The pacemaker was extracted percutaneously and we used an innovative temporary cardiac pacing strategy to fix the lead to right ventricle through the right jugular vein. We observed the leads engulfed by massive cheese-like substances (Figure 1C). Swabs of the electrodes and generator were sent for culture and each sample yieldedAspergillus flavuson blood agar (Figure 1D & E). Treatment was transitioned to intravenous voriconazole 200 mg b.i.d. for the following six weeks. We were going to surgical implant another device but decided to do a less invasive procedure due to the patients concerns. Finally, we implanted a permanent pacemaker percutaneously. After one-year follow-up, the patient presented no systemic signs of infection relapse.
With the increasing use of intracardiac devices, clinicians are prone to encounter more patients with CIED-related complications. Infection related to devices causes significant mortality. Aspergillus species account for 20% to 30%of fungal endocarditis and are less common than Candida species as causative pathogens.[3]CIED-related Aspergillus infection should be suspected in persons with underlying hematological malignancies, recent cardiothoracic surgery,intravenous drug use, and immunosuppression with culture-negative endocarditis and/or systemic or pulmonary emboli.[4]Our patient is immunocompetent without any other known risk factors except uncontrolled diabetes. He may have had some occupational exposure to Aspergillus due to work as a sanitary worker.
The initial symptoms of CIED-related Aspergillus infection may be minimal and insidious making the diagnosis difficult. Diagnosis ultimately requires confirmation of histology and culture.[5]Here we demonstrate the importance of transesophageal echocardiography (TEE) to such patients suspected of CIED-related infections. A study conducted in 2003 reveals TEE has superior sensitivity (> 90%) over TTE (< 30.5%) and shows significant advantages on visualizing vegetations.[6]Noninvasive marker, such as galactomannan, may be positive but are not specific for the site of disease. False-positive results can occur with fungal infections (i.e., histoplasmosis, blastomycosis, cryptococcosis,and penicilliosis), as well as concomitant antibiotic therapy with piperacillin-tazobactam and amoxicillin-clavulanate.[4]
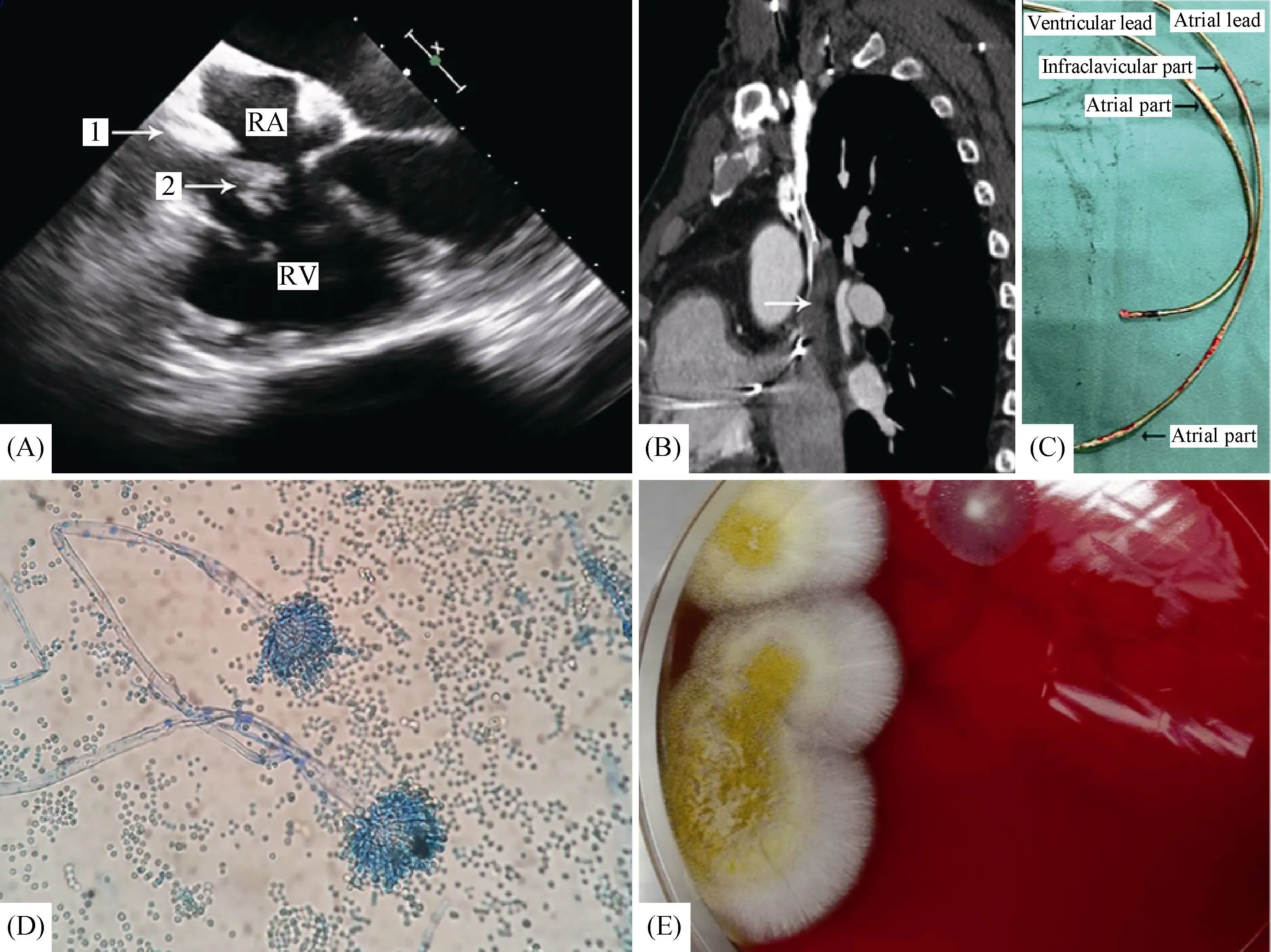
Figure 1. Clinical data of the case. (A): Transesophageal echocardiographic images. Vegetation adherent to the pacemaker leads prolapsing into the atrial aspect of tricuspid valve (1. Head of vegetation. 2. Pedicle of vegetation). (B): Computed tomography of chest. Sagittal aspect, arrow shows filling defect from aortic arch to right atrium. The filling defect is assumed to be the necrotic substance. (C): Cheese-like necrotic substances engulfing the lead. (D): Photomicrograph from vegetations presents classic structure of Aspergillus flavus. Phialides are biseriate and arise circumferentially. Conidia are round, slightly rough and form long chains. (E): Positive culture of Aspergillus flavus on blood agar. Colonies are yellow, granular and velvety. RA: right atrium; RV: right ventricle.
Infections related to intracardiac devices should be treated with removal of the infected hardware and appropriate antimicrobial therapy.[7,8]Voriconazole or liposomal AmB(3-5 mg/kg per day) are recommended as first-line agents.However, the duration of antifungal therapy is still controversial. Guidelines recommend long duration of anti-fungal therapy (> 2 years) with consideration of lifelong therapy concomitant with frequent clinical and echocardiographic assessment for possible recurrence.[8]In our patient, we used vancomycin and cefuroxime empirically before the final diagnosis. The patient responded well with his C-reactive protein (CRP) dropping from 23.9 to 4.6 mg/L. Treatment was transitioned to intravenous voriconazole 200 mg b.i.d.for the following six weeks after the positive culture ofAspergillus flavus. For the next one year follow up, there is no recurrence of infection and both TEE and chest CT showed a marked decrease in size of the vegetation. We conducted a MEDLINE search for CIED-related aspergillus infection,the duration of antibiotics varies, ranging from three weeks to lifelong time. Whether CIED-relatedAspergillusinfection patients without immunocompromising status need the lifelong antifungal medications still need to be proved.
Finally, we want to share our single case experience on the choice of re-implantation strategy. Considering the patient had left persistent superior vena cava and refused the insertion of an epicardial pacemaker, we decided to implant a permanent pacemaker percutaneously through the infectious side. His pacemaker worked well during the one-year follow-up. Although it is recommended the re-implantation should be on the contralateral side of the infection, we present our single case experience of reimplanting on the side of the infection.
In conclusion, the CIED infections due to fungal organisms are rare but fetal. The initial symptoms may be minimal and insidious. When CIED infections are suspected,TEE should be performed. The guidelines recommend combing surgical and medical treatments but more specific management consensus is still required, these should address the choice of antifungal agents and their duration, the timing of surgery, and follow-up.
Statement of Ethics
In this case report, all the treatment comply with the guidelines for human studies and research was conducted ethically in accordance with the World Medical Association Declaration of Helsinki. In the manuscript, we had the written informed consent to publish their case (including publication of images) from our patient. Also, the study protocol was approved by the institute’s committee on human research. Information revealing the subject’s identity is to be avoided. All patients should be identified by numbers or aliases and not by their real names.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work was supported by National Natural Science Foundation of China (No. 81600267) to HAN ZL. The funder had no role in study design, data collection and analysis,decision to publish, or preparation of the manuscript.
 Journal of Geriatric Cardiology2020年1期
Journal of Geriatric Cardiology2020年1期
- Journal of Geriatric Cardiology的其它文章
- Polymorphic ventricular tachycardia during phase II cardiac rehabilitation in a patient with heart failure: a case report
- “One-man” bailout technique for high-speed rotational atherectomy—assisted percutaneous coronary intervention in an octogenarian
- Is dual therapy the correct strategy in frail elderly patients with atrial fibrillation and acute coronary syndrome?
- A meta-analysis of 1-year outcomes of transcatheter versus surgical aortic valve replacement in low-risk patients with severe aortic stenosis
- Anemia in patients with high-risk acute coronary syndromes admitted to Intensive Cardiac Care Units
- Prognostic factors in heart failure patients with cardiac cachexia
