Expression of PD1 and BTLA on the CD8+ T Cell and γδT Cell Subsets in Peripheral Blood of Non-Small Cell Lung Cancer Patients
Yi Bao,Juanfen Mo,Jiayuan Wu,Chenxi Cao
1Central Laboratory,2Department of Oncology,The Second Hospital of Jiaxing City,Jiaxing,Zhejiang 314000,China
Key words:CD8+ T cell;γδ T cell;programmed cell death protein 1;B and T lymphocyte attenuator;non-small cell lung cancer
Objective To investigate the expression and regulation of programmed cell death protein 1 (PD1),B lymphocyte and T lymphocyte attenuator (BTLA) in peripheral blood of patients with non-small cell lung cancer (NSCLC);to examine the correlation of the mRNA levels between PD and BTLA in NSCLC.Methods Flow cytometry was used to detect the expression of PD1 and BTLA on the surfaces of CD8+ T cells and γδ+ T cells in the peripheral blood samples collected from 32 in-patients with stage IV NSCLC and 30 healthy individuals.We compared the expression of PD1 and BTLA on the surfaces of γδ+ T cells in the NSCLC patients with bone metastasis before and after the treatment of zoledronic acid.The correlations of PD1 and BTLA,as well as their ligands were analyzed using Pearson correlation analysis with the cBioPortal data platform.Results The frequency of PD1 on the surfaces of CD8+ T cells was significantly higher than that of the γδT cells in both healthy controls (t=2.324,P=0.024) and NSCLC patients(t=2.498,P=0.015).The frequency of PD1 on CD8+ T cells,rather than on γδ+ T cells,was significantly upregulated in advanced NSCLC patients compared with that in healthy controls (t=4.829,P<0.001).The PD1+ BTLA+γδT cells of the healthy controls were significantly lower than that of the NSCLC patients (t=2.422,P=0.0185).No differences in percentage of PD1+γδ+ and BTLA+γδ+ T cells were observed in 7 NSCLC patients with bone metastasis before and after zoledronic acid treatment.PD1 was positively correlated with BTLA in both lung adenocarcinoma (r=0.54;P<0.05) and lung squamous cell carcinoma (r=0.78;P<0.05).Conclusions The upregulation of co-inhibitory molecules occurs on the surfaces of both CD8+ T cells and γδT cells in advanced NSCLC,suggesting that these molecules were involved in regulating the inactivation of CD8+ T cells and γδ+ T cells,immune escape and tumor invasion.
LUNG cancer is the most common malignant tumor in China,with the top ranked morbidity and mortality rates.1Non-small cell lung cancer (NSCLC) accounts for about 85% of lung cancers in total.In recent years,adenocarcinoma has gradually taken over squamous cell carcinoma becoming the most common subtypes of NSCLC.The clinical application of immune checkpoint inhibitors such as programmed death protein 1 (PD1) and its ligand(PDL1) blockades has gradually changed the traditional strategies of the treatment for advanced NSCLC.2In June 2018,the National Medical Product Administration of China officially approved Nivolumab (OPDIVO?) for the treatment of locally advanced or metastatic NSCLC.This approval has shed light on the immunotherapy in cancer treatment.
According to differences in expression of T cell receptors (TCRs),human T lymphocytes are classified into αβT cells and γδT cells subtypes.3αβT cells are considered to be the dominant subtype of immune T cells and have the capacity of specifically recognizing antigens mediated by a major histocompatibility complex (MHC).4Unlike αβT cells,γδT cells represent a minor subset that does not require self-MHC-restricted priming,and are functionally similar to innate-like immune cells.5T cell activation is considered to be stimulated by double signals:the TCR recognition of the antigen-MHC molecular complex,followed by a second signal produced by the activation of co-stimulatory molecules.6However,to prevent the overactivation of T cells and the occurrence of autoimmune responses,co-inhibitory signals,such as cytotoxic T-lymphocyte antigen-4 (CTLA4),PD1 and the newly discovered signal B lymphocytes and T lymphocyte attenuator (BTLA),are also present on the surfaces of T cells.7The stimulation of these signal pathways provides negative regulatory signals to suppress over-activation of T cells.8
In this study,we examined the expression of PD1 and BTLA on the surfaces of CD8+T cells and γδ+T cells in patients with advanced NSCLC and healthy individuals,and explored whether zoledronic acid regulates these co-inhibitory molecules in NSCLC patients with bone metastasis;additionally,the corrections of gene expression profiles,including PD1 and BTLA,as well as their ligands were studied using The Cancer Genome Atlas(TCGA) NSCLC datasets.This study provides preliminary data for understanding the effectiveness of using adoptive T immunotherapy and checkpoint inhibitors against PD1/PDL1 pathway in the treatment of lung cancer.
PATIENTS AND METHODS
Subject recruitment and sample preparation
The study was approved by the ethics committee of the second hospital of Jiaxing City(20181102h01),and informed consents were obtained by patients and healthy volunteers who provided the blood samples.Blood specimens were collected from 32 in-patients with stage IV NSCLC from January 2016 to June 2017.There were 24 (75%) males and 8 (25%)females,with mean age of 60.6±1.6 years old.The diagnosis of NSCLC was confirmed by pathology,including adenocarcinoma (n=20) and squamous cell carcinoma (n=12).The TNM staging was based on the criteria of the American Joint Committee on Cancer (AJCC) staging manual (8thedition).9Among these 32 patients,there were 7 patients with bone metastasis,and we collected their blood specimen before and 3 weeks after zoledronic acid treatment (a single 4 mg dose intravenous infusion).We recruited 30 healthy volunteers for controls,including 17 males and 13 females,with mean age of 57.5± 1.8 years old.
Blood specimen collection
We collected 2 mL peripheral blood from each fasting subject using sodium citrate dipotassium anticoagulant tubes.All blood samples were sent for examinations within 24 hours.
Flow cytometry staining
To determine the frequency of co-inhibitory biomarkers on the surface of γδ T cells,we conducted multicolored immunofluorescence staining using freshly collected blood specimens from all subjects.The antibodies were conjugated to fluorescent markers as follows:CD3-PE-Cy5.5,TCR γδ-APC,PD1-FITC,BTLA-PE,and CD8-APC-CY7.The mouse IgG1 with fluorescent markers,including PE-Cy5.5,APC,FITC and PE,were used as isotype controls (BD Biosciences).For extracellular staining,50 mL blood sample was incubated with different combinations of fluorochrome-coupled antibodies (10 ml of each antibody).After 20 min incubation at room temperature,cells were washed twice with 1X PBS and flow cytometry was performed using a flow cytometer (BD FACSCanto II,BD Biosciences,USA).Data were collected and analyzed with DIVA software (version 6.1.3;BD Biosciences,San Jose,CA,USA).
Datasets extraction
The NSCLC mRNA expression datasets were obtained from http://www.cbioportal.org,including 586 lung adenocarcinoma samples and 511 lung squamous cell carcinoma samples derived from TCGA.The cBioportal data analysis platform6was used to study correlations of the expressions between PD1 and BTLA,PD1 and its receptor PDL1,BTLA and its receptor herpes virus entry mediator (HVEM).
Statistical analysis
Data were presented as mean ± standard deviation.Unpaired Student'st-test or pairedt-test was used for comparisons between groups.Pearson correlation analyses were performed to analyze correlations of mRNA levels of genes expression using the TCGA database.The Pearson correlation coefficient≥0.4 was defined as medium-degree correlation,and≤0.2 was defined as no correlation.GraphPad Prism (version 5,GraphPad Software Inc.,La Jolla,CA,USA) was used for all statistical calculation and figure generation.Pvalue<0.05 indicates statistical significance.
RESULTS
Expression of PD1 and BTLA on the surfaces of CD8+ and γδ+ T lymphocytes in the peripheral blood of healthy controls
To assess the frequency of PD1 and BTLA on the surface of CD8+and γδ+T cells in peripheral blood of healthy individuals,lymphocytes were first gated on the basis of a forward scatter/side scatter (FSC/SSC) profile,followed by CD8+and γδ+T cell analyses in a gated population with CD3+staining.PD1 and BTLA antibodies were used to determine the percentage of PD1 and BTLA positive CD8+and BTLA+γδ+T cells (Figure 1A).The results showed that the percentages of PD1+CD8+T cells and PD1+γδ+T cells were 10.97%±0.91% and 7.70%±1.07%,respectively,with a statistically significant difference (t=2.324,P=0.024)(Figure 1B).The percentages of BTLA+CD8+T cells and BTLA+γδ+T cells were 54.89%±3.05% and 57.16%±4.02%,respectively,and there was no significant difference between the two groups (t=0.449,P=0.67) (Figure 1C).
Expression of PD1 and BTLA on the surfaces of CD8+ and γδ+ T lymphocytes in patients with advanced NSCLC
The gating strategy was the same as that in Figure 1A.In the peripheral blood of advanced NSCLC,the percentages of PD1+CD8+T cells and PD1+γδ+T cells were 19.85±1.58% and 12.45%±2.51%,respectively,with statistically significant differences (t=2.498,P=0.015) (Figure 2A),and the percentages of BTLA+CD8+and BTLA+γδ+T cells were 56.71%±3.64%and 56.68%±4.41%,respectively,with no significant difference (t=0.004,P=0.997) (Figure 2B).The frequency of PD1+CD8+T cells between patients with NSCLC and healthy controls were 19.85%±1.58%and 10.97%±0.91%,respectively,with significant difference observed between the two groups (t=4.829,P<0.001) (Figure 2C).NSCLC patients tend to have higher percentage of PD1+γδ+T cells than the healthy controls (12.45%±2.51%vs.7.70%±1.07%),but the statistics failed to show a significant difference(t=1.709,P=0.09) (Figure 2D).We did not observe any difference in the BTLA+CD8+and BTLA+γδ+T lymphocytes between healthy controls and patients with advanced NSCLC (Figure 2E-F).
Proportion of PD1+ BTLA+ γδ+ T cells in the peripheral blood of NSCLC patients
Using the gating strategy shown in Figure 1A,the double positive expression of PD1 and BTLA on the surfaces of γδ+T cells in the peripheral blood of the study subjects was analyzed.The percentages of PD1+BTLA+γδ+T cells in healthy controls and NSCLC patients were 5.05%±1.08% and 12.08%±2.55%respectively,with a statistically significant difference(t=2.422,P=0.0185) (Figure 3).
Changes in γδ+ T cells and co-inhibitory molecules after zoledronic acid treatment in NSCLC patients with bone metastases
In 7 NSCLC patients with bone metastases treated with zoledronic acid,the frequency of the γδ+TCR cell population was 3.57%±0.69% before the treatment and 10.83%±3.80% 3 weeks after the treatment,with an increasing trend,but the difference was not statistically significant (t=2.010,P=0.064).Moreover,we did not observe any differences in the percentages of PD1+γδ+and BTLA+γδ+cell before and after zoledronic acid treatment (Figure 4).
Correlation of mRNA levels of PD1,BTLA and their ligands in NSCLC
Using the gene expression profiles of lung adenocarcinoma and lung squamous cell carcinoma from the TCGA database,we further analyzed the correlations of mRNA levels between PD1 and PD-L1,PD1 and BTLA,BTLA and HVEM in tumor tissues (Figure 5).In lung adenocarcinoma (AC),PD1 and its ligand PD-L1 showed a slightly positive correlation (r=0.33);a significant positive correlation between PD1 and BTLA was observed(r=0.54,P<0.05);BTLA and its ligand HVEM were slightly correlated (r=0.23).In lung squamous cell carcinoma (SCC),PD1 and its ligand PD-L1 was barely correlated (r=0.18);a strong positive correlation was observed between PD1 and BTLA (r=0.78,P<0.05);BTLA and its ligand HVEM also showed a positive correlation (r=0.48,P<0.05).
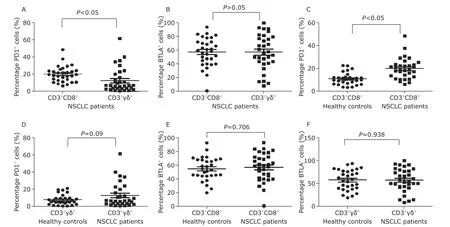
Figure 2.PD1 and BTLA expression on the surface of CD8+ T cells and γδ+ T cells in peripheral blood of advanced NSCLC and healthy controls.A.Higher percentage of PD1+ cells was observed in CD3+CD8+ T cells than CD3+γδ+ T cells;B.the percentage of BTLA+ cells in CD3+CD8+ T cell was not significant different from CD3+γδ+ T cells;C.the percentage of PD1+ cells in CD3+CD8+ T cells of NSCLC was higher than that of healthy controls;D.the percentage of PD1+ cells in CD3+γδ+ T cells of NSCLC patients appeared to be higher than that of healthy controls with no significant difference;E and F.the percentage of BTLA+ cells in CD3+CD8+ T cell and in CD3+γδ+ T cells was not significant different between NSCLC patients and healthy individuals.
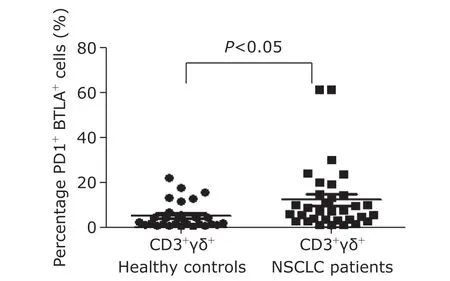
Figure 3.The positive expression of PD1 and BTLA on the surface of CD3+γδ+ T cells between healthy controls and patients with NSCLC.
DISCUSSION
This study suggested that the co-inhibitory molecules PD1 and BTLA were both present on the surfaces of CD8+T cells and γδ+T cells.In both NSCLC patients and healthy individuals,the PD1 expression on circulating CD8+T cells were significantly higher than those on γδ+T cells,but there was no significant difference in the expression of BTLA between CD8+T cells and γδ+T cells.In addition,the percentage of PD1+CD8+in the peripheral blood in NSCLC patients was higher than in healthy individuals;a similar trend was also observed in PD1+γδ+T cells,but no statistically significant difference was observed.The proportions of neither BTLA+CD8+T cells nor BTLA+γδ+T cells in peripheral T cell was different between healthy individuals and patients with advanced NSCLC;however,the frequency of PD1+BTLA+γδ+T cells was higher in NSCLC patients than that in healthy individuals.
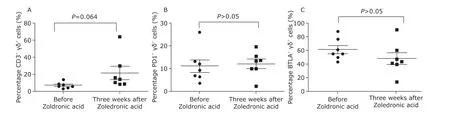
Figure 4.The frequency changes of γδ+ cells before and after zoledronic acid treatment in the NSCLC patients with bone metastasis.A.CD3+γδ+ T cells;B.PD1+γδ+ T cells;C.BTLA+γδ+ T cells.
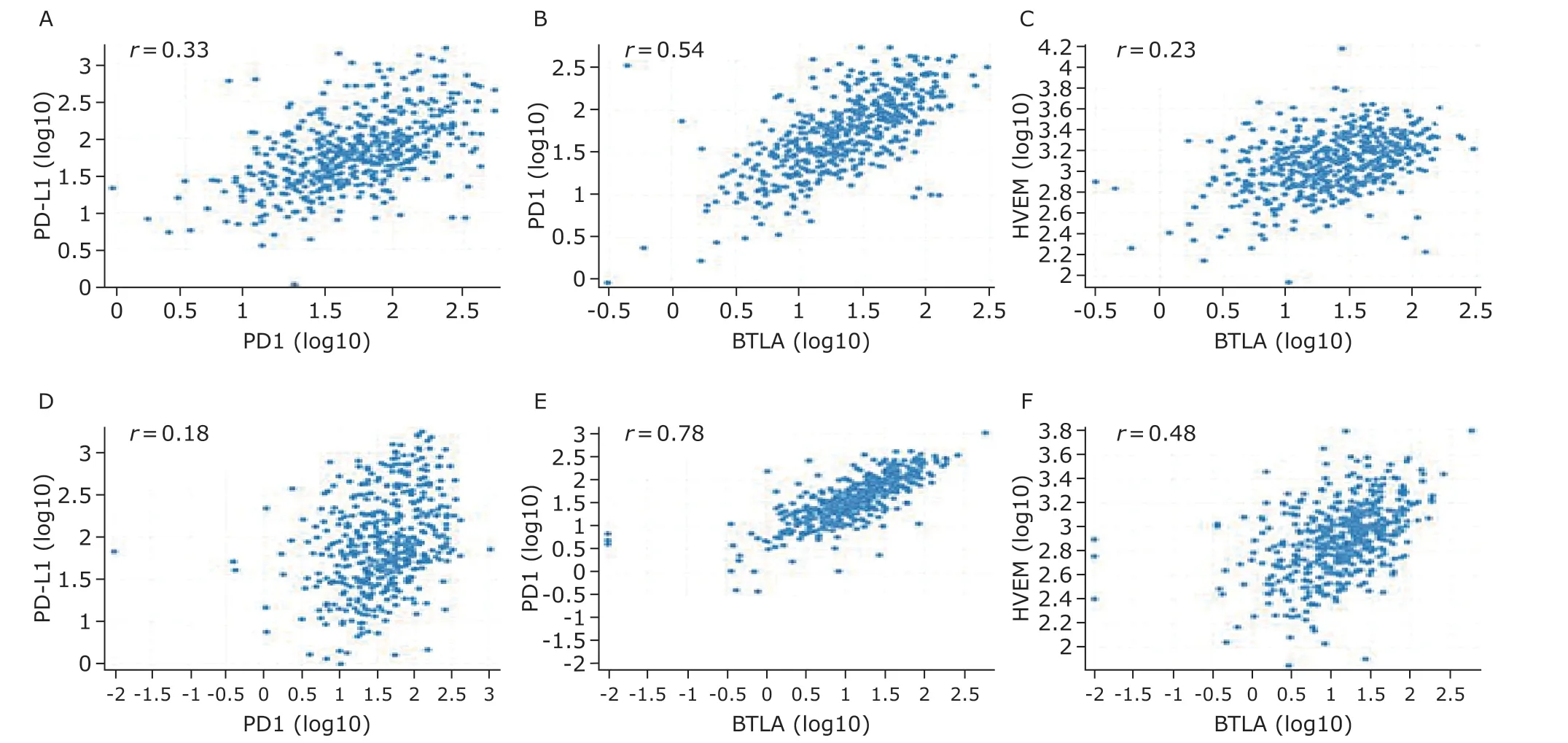
Figure 5.Scatter plots of correlations between PD1 and BTLA gene expressions,and correlations with their corresponding ligands.A.Between PD1 and PDL1 in lung AC;B.between PD1 and BTLA in lung AC;C.between BTLA and HVEM in lung AC;D.between PD1 and PDL1 in lung SC;E.between PD1 and BTLA lung SC;F.between BTLA and HVEM in lung SC.AC,adenocarcinoma;SC,squamous cell carcinoma.
PD1 and BTLA are two co-inhibitory molecules that have been extensively studied in recent years,especially PD1.PD1 is widely expressed on the surfaces of T cells,B cells,and nature killer cells (NK cells).10The expression of PD1 on the resting T cells is very low in healthy individuals.11After the activation of T cells,PD1 is transiently upregulated on the surface of the cells;but the expression of PD1 will be downregulated when these T cells are ready to exert cytotoxic effects.12The continuously higher expression of PD1 is present on the surface of exhausted T cells.13During the upregulation of PD1 expression,this molecule can bind to its ligand PDL1 on the surfaces of tumor cells.The activation of the PD1/PDL1 pathway leads to T cell inactivation and exerts immunosuppressive effects.12Currently,the effectiveness of preclinical trials of monoclonal antibodies targeting PD1/PDL1 molecules is mainly reported in the treatment malignant melanoma and NSCLC,13and these antibodies have been approved for clinical use in several countries,including China.PD1 can also be rapidly upregulated on the surfaces of γδ+T cells after activation in the peripheral blood of healthy individuals,and mainly expressed on the terminal effector memory T cells(CD45RA+CD27-) γδ+T subpopulation.14However,the expression pattern of PD1 on γδ+T cells in peripheral blood of the patients with advanced lung cancer is unclear.Our results showed that the expression of PD1 on the surfaces of CD8+T cells and γδ+T cells was upregulated in patients with advanced NSCLC,and more obviously on CD8+T cells,suggesting that the presence of higher percentages of exhausted CD8+T and γδ+T cells in the circulation during the progress of NSCLC leads to a loss of the ability to eliminate cancer and may be associated with the occurrence of immune escape and failure of immunotherapy.15Indeed,blocking the PD1/PDL1 signaling pathway has been approved as a therapeutic strategy in the treatment of NSCLC,and our data suggest that in addition to CD8+T cells,the downregulation of PD1 on the surfaces of γδ+T cells may also be associated with enhanced antitumor responses and tumor regression.
BTLA is another negative costimulatory molecule discovered recently.It is a type I transmembrane glycoprotein distributed on the surfaces of cell membranes.16BTLA is highly expressed in T cells and has also been detected on the surfaces of B cells,NK cells,macrophages and dendritic cells at different expression levels.17BTLA is expressed on both the mature αβT cells and γδT lymphocytes in the peripheral blood,but not expressed on regulatory T cells.18BTLA ligand,HVEM,belongs to the family of tumor necrosis factor receptors.HVEM is widely expressed in the peripheral blood,including T cells and B cells,and can produce inhibitory signals by binding to BTLA through its specific domain.19
In a recent study using adoptive tumor infiltrating lymphocytes (TIL) immunotherapy in patients with advanced malignant melanoma,after infusingin vitroexpanded T lymphocytes isolated from tumor tissues,the researchers found that the patients who responded well to the treatment had a higher percentage of BTLA+CD8+T cells in the expanded TIL cells,but it was unclear whether these exogenously large amounts of BTLA+CD8+T cells play any role.20In our study,there was no significant difference in the expression of BTLA on either CD8+T cells or γδ+T cells between healthy controls and lung cancer patients,however,we found a high proportion of PD1+BTLA+γδ+T in advanced NSCLC patients.These results in our study may be essential to further clarify the roles of BTLA+/HVEM in the progression of NSCLC.
By analyzing gene expression profiles from the NSCLC TCGA data sets,we found a positive correlation between PD1 and BTLA in the tumor tissues of NSCLC patients.Since we did not obtain tumor tissues from all the NSCLC patients in this study,it may be hard to get a directive conclusion regarding the correlation of PD1 and BTLA by using TCGA data sets.Nevertheless,the current data provide clues for future studies.Interestingly,in a recent study which characterized lung cancer into epithelial subtype and mesenchymal subtype,both upregulated gene and protein expressions of PD1 and BTLA were observed in tumor tissues derived from the mesenchymal subtype of lung cancer rather than the epithelial subtype.This finding indicated the two inhibitory molecules and their associated signaling pathways may be involved in epithelial-mesenchymal transition (EMT),drug resistance and poor prognosis of lung cancer.21
We compared the proportional changes of γδ+T cells,PD1+γδ+and BTLA+γδ+T cells in lung cancer patients with bone metastases before and after zoledronic acid treatment.Zoledronic acid is a commonly used medicine which slows down bone resorption and allows bone remodeling.It has shown that zoledronic acid has a capacityin vitroto promote a large scale of γδT cells expansion,which is used as a candidate of the adoptive T cell immunotherapy.We found that after three weeks of zoledronic acid administration,there appeared an increasing trend of γδ+T cells in peripheral blood of advanced NSCLC patients,especially in patients younger than 50 years old.However,the difference was not statistically significant,which might be due to the small number of cases in this study.We did not find any change of PD1 or BTLA expression on the surfaces of γδ+T cells before and after zoledronic acid treatment.Further studies with large samples are needed to draw a clear conclusion.Previous studies have shown that Vγ9Vδ2,the most dominant γδT cell in peripheral blood,can be largely expandedin vitroby small phosphorylated non-peptide antigens,including isopentenyl pyrophosphate and zoledronic acid.22,23A retrospective study has shown that zoledronic acid is associated with a prolonged overall survival in the patients with breast cancer.24However,in vivoproliferation of γδT cells by zoledronic acid may be affected by the age of patient as well as the treatments patient received,such as chemotherapy.
Overall,the PD1/PDL1 and BTLA/HVEM inhibitory signaling pathways are involved in tumor cell escape.By studying the expression and regulation of PD1 and BTLA on T cells,we provide important preliminary data for understanding the effectiveness of immunotherapy in the treatment of lung cancer.
Conflict of interest statement
All authors declared no conflicting interests in this study.
 Chinese Medical Sciences Journal2019年4期
Chinese Medical Sciences Journal2019年4期
- Chinese Medical Sciences Journal的其它文章
- Bevacizumab Combined with Icotinib Overcomes Osimertinib Resistance in a Patient of Non-Small Cell Lung Cancer
- An Optimized Protocol of Azoxymethane-Dextran Sodium Sulfate Induced Colorectal Tumor Model in Mice
- Ontology:Footstone for Strong Artificial Intelligence
- Antagonistic Effects of N-acetylcysteine on Mitogenactivated Protein Kinase Pathway Activation,Oxidative Stress and Inflammatory Responses in Rats with PM2.5Induced Lung Injuries
- Physiological Variables Associated with the Development of Acute Mountain Sickness
- A Single-center Retrospective Cohort Study on Cesarean Section under General Anesthesia
