A Single-center Retrospective Cohort Study on Cesarean Section under General Anesthesia
Xu Li,Biye Wu,Mingzhu Zhang3,Le Shen
1Department of Anesthesiology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
2Department of Anesthesiology,Fudan University Shanghai Cancer Center,Shanghai 200032,China
3Department of Anesthesiology,Cancer Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100021,China
Key words:general anesthesia;cesarean section;pathogenies;maternal and neonate outcome
Objective Neuraxial block is the most common anesthesia method for cesarean section (CS).However,for some urgent and high-risk cesarean delivery,general anesthesia (GA) also plays a very important role.We aimed to find out the reasons of choosing GA for CS in our center and the factors that may be related to the maternal and fetal outcomes.Methods We retrospectively selected parturients who had CS procedures under GA in Peking Union Medical College Hospital from January 1,2014 to December 31,2016.Clinical data (baseline maternal status,preoperative status,perioperative information,maternal and fetal outcomes) of parturients and neonates were collected and analyzed.We summarized the common reasons for applying general anesthesia,and compared the back-to-ICU ratio and hospital stay time between parturients with different maternal American Society of Anesthesiologists (ASA) grade,gestational weeks and intraoperative blood loss,as well as the fetal one-minute Apgar score between different maternal ASA grade and gestational weeks.Results There were 98 cases of CS under GA enrolled in the study.Among the maternal and fetal factors,pregnancy with internal or surgical diseases is the most common reason (59 cases,60.2%) for choosing GA,followed by the placenta and fetal membrane abnormalities (38 cases,38.8%) and the pregnancy-specific disorders(36 cases,36.7%).ASA grade Ⅲ-Ⅳ of parturients (χ2=44.3,P<0.05),gestation period < 37 weeks (χ2=23.4,P<0.05),and blood loss > 800 ml (χ2=5.5,P<0.05) were related to the higher postoperative intensive care unit (ICU) rate in parturients.ASA grade Ⅲ-Ⅳ of parturients (t=-2.99,P<0.05),gestation period < 37 weeks(t=2.47,P<0.05) were related to the longer hospital stay.ASA grade Ⅲ-Ⅳ of parturients (t=2.21,P=0.01) and gestation period < 37 weeks (t=-3.21,P=0.002) were related to the lower one-minute Apgar score of neonates.Conclusion Pregnancy with internal or surgical diseases is the most common reason for choosing GA for CS.High ASA grade and short gestation period were the related factors of high postoperative ICU ratio for parturients and low one-minute Apgar score for neonates.
NEURAXIAL block is the common choice for cesarean section (CS) procedure.It could provide effective pain control,mobility control and fast recovery to daily activities,which is important for new mothers' life quality.1The latest obstetric anesthesia guidelines still recommend spinal anesthesia as the preferred anesthesia for most cesarean section.2
However,in some circumstances (e.g.,profound fetal bradycardia,ruptured uterus,severe hemorrhage,severe placental abruption,umbilical cord prolapse,and preterm footling breech),general anesthesia (GA)may be the most appropriate choice because it can provide better circulation and airway control.GA even is routinely chosen for CS in some hospitals.2
In the Peking Union Medical College Hospital(PUMC),the routine anesthesia method for CS is neuraxial block,mainly using combined subarachnoid and epidural anesthesia (CSEA).GA is considered when parturients have contraindications for neuraxial block,in emergency,or under certain urgent circumstances such as concurrent severe heart diseases.In this retrospective study,we focused on the reasons for choosing GA for CS,and tried to recognize factors that relate to poor outcome of parturients and neonates after CS under GA.
PATIENTS AND METHODS
Patient selection and data collection
This retrospective cohort study was approved by the Ethics Committee of PUMC Hospital (S-K882).Written informed consent was waived.The inclusion criteria are maternity patients receiving CS under GA in our hospital from January 1,2014 to December 31,2016.Those with gestation period less than 28 weeks were excluded from the study.We retrospectively collected data including the following aspects:1) the baseline maternal information:age,height,weight,body mass index (BMI),and gestation period;2) preoperative status:maternal diseases(i.e.,preexisting cardiac,hypertension,respiratory,renal,hematologic,neurologic,and neoplastic disorders),pregnancy-related complications,American Society of Anesthesiologists' Physical Status classification (ASA grade);3) perioperative information:the indications for GA,urgency of case,fasting time,mode of airway management,anesthetic medications used for induction and maintenance;4) maternal outcomes:whether or not admitted to the Intensive Care Unit (ICU),time stayed in ICU;5) fetal outcomes:neonatal Apgar scores,whether or not admitted to the neonatal ICU(NICU).The follow-up of the maternal and fetal outcomes lasted till parturient and neonate were discharged from hospital.
Data analysis
Categorical data were presented as counts and percentage.The distribution of continuous variables was checked using visual inspection of the histogram.Variables normally distributed were reported as means and standard deviation (SD).The gestation period was reported as medians and quartiles.Thet-test was performed to compare the hospitalization time of the parturients and the fetal's one-minute Apgar score between different ASA grades or gestational weeks.The chi-square tests were performed to compare the postoperative ICU ratios of parturients in different ASA grades,gestation period,and intraoperative blood loss.The analyses were performed using the SPSS software(version 19.0,SPSS Inc.,Chicago,IL,USA).Pvalue<0.05 was considered statistically significant.
RESULTS
Patients and characteristics
Upon data from the electronic medical record system,totally there were 3789 patients receiving cesarean sections from January 1,2014 to December 31,2016.Among them 3680 cases were under neuraxial block,109 cases were under GA.The patient selection procedure is illustrated in Figure 1.In total,98 cases were enrolled in the study,with mean age of 31.3±4.6 years old,ranging from 14-48 years old.The median gestational week was 36.6 (34.3,38.7) weeks.There were 58(59.2%) cases of ASA grade Ⅰ-Ⅱ,40 (40.8%) cases of ASA grade Ⅲ-IV.Regarding intra-operative blood lose,there were 83 (84.7%) and 15 (15.3%) cases whose blood loss were < 800 ml and ≥ 800 ml,respectively.
Factors related to GA for cesarean section
The details of clinical characteristics for the enrolled cases who had GA for cesarean section regarding maternal and fetal factors were shown in Table 1.
Maternal and fetal outcomes
Outcomes of parturient
In 98 cases of CS under GA,compared with cases of ASA grade Ⅲ-IV,gestation period<37 weeks and intraoperative blood loss≥800 ml,the postoperative ICU ratio was lower in parturients with ASA grade Ⅰ-Ⅱ,gestation period≥37 weeks and intraoperative blood loss<800 ml (Table 2).The average hospitalization time of parturients with ASA score Ⅰ-Ⅱ were 6.9±3.3 days,which was significantly shorter than that of parturients with ASA score Ⅲ-IV (11.0±7.5 days,t=-2.99,P<0.05).The average hospitalization time of parturients with gestation period < 37 weeks were 11.0±8.4 days,which was significantly longer than that of parturients with gestation period ≥ 37 weeks (7.5±5.1 days,t=2.47,P<0.05).
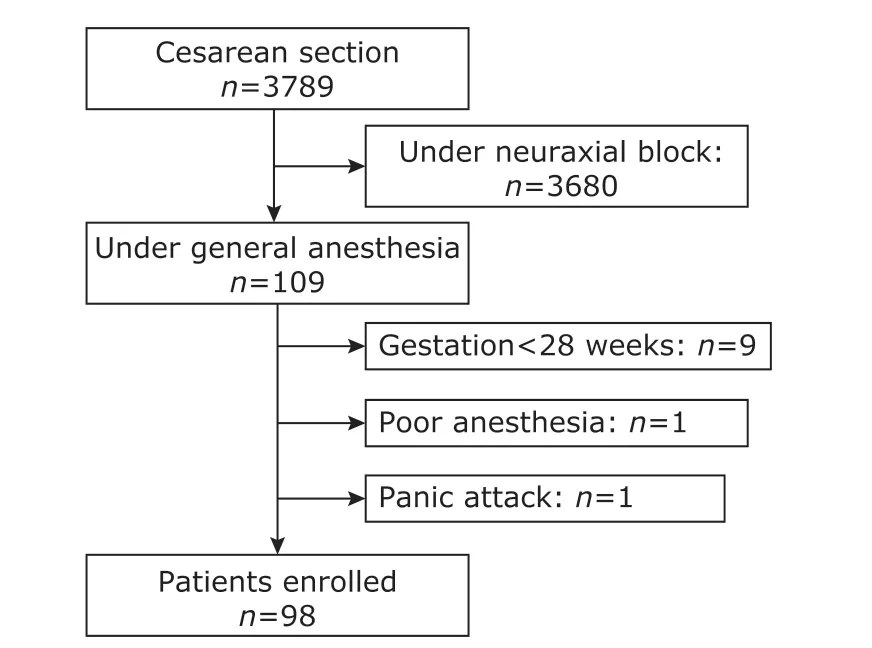
Figure 1.Flowchart of patients enrolling in this study.
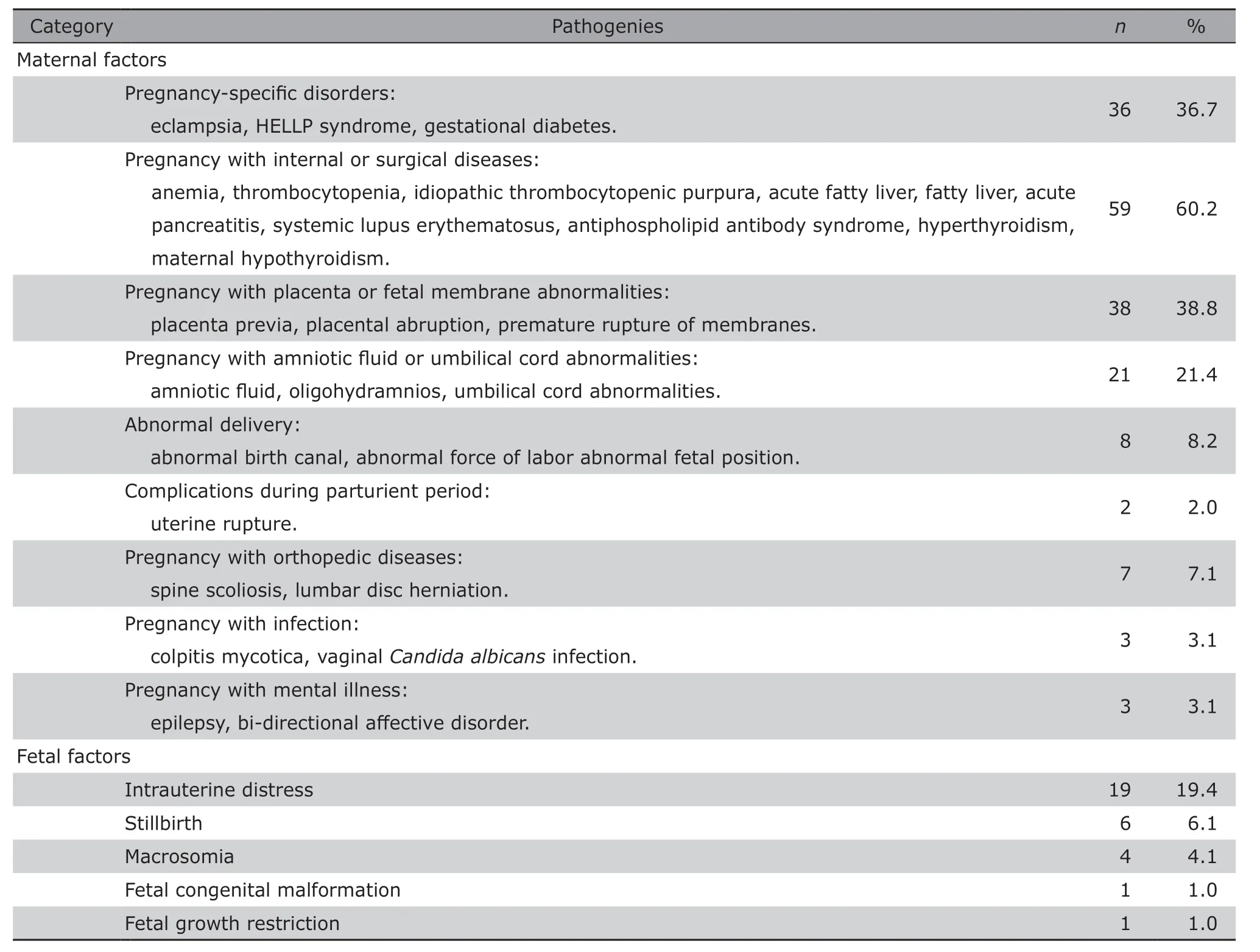
Table 1.Pathogenies of cesarean section under general anesthesia in PUMC Hospital (n=98)
Outcomes of neonates
In the 98 cases of CS under GA,5 neonates were stillborn,no Apgar score was collected.Of 12(12.2%)neonates who had one-minute Apgar score of 1-3,6(50.0%) died after surgery,and 6 (50.0%) neonates entered into the Neonatal Intensive Care Unit (NICU).Of 31(31.6%) neonates who had one-minute Apgar scores of 4-7,1 (3.2%) neonate died,22 (71.0%)neonates entered the NICU.In 50(51%) neonates whose one-minute Apgar score was 8-10,no postoperative neonatal death,12 (24%) neonates entered the NICU.
Among the 5 stillborn neonates,the shortest gestation period was 26+6weeks and the longest one was 38+5weeks;2 of parturients with ASA score Ⅱ,2 with ASA score Ⅲ,and 1 with ASA score IV.Among these 5 cases,4 cases with placental abruption;1 case with uterine rupture and hemorrhagic shock.The fetal one-minute Apgar scores of parturients with ASA grade Ⅰ-Ⅱ and whose gestation period<37 weeks were significantly lower than that of parturients with ASA grade Ⅲ-IV (t=2.21,P<0.05),and gestation period ≥37 weeks (t=-3.21,P<0.05)(Table 3).
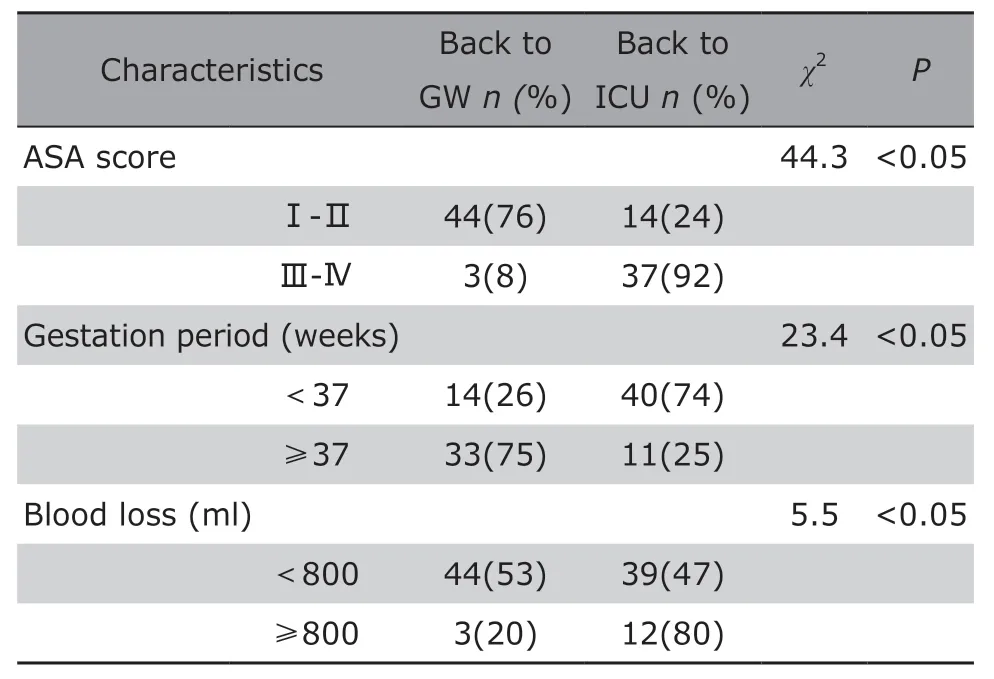
Table 2.Relationship of ASA score,gestation period and blood loss with the post-operative ICU care in parturients of cesarean section under general anesthesia (n=98)
DISCUSSION
Indications of GA for CS:factors of parturients
1.Pregnancy with internal or surgical diseases
Among internal and surgical diseases,women who have heart disease during pregnancy often present to the emergency center with obvious symptoms,such as wheezing,orthopnea,hypoxemia,and etc.The heart diseases include perinatal cardiomyopathy,decreased systolic function of left and right ventricular myocardium,pericardial effusion,pulmonary hypertension.These women need to undergo cesarean section to terminate pregnancy in order to reduce the burden on heart and lungs and save the mother and child.
Hypotension during spinal and epidural anesthesia is mainly a result of sympathetic blockade,which causes pooling of blood into the lower extremities3and sometimes can cause instability of breathing and circulation.Compared with neuraxial block,general anesthesia can achieve a steadier adjustment of anesthesia depth by adjusting the dosage of anesthetic,which enable to reduce the impact of anesthesia on cardiopulmonary function and ensure the safety of mother and child as much as possible.So in most of these cases,we chose general anesthesia,which was consistent with other medical groups.4
Besides,there are parturients with digestive diseases,acute pancreatitis,even systemic inflammatory response syndrome,etc.Pregnant women with these diseases often took urgent visit.The obstetricians need time to collect clinical data to determine whether patients need emergent cesarean section or not.Sometimes,parturients fail to cooperate with anesthesiol-ogists for neuraxial block due to a variety of reasons,such as pain or irritability.In this situation,general anesthesia may be more beneficial to women with high possibility of puncture failure,or those need exploratory laparotomy after cesarean section.
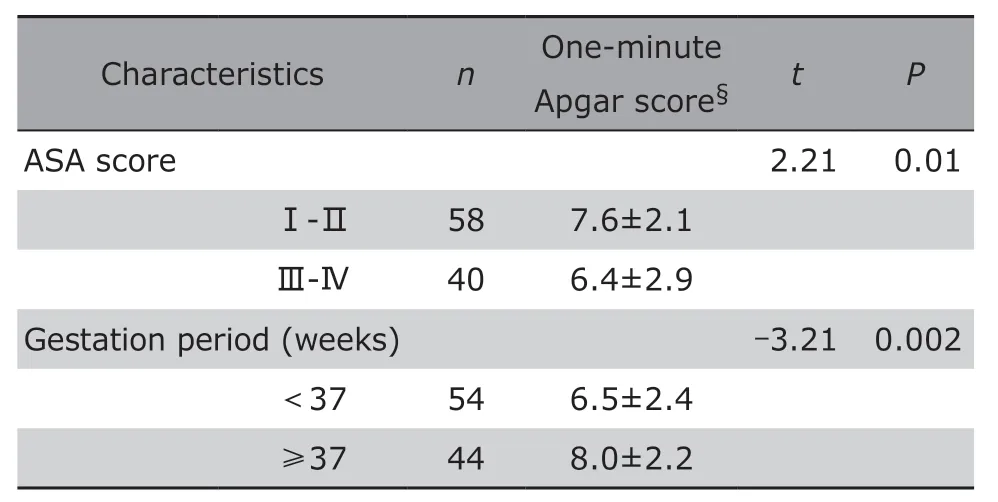
Table 3.Relationship of maternal ASA score,gestation period and neonate one-minute Apgar score in cesarean section under general anesthesia (n=98)
Other common internal diseases are platelet and coagulation disorders.Previous data have shown the thrombocytopenia (TP) affects 7%-10% of pregnant women.In recent years,many experts believe that the platelet count in a range of (75-100)×109is safe for spinal anesthesia applied to CS,and the platelet count under 50×109requires careful assessment on the overall situation whether spinal anesthesia can be applied.5In the current study,as some parturients were concurrent with idiopathic thrombocytopenic purpura,hemophilia,neuraxial block might cause serious consequences such as epidural hematoma,we applied GA to ensure patient's safety and reduce the risks of postoperative complications.6
2.Pregnancy with pregnancy-specific disorder
Experts from World Health Organization mentioned that about 6%-10% pregnant women developed pregnancy induced hypertension (PIH),7which is a common cause of death for parturients and neonates.In the cohort of our study,31% cases had pregnancy-specific hypertensive disorders,including pre-eclampsia,eclampsia,pregnancy with chronic hypertension,and chronic hypertension complicated by pre-eclampsia.For patients with poor controlled disease or in emergent situation,treatment should be cautious under close monitoring the condition of mother and neonates;and when necessary,terminate pregnancy at an appropriate time.In this situation,GA can achieve rapid induction and comprehensive effects of sedation,analgesia and muscle relaxant for the operation.
Another pregnancy-specific disease in this cohort is gestational diabetes mellitus (GDM).GDM is a risk factor for emergency CS.8Women with GDM had relatively higher possibilities to develop macrosomia,cephalopelvic disproportion,and dystocia.Therefore,GDM is a good indication of GA,especially for those who have to receive emergent CS or have unsuccessful neuraxial block due to obesity.
3.Pregnancy with placenta and fetal membrane abnormalities
Premature rupture of membranes(PROM) is a common disease during pregnancy and the incidence is about 4 per thousand.The subsequent complications include chorioamnionitis,pulmonary hypoplasia,restriction deformities,fetal loss,and complications of extreme prematurity among surviving neonates.9The preferred method for labor induction in the patient with PROM remains controversial.10
4.Pregnancy with orthopedic diseases
Because the orthopedic department of our hospital is well recognized for treating idiopathic scoliosis,there were 7 parturients with orthopedic diseases (all were spine-related diseases) in our cohort,which was relatively high.At present,contraindications for intraspinal anesthesia associated with the spine include:deformity,trauma,spinal tuberculosis,tumors,multiple sclerosis of spinal cord,meningitis,and skin infection near the puncture site.The 7 parturients above were all concurrent with lumbar disc herniation and scoliosis.Symptomatic lumbar disc herniation is the most common spinal pathology in pregnancy.Therefore,for parturient with spine-related orthopedic diseases,anesthesiologists need to be cautious about the contraindications of neuraxial block and carefully choose anesthetic method.GA is always a good option in this situation.
5.Pregnancy with mental illness
The prevalence of epilepsy in pregnant women was reported to be 0.3%-0.7%.11Over 90% of pregnancies in women with epilepsy did not develop any complication.12Although epilepsy is not a contraindication to any mode of anesthesia or analgesia, anesthesiologists should be alert about the effects of narcotics on epileptic patients.13It is reasonable to take the GA with Rapid Sequence Intubation (RSI) to terminate delivery quickly,because some commonly used anesthetics for GA,such as high-dose propofol13and midazolam14are antiepileptic.
Indications of GA for CS:factors of neonates
Stillbirth is mainly related with labor dystocia (prolonged obstructed labor and/or uterine rupture) and obstetric hemorrhage.Also,compared with cesarean delivery,women who have spontaneous vaginal delivery are with higher odds of stillbirth.14Therefore,for parturient with serious complications or in emergency situations, the proper surgical procedures,timing for surgery,parturients' physical and mental conditions,and their individual will should be considered comprehensively.It may be more appropriate to choose CS under GA.
Fetal distress occurs in 19% of the current cohort.Rapid reaction is crucial to achieve a delivery under urgent situation,and actions should be taken decisively to improve hypoxia status of the fetal.15There has been no universal consensus on an acceptable time to achieve delivery by caesarean section or vaginal assistance in condition of fetal distress.16At present,there is no conclusion about the influence of anesthetic methods on the prognosis of parturients and neonates after CS.A variety of anesthetic methods seem to be safe,but regional blockade shows more advantages on neonatal outcome.17
Maternal and fetal outcomes
In 98 cases of CS under GA,we found that for the parturients,ASA grade Ⅲ-IV,gestation period <37 weeks and intraoperative blood loss≥800 ml cases were related to high post-operative ICU care ratio.As the ASA grade defines the condition of the parturients,the overall mortality and complication mobility increase with increase of ASA grade.The shorter gestation period,the more urgent of the operation,and the higher risk for the parturient.With increase of intraoperative blood loss,the postoperative risk of a parturient increases.
For neonates,we chose the one-minute Apgar score to evaluate the outcome.The result showed ASA gradeⅢ-Ⅳ and gestation period <37 weeks were also the factors that related to the low one-minute Apgar score.
As we didn't compare the neonatal outcome between neuraxial block and GA,we can't provide evidence in which anesthetic method is better for the maternal and fetal outcomes.Some literatures showed no difference in neonatal outcomes between general and regional anesthesia for caesarean section when only out-of-risk newborns were analyzed.18But for the very preterm infants (27-32 weeks),multivariate analysis showed that neuraxial block was associated with an increased risk of neonatal death compared to GA,disregarding the gestational age,characteristics of pregnancy,delivery and neonates.19
In conclusion,pregnancy with internal or surgical diseases,including anemia,thrombocytopenia,idiopathic thrombocytopenic purpura,acute fatty liver,fatty liver,acute pancreatitis,systemic lupus erythematosus,antiphospholipid antibody syndrome,hyperthyroidism,maternal hypothyroidism,etc.,was the most common reason for choosing GA for CS.The indication of the anesthetic method is consistent with the Practice Guidelines for Obstetric Anesthesia,2in which the consultants and ASA members strongly suggest that (1) the decision to use a particular anesthetic technique for CS should be individualized,based on anesthetic,obstetric,or fetal risk factors (e.g.,elective vs.emergency),patient's preferences,and anesthesiologist's judgement;(2) consider selecting neuraxial techniques in preference to GA for most cases of CS;(3) GA may be the most appropriate choice in some circumstances,e.g.profound fetal bradycardia,ruptured uterus,severe hemorrhage,severe placental abruption,umbilical cord prolapse,and preterm footling breech.For parturients,with the increase of maternal ASA scores,the post-operative ICU care rate increased.For neonates,with the increase of Apgar scores,they showed better prognosis.
Conflict of interest statement
All authors declared no conflicting interests.
 Chinese Medical Sciences Journal2019年4期
Chinese Medical Sciences Journal2019年4期
- Chinese Medical Sciences Journal的其它文章
- Bevacizumab Combined with Icotinib Overcomes Osimertinib Resistance in a Patient of Non-Small Cell Lung Cancer
- An Optimized Protocol of Azoxymethane-Dextran Sodium Sulfate Induced Colorectal Tumor Model in Mice
- Ontology:Footstone for Strong Artificial Intelligence
- Antagonistic Effects of N-acetylcysteine on Mitogenactivated Protein Kinase Pathway Activation,Oxidative Stress and Inflammatory Responses in Rats with PM2.5Induced Lung Injuries
- Physiological Variables Associated with the Development of Acute Mountain Sickness
- Expression of PD1 and BTLA on the CD8+ T Cell and γδT Cell Subsets in Peripheral Blood of Non-Small Cell Lung Cancer Patients
