Rural congestive heart failure mortality among US elderly,1999–2013: Identifying counties with promising outcomes and opportunities for implementation research
Maria C. Mejia de Grubb, Robert S. Levine, Barbara Kilbourne, Baqar A. Husaini,Tyler Skelton, Lisa Gittner, Michael A. Langston, George E. Rust
Rural congestive heart failure mortality among US elderly,1999–2013: Identifying counties with promising outcomes and opportunities for implementation research
Maria C. Mejia de Grubb1, Robert S. Levine1, Barbara Kilbourne2, Baqar A. Husaini3,Tyler Skelton1, Lisa Gittner4, Michael A. Langston5, George E. Rust6
Objective:Describe modern trends in congestive heart failure (CHF) among elderly(>65 years of age) in the United States, to identify potentially successful rural areas. Compare CHF mortality using multiple- (MCOD) versus underlying-(UCOD) cause of death data.
Methods:U.S. Centers for Disease Control and Prevention mortality files (WONDER internet site).
Results:Using MCOD data, overall mortality rates/100,000 population (and 95% confidence intervals) for CHF among persons >65 years of age (1999–2013) were 482.0 (481.2–482.8) for large central and large fringe metropolitan (LCLF) counties, 549.6 (548.6–550.7) in small and medium metropolitan (SM) counties, and 652.6 (650.9–654.0) in micropolitan and non-core,non-metropolitan (MNCNM) counties. Twenty positive deviance NCNM counties (collectively including 198,581 residents >65 years of age) had an overall CHF rate of 300.9 (275.0–326.9) in 2013. This was significantly lower than the LCLF rate for 2013 (482.0 [481.2–482.8]), and represented a reduction of 47% since 1999. Overall CHF occurrence as estimated with MCOD was 3.4-fold higher than that obtained with UCOD.
Conclusion:These data illustrate underestimation of CHF by UCOD data and the importance of correct death certification. Rural CHF mortality rates are higher than urban rates, but some positive deviance counties demonstrate that this is not inevitable. Further research is needed to understand the relative contribution of research innovation, medical care, and public health to rural-urban disparities and the relative success of positive deviance counties.
Congestive heart failure; elderly; mortality; rural
Introduction
Despite advances in health care, the occurrence of congestive heart failure (CHF) remains high in the United States (US), and poses daunting challenges to public health. CHF has been reported to be the second leading cause of hospitalization among patients between 65 and 84 years of age, and the leading cause of hospitalization among persons >85 years of age [1]. Approximately one-half of patients diagnosed with CHF will die within 5 years[2]. In 2011 Medicare spent 28% of its payments on care in the last 6 months of life [3].Therefore, caring for patients with CHF notonly increases already high end-of-life costs, but also reflects the more than 50% of Medicare patients with CHF who are readmitted within 6 months of hospital discharge [4–6].
Although Medicare hospitalization rates for CHF declined by 29.5% from 1998 to 2008, the relative decline in riskadjusted 1-year CHF mortality rates was only 6.6% (from 31.7% to 29.6%) for the same time period [5]. Chen et al. [5]reported significant racial disparities, with lesser declines in hospitalization rates for black persons with CHF. There was significant geographic variation as well (e.g., mortality declining in 4 states, but increasing in 5 states) [5].
Rural residence may pose special problems in CHF care,even in health care systems outside the US where there is universal coverage [7, 8]. Within the US, studies have shown both an increased frequency of CHF admissions and barriers to early physician follow-up in rural areas [5, 9]. Nevertheless,several previous reports have shown that poor outcomes from various causes are not inevitable, even among high-risk populations [10–13]. Moreover, we have shown that for stroke and heart disease, reductions in mortality of >50% are associated with simultaneous, but not necessarily integrated advances in scientific innovation, clinical implementation, and public health [13]. The present report addresses these issues in the context of the explanatory hypotheses they have inspired systems of care for US elderly in rural areas of the US.
Methods
Mortality data were obtained from the publically available WideRanging ON-line Data for Epidemiologic Research(WONDER) internet site provided by the US Centers for Disease Control and Prevention (National Center for Health Statistics) [14]. The Baylor College of Medicine Institutional Review Board considers such public data to be exempt from review. Except for comparative purposes, we used multiple cause of death (MCOD) data instead of the compressed mortality file (CMF). CMF and MCOD are national, county-level mortality data based on death certificates for US residents.Each death certificate contains a single underlying cause of death and up to 20 additional contributory causes. Typically,the certification of these causes is done by the physician who attends the death. CMF data is based on the underlying cause of death. MCOD data speci fies the underlying cause of death,but also includes contributory causes. We used MCOD, in part because it has been observed that methods relying on determination of a single underlying cause of death among the elderly may yield underestimates of the extent to which multiple problems contribute [15]. Moreover, instructions for completing death certificates state that when system failures, such as CHF,are listed, the system failure must be immediately followed by the etiology [16]. Death certificates which simply identify CHF as the underlying cause of death are considered coding errors.To document differences in reporting frequencies between MCOD and CMF data, we compared rates of occurrence for CHF when listed as an underlying cause of death (Compressed Mortality Data – International Classification of Diseases[10th edition] codes I150 [CHF], I111.0 [hypertensive heart disease with CHF], I113.0 [hypertensive heart and renal disease with CHF], and I113.2 [hypertensive heart disease with both CHF and renal failure]) and when listed anywhere on the death certificate (specified as the combined appearance of the aforementioned ICD-10 codes and any other ICD-10 code –MCOD data).
Because information on Hispanic or Latino ethnicity(Hispanic) is not available before 1999, we restricted our descriptions to the 15-year period between 1999 and 2013, the most recent years for which data is available. Methods used for calculating age-adjusted rates (year 2000 standard population), 95% CIs, and for classifying urbanization are available from the WONDER site. In the present descriptions, urbanization follows the National Center for Health Statistics classifi-cation (large central and large fringe metropolitan [aggregated here as LCLFM], small and medium metropolitan [SMM],small metropolitan [SM], micropolitan [non-metropolitan]and non-core-non-metropolitan [MNCNM]; version of 2013)[8, 17]. To assure stable rates per National Center for Health Statistics criteria, we restricted these descriptions to places with at least 20 cases (deaths) in the numerator of each rate.
A two-step process was used to identify potentially successful positive deviant counties. First, MCOD data for 2013 were used to identify MNCNM (rural) counties in which the overall CHF mortality comprised the lowest 2.4% of the 781 MNCNM counties based on a log normal transformation of the rates (skewness =0.05) with Stats Direct software(Stats Direct 2.7.9; Stats Direct, Ltd., Cheshire, UK). These data were defined as potentially successful positive deviants.Although the 2.4% criterion would have yielded 19 of the 781 MNCNM counties, the rate for the county with the 19th highest rate equaled that for the county with the 20th highest rate, thus both were included. We then tracked the yearly rates for overall CHF mortality among persons >65 years of age in these counties, along with comparable data for all LMLFM,SM, and MNCNM counties from 1999 to 2013. The percent change in overall CHF mortality among persons >65 years of age for each group (year 2 [2013] – year 1 [1999])/(year 1[1999]*100) was then calculated for each group.
Results
CHF mortality according to demographic factors
Figure 1 shows the age-adjusted rates of CHF as recorded in MCOD data for non-Hispanic elderly persons (>65 years of age) in the US according to US Census-defined categories of race (Asian or Pacific Islander, American Indian or Alaska Native, black or African American, or white), gender (male or female), and urbanization (LCLFM, SM, or MNCNM). Fig. 2 shows the same types of rates for Hispanic residents. Overall,the rates were highest among non-Hispanic blacks or African Americans (blacks), followed by non-Hispanic whites and Hispanic whites. Within each group, rates were higher among men. Interestingly, the Hispanic advantage, which is present for other groups, is not apparent among Hispanic Asian and Pacific Islanders residing outside LCLFM areas. Regardless of race, gender, or ethnicity, the rates were highest in MNCNM counties.
Comparing compressed(underlying cause of death)and multiple causes of death data
Table 1 presents a comparison of MCOD and CMF data for non-Hispanic and Hispanic blacks and whites according to levels of urbanization. Although general patterns are similar(e.g., the rural rates are highest), the rates and total numbers of deaths are 3.4-fold lower when CMF data is used.
Geographic variation in CHF mortality
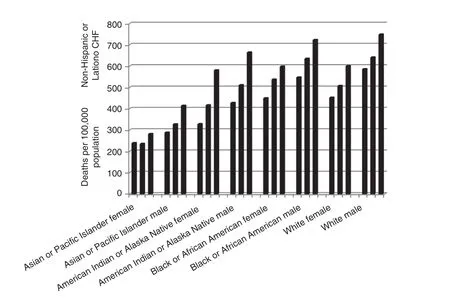
Fig. 1. Non-Hispanic or Latino congestive heart failure occurrence at death (age-adjusted, 65–85+ years) according to race, gender, and urbanization (large central and large fringe metro, middle and small Metro, and non-core, non-metro). Multiple causes of death data, US,1999–2013.
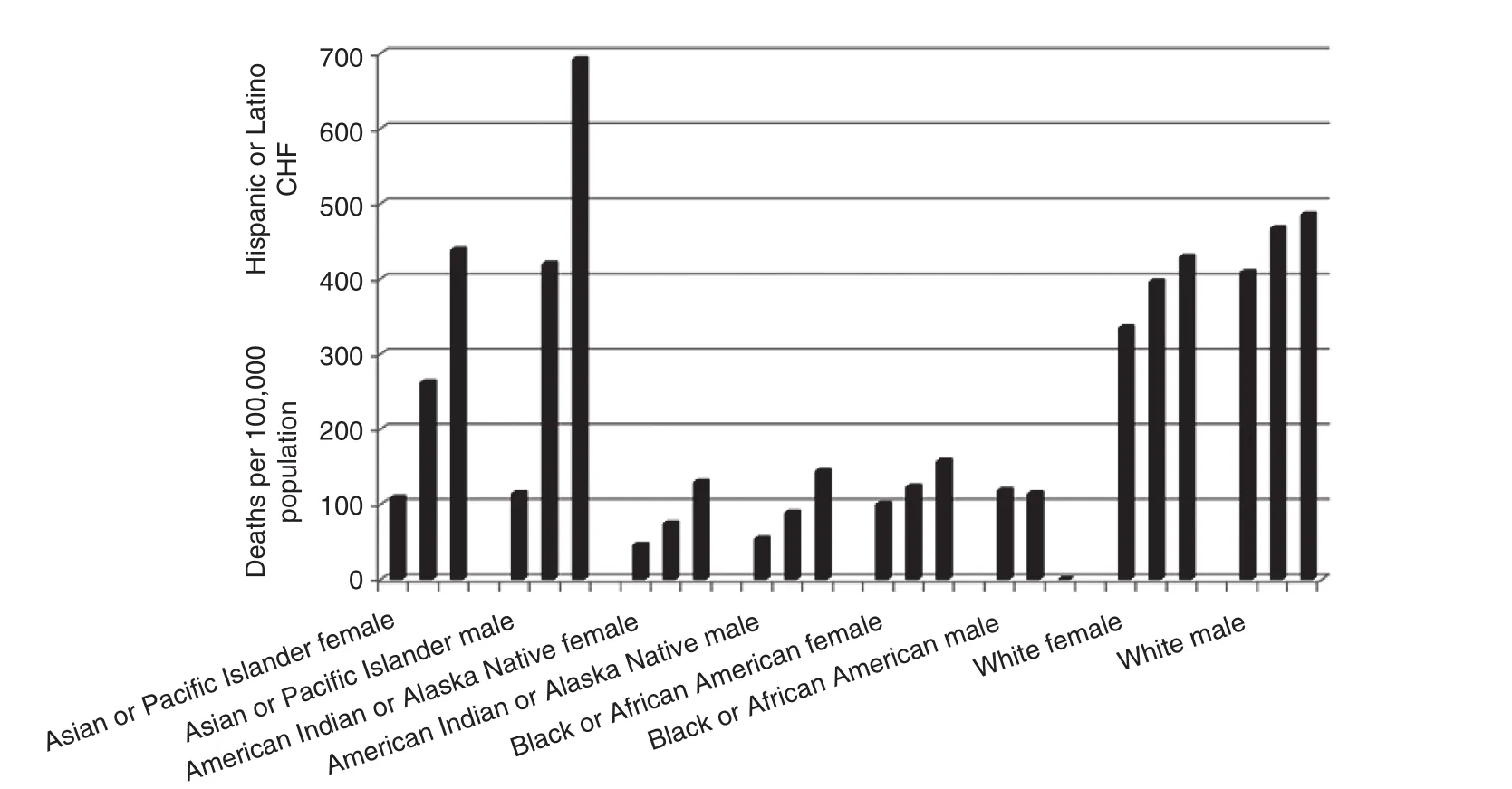
Fig. 2. Hispanic or Latino congestive heart failure occurrence at death (age-adjusted, 65–85+ years) according to race, gender, and urbanization(large central and large fringe metro, middle and small metro, and non-core, non-metro). Multiple causes of death, US, 1999–2013.
Table 2 shows the age-adjusted mortality rates and 95% CIs among the elderly according to race (black or white), gender,ethnicity (Hispanic or non-Hispanic), and US census division.The highest (boldface italics) and lowest (boldface) divisions are noted for each demographic category. With the exception of Hispanic black women (for whom the South Atlantic Division had the highest rates), either the East South Central Census Division (Alabama, Kentucky, Mississippi, and Tennessee) or the West South Central Census Division (Arkansas, Louisiana,Oklahoma, and Texas) had the highest rates. The highest and lowest census divisions were more variable for other demographic groups.
Identifying potentially successful rural counties
Figure 3 depicts the county level age-adjusted CHF mortality among non-Hispanic elderly whites in 1911 counties according to urbanization for the year 2013. The figure shows that even though MNCNM counties had the highest overall CHF rates,there were counties within this high-risk group in which the race-specific rates were equivalent to the lowest rates among LCLFM counties. Comparable results were not detected for non-Hispanic blacks or Hispanic whites (data not shown).
The 20 potentially successful positive deviant MNCNM counties were distributed across the US as follows: Baxter,AR; Monroe, FL; Whiteside, IL; Clinton and Jasper, IA;Reno, KS; Madison, KY; St. Landry Parish, LA; Talbot,MD; Newaygo, MI; Winona, MN; Flathead and Gallatin,MT; Douglas, NV; Grafton, NH; Greene, NY; Moore,Transylvania, NC; Greenwood, SC; Llano and Walker, TX;Pittsylvania, VA; Shenandoah, VA; and Door, WI. In 2013,a total of 198,581 people >65 years of age resided in these counties, equal to 2.5% of the 7,994,277 people >65 years of age residing in comparable rural areas. Sixteen of the counties were in the micropolitan group, although four (Newago,Greene, Shenandoah, and Door) were non-core, non-metro.Overall, 56% of the rural counties were in the micropolitan group. Further delineation of individual or contextual features of these counties is beyond the scope of the present report.
Figure 4 depicts the yearly time course of overall, ageadjusted (>65 years of age) CHF mortality in the 20 potentially successful positive deviant counties, as well as comparable data for overall CHF mortality in the LCLFM, SM, and MNCNM counties. Although the 20 potentially successful positive deviant counties began the observation period (1999)with an overall rate (569.0 [530.5–607.6]) approximating that of the LMLFM counties (580.2 [576.2–607.6]), the rate was 300.9 (275.0-326.9) in 2013, a reduction of 47%. LMLCM counties, in contrast, were 442.9 (439.2–446.1) in 2013, a reduction of 24%. Corresponding changes for SM counties were from 600.7 (603.7–613.7) in 1999 to 498.6 (494.6–502.6)in 2013 (an 18% reduction), and for MNCNM counties from 720.4 (713.7–727.1) in 1999 to 583.1 (577.4–588.7) in 2013(a 19% reduction).
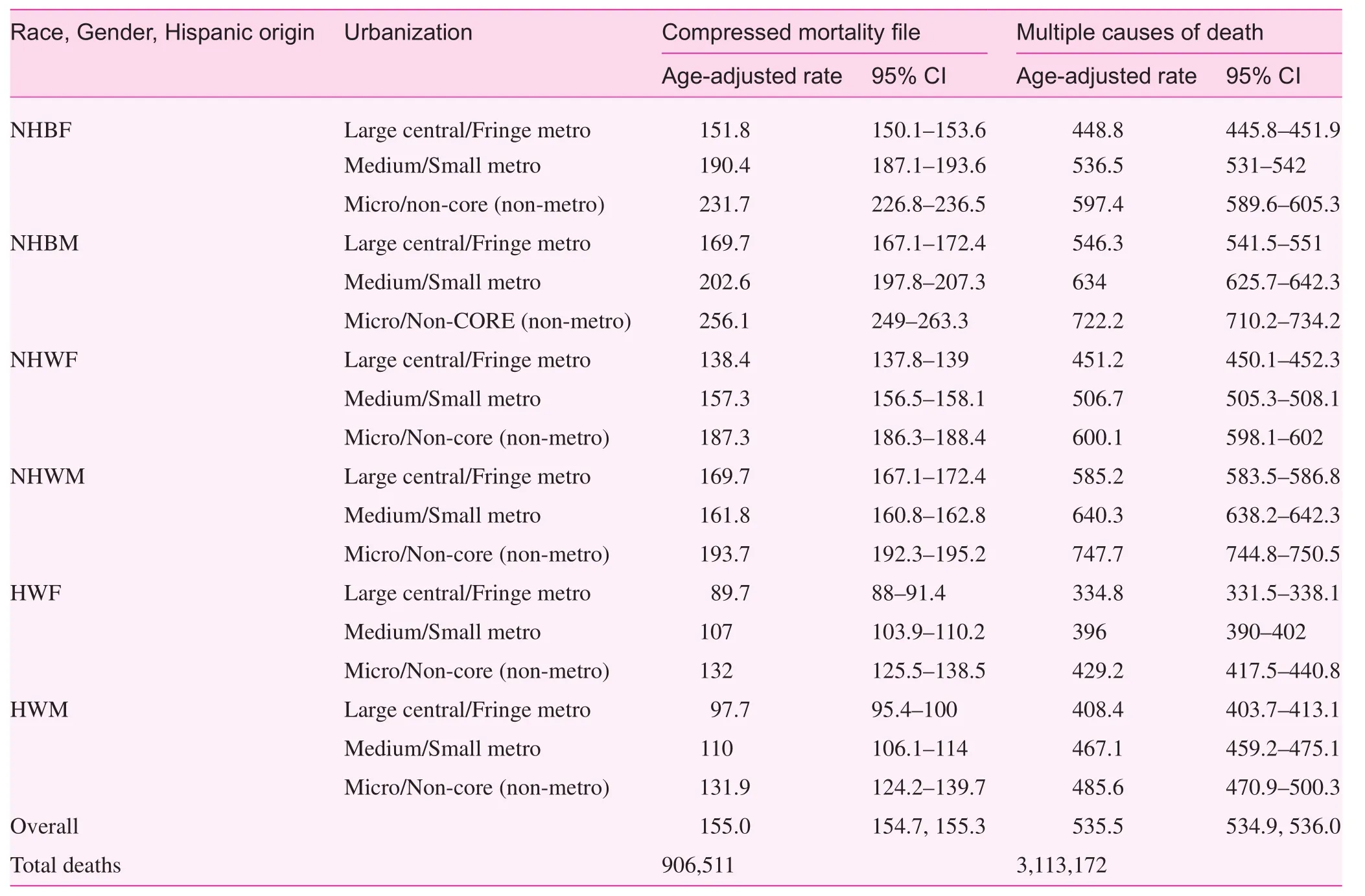
Table 1. Differences in congestive heart failure reported mortality rates between compressed mortality and multiple causes of death files among persons ≥65 years of age according to race, gender, Hispanic origin, and urbanization, US, 1999–2013
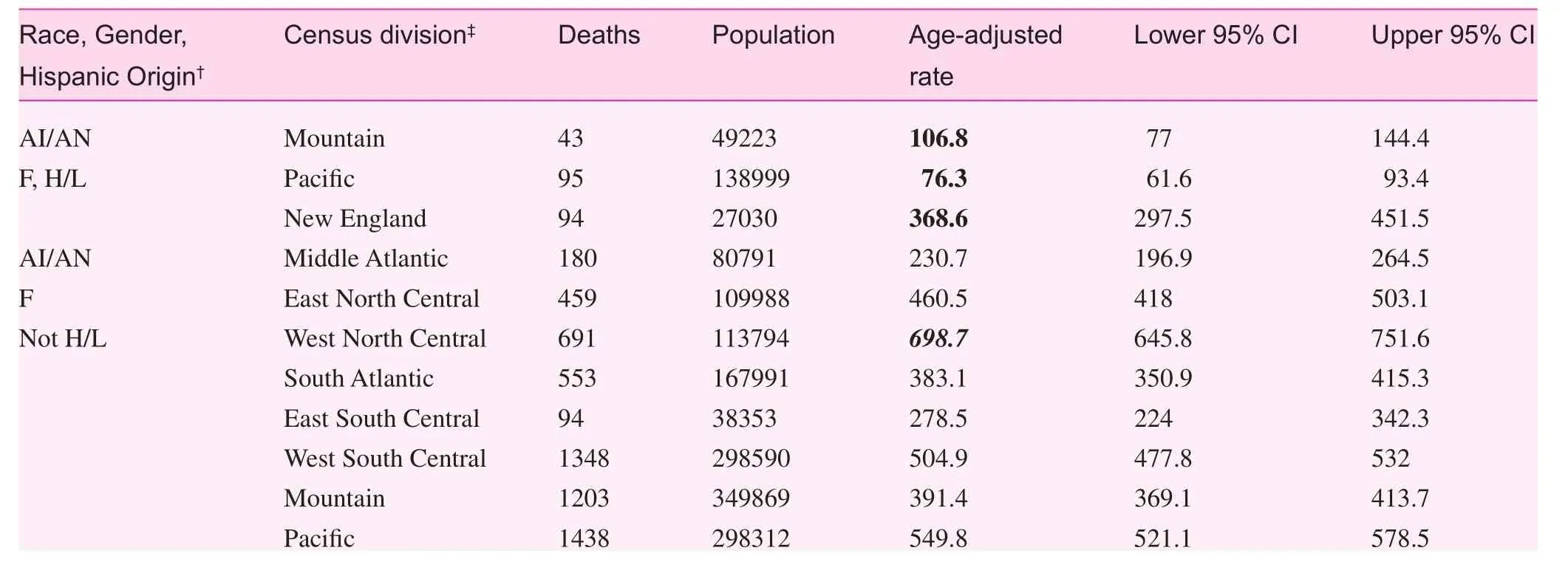
Table 2. Congestive heart failure mortality among persons 65+ years of age according to race, gender, Hispanic origin, and US Census Division,* US, 1999–2013
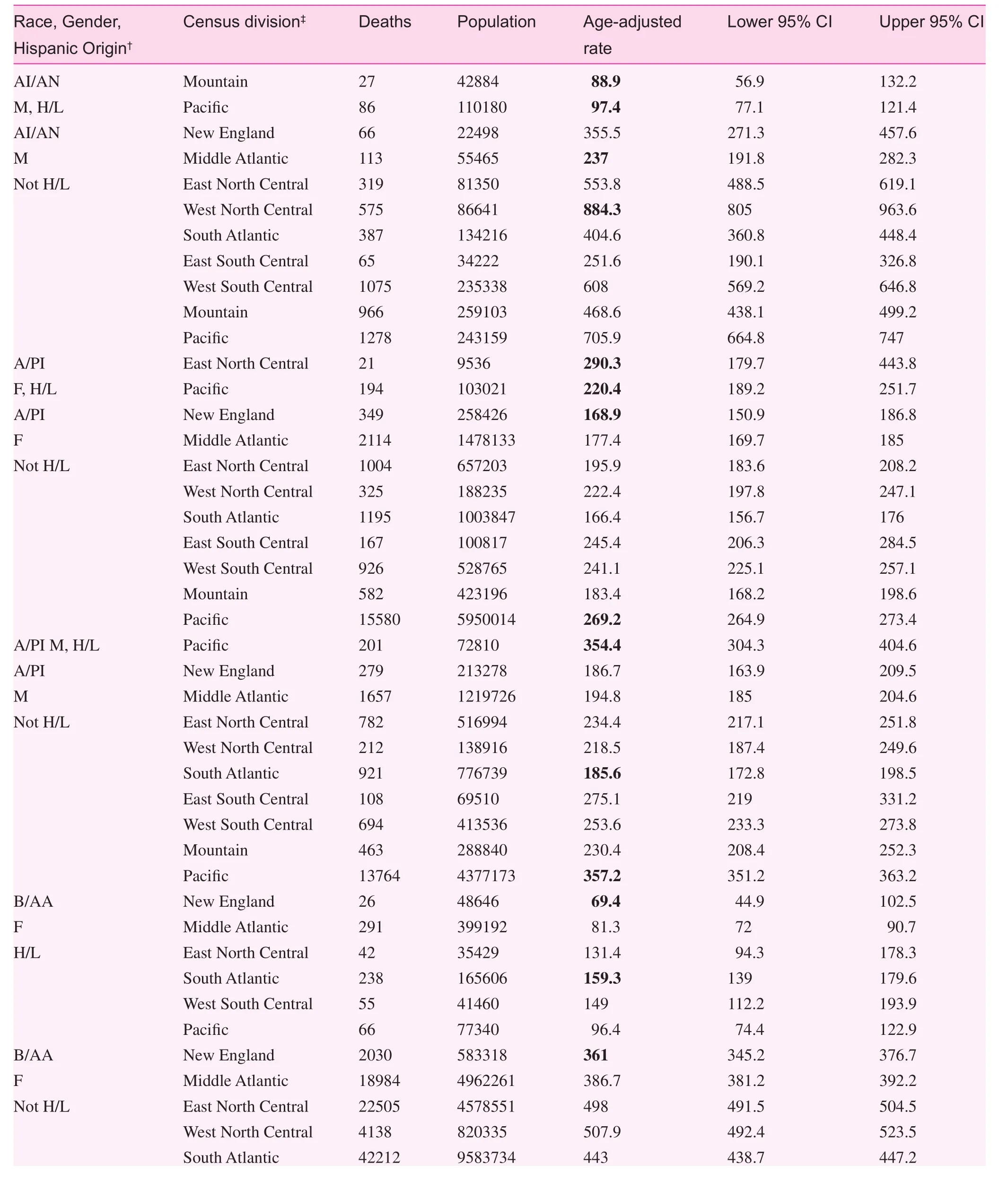
Table 2. (continued)
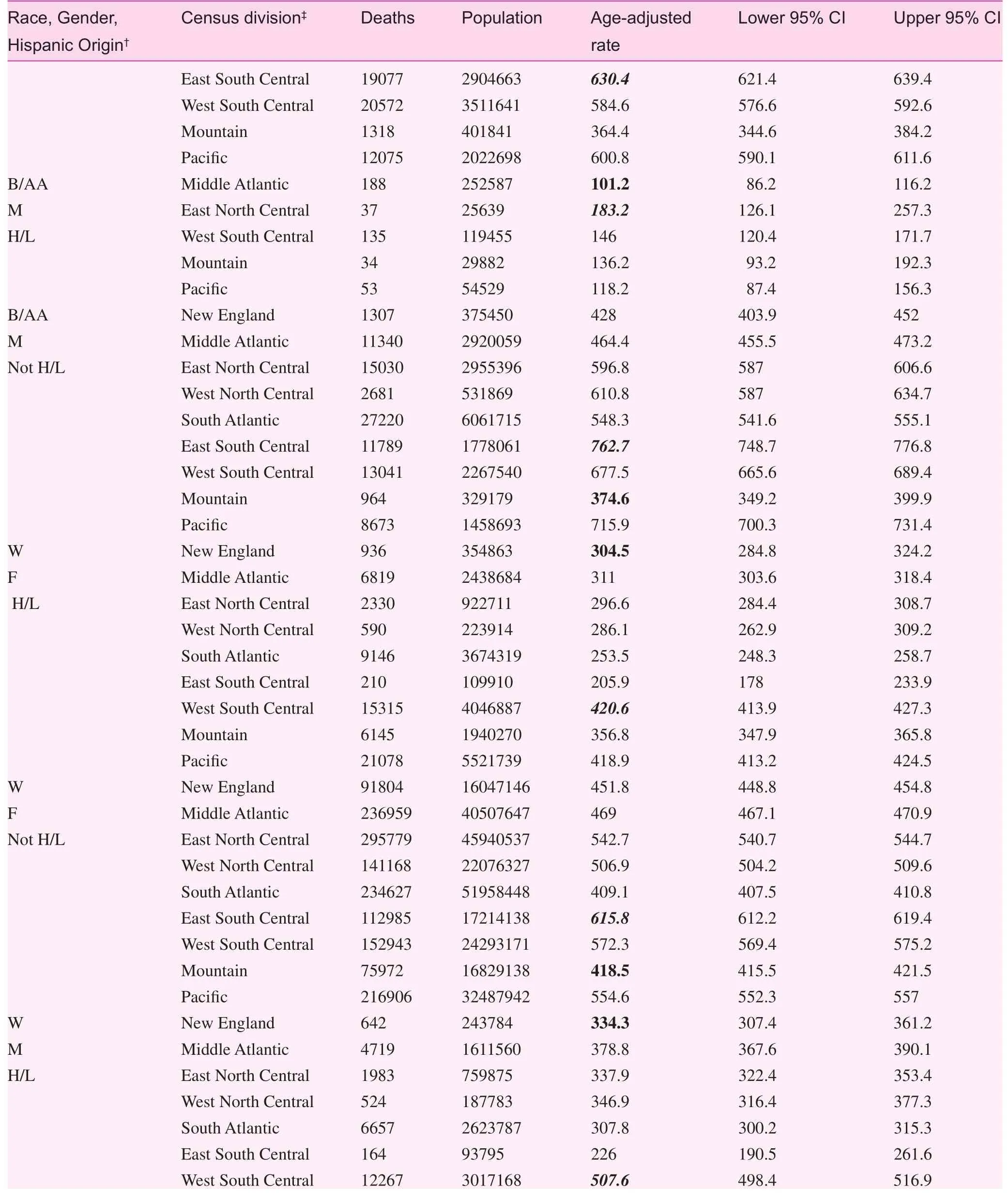
Table 2. (continued)

Table 2. (continued)
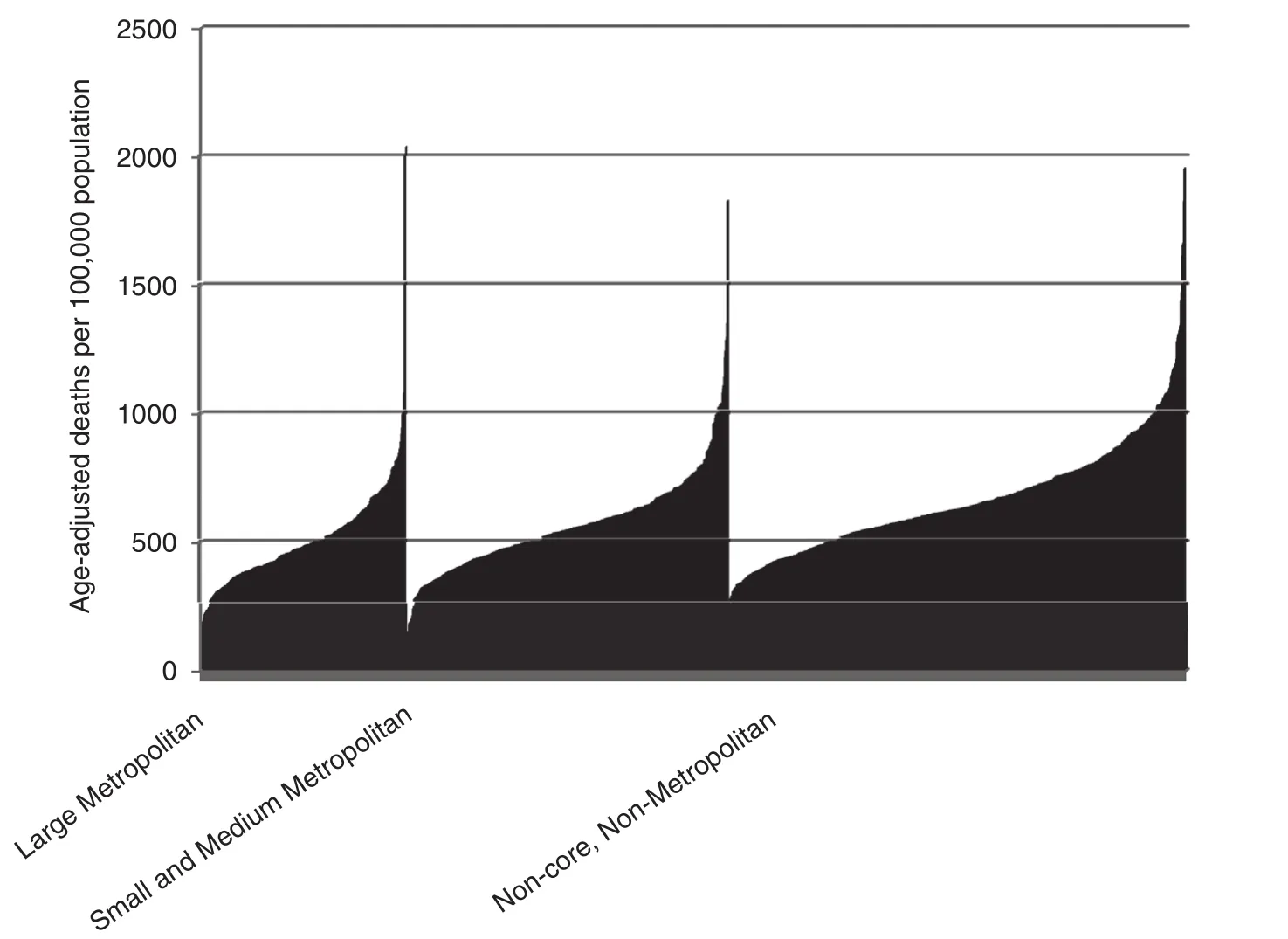
Fig. 3. Occurrence of congestive heart failure at death. Non-Hispanic white rates (age-adjusted, 65–85+ years) 1911 counties, US, 2013.
Fig. 4. Overall congestive heart failure as a contributory cause of death among US elderly (65+ years). Large metro, (n=349) medium/small metro (n=552), non-metro (n=781), and lowest micropolitan and non-core, non-metro (n=20) counties, 1999–2013.
Discussion
Within the generally high-risk population residing in micropolitan and non-core, non-metro (rural) US counties, these data identified a small subset of counties in which the risk was significantly lower than the lowest risk group based on urbanization (i.e., LCLFM counties). Moreover, this subset of rural counties experienced a decline in the overall occurrence of CHF of 47% between 1999 and 2013. We have previously shown that reductions in US mortality of 50% and higher from a variety of causes during the second half of the twentieth century are likely associated with simultaneous,if not necessarily integrated successes in scientific research,clinical implementation, and public health [13]. Because the present potentially successful positive deviant group reached a 47% mortality reduction in only 15 years, we believe that these descriptive data are consistent with the hypothesis that comparable concurrent successes may also be operative in these relatively low-risk rural counties. Moreover, because the aforementioned successes took place even as potentially negative factors, such as income inequality increased [18], there is reason to hypothesize further that the causes of community success with CHF may not necessarily be the simple opposite of adverse community progress. Analytic epidemiologic research designed a priori to test these hypotheses and link the outcomes to specific policies might provide important insight for policy makers.
Studies of rural successes in CHF are sparse. Nonetheless,Wu et al. [19] noted longer adverse event-free survival for CHF in some rural settings. The reasons for the protective effect were unclear. Another investigation showed that hospitals in urban areas had similar mortality rates for CHF admissions when compared with hospitals in more geographically remote areas. specifically, risk-standardized mortality rates for heart failure hospital admissions were not significantly different in urban areas than large rural areas (p=0.92), small rural areas(p=0.84), or remote small rural areas (p=0.42). The investigators suggested that this could reflect a better capacity to provide care for conditions not requiring intensive management in rural areas. Further, the authors speculated that this may reflect equal or better capability for providing care in rural areas for conditions that do not require intensive management,possibly because patients’ personal primary care physicians may be more likely to provide in-patient care, where their familiarity with medical history could shorten time to diagnosis, treatment, and discharge [20]. The comparability of such results, which conflict with the present data, is unclear, in part because the present results are population-based.
Although highlighting potential rural successes, the overall results in these data con firm previous reports reflecting rural disadvantages in CHF outcomes [5, 7–9]. In part, this may reflect limited access to resource-intensive programs found in major urban medical centers [21]. Lower densities of cardiology specialists may also be a factor because nearly 50% of cardiologists are concentrated in regions that have only 25%of the Medicare population, and approximately 60% of this population has access to approximately 38% of cardiologists[22]. Finally, poorer quality health care in rural safety net hospitals may also play a role [23].
Our findings are consistent with previous reports that blacks are at a significantly higher risk of death from CHF [24]. Our results showed that non-Hispanic black death rates exceeded the death rates for non-Hispanic whites, although the rates for Hispanics were lower than the death rates for non-Hispanics with the possible exception of Hispanic Asian or Pacific Islanders residing outside LCLFM counties. The increased risk of heart failure among racial and ethnic minorities has been linked to the prevalence of comorbidities, such as hypertension and diabetes mellitus, which in combination with socio-ecologic and biobehavioral factors may largely explain disparities in heart failure outcomes [24–26]. Young black men may be at especially high risk [27]. In contrast, the observed relatively low rates of CHF mortality among most Hispanic populations in these data may support the concept of the “Hispanic paradox” [28].
Finally, the present results illustrate that reliance on data based on assignment of CHF as the underlying cause of death may lead to underestimates of how often CHF contributes to mortality. Primary care physicians and others responsible for completing death certificates as well as researchers who analyze the data need to be aware of this. For example, because CHF is regarded as a system failure derived from a more specific problem (e.g., cardiac valve dysfunction) it is currently unacceptable to designate CHF as the “underlying cause of death” on US death certificates. For researchers, MCOD data provides more valid estimates of CHF contribution to mortality.
The present data have limitations of death certificate data in general [29], and multiple causes of death data in particular[30]. In addition, there is a lack of patient level information[31]. The experience of potentially successful positive deviant counties in the present could reflect basic differences in the characteristics of people residing in the positive deviant counties rather than infrastructure or policy factors. It is also possible that there are coding differences which explain the apparent successes. Despite these limitations, however, we believe the present results are useful, particularly with respect to identifying places where barriers to successful rural outcome for CHF may have been met with greater success. Finding pathways to eliminate geo-social variations in heart failure, including urban-rural differences, may assist in efforts to eliminate racial disparities as well. Furthermore, additional research will support primary care clinicians, public health professionals, and others who are interested in developing successful interventions, prevention programs, and services specifically targeted at risk burdens in these vulnerable populations. Based on previous US experience [13], there may be reason for optimism if sustained and balanced successes in implementation science,primary care, and public health are achieved.
conflict of interest
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-pro fit sectors.
1. Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS.Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med 2009;122(5):443–53.
2. Levy WC, Mozaffarian D, Linker DT, Sutradhar SC, Anker SD,Cropp AB, et al. The Seattle Heart Failure Model: prediction of survival in heart failure. Circulation 2006;113(11):1424–33.
3. KHN Morning Brie fing [http://kaiserhealthnews.org/]. End-Of-Life Care: A Challenge In Terms Of Costs And Quality. 2013 June 4 [cited 2015 March 1]. Avaiable from: http://kaiserhealthnews.org/morning-breakout/end-of-life-care-17/
4. Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J,Bradley EH, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes 2009;2(5):407–13.
5. Chen J, Normand SL, Wang Y, Krumholz HM. National and regional trends in heart failure hospitalization and mortality rates for Medicare beneficiaries, 1998–2008. J Am Med Assoc 2011;306(15):1669–78.
6. Chun S, Tu JV, Wijeysundera HC, Austin PC, Wang X,Levy D, et al. Lifetime analysis of hospitalizations and survival of patients newly admitted with heart failure. Circ Heart Fail 2012;5(4):414–21.
7. Gamble JM, Eurich DT, Ezekowitz JA, Kaul P, Quan H,McAlister FA. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ Heart Fail 2011;4(3):317–23.
8. Teng TH, Katzenellenbogen JM, Hung J, Knuiman M,San filippo FM, Geelhoed E, et al. Rural-urban differentials in 30-day and 1-year mortality following first-ever heart failure hospitalisation in Western Australia: a population-based study using data linkage. BMJ Open 2014;4(5):e004724.
9. Kociol RD, Greiner MA, Fonarow GC, Hammill BG,Heidenreich PA, Yancy CW, et al. Associations of patient demographic characteristics and regional physician density with early physician follow-up among medicare beneficiaries hospitalized with heart failure. Am J Cardiol 2011;108(7):985–91.
10. Levine RS, Briggs NC, Kilbourne BS, King WD, Fry-Johnson Y,Baltrus PT, et al. Black-White mortality from HIV in the United States before and after introduction of highly active antiretroviral therapy in 1996. Am J Public Health 2007;97(10):1884–92.
11. Fry-Johnson YW, Levine R, Rowley D, Agboto V, Rust G. United States black:white infant mortality disparities are not inevitable:identification of community resilience independent of socioeconomic status. Ethn Dis 2010;20(1 Suppl 1):S1-131-5.
12. Levine RS, Rust G, Aliyu M, Pisu M, Zoorob R, Goldzweig I,et al. United States counties with low black male mortality rates.Am J Med 2013;126(1):76–80.
13. Rust G, Satcher D, Fryer GE, Levine RS, Blumenthal DS.Triangulating on Success: Innovation, Public Health, Medical Care, and Cause-specific US Mortality Rates Over a Half Century (1950–2000). Am J Public Health 2010;100(Suppl 1):S95–104.
14. Centers for Disease Control and Prevention, National Center for Health Statistics. Multiple Cause of Death from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. [cited 2015 Mar 31]. Available from:http://wonder.cdc.gov/mcd-icd10.html
15. Tinetti ME, McAvay GJ, Murphy TE, Gross CP, Lin H,Allore HG. Contribution of individual diseases to death in older adults with multiple diseases. J Am Geriatr Soc 2012;60(8):1448–56.
16. Instructions for completing the cause-of-death section of the Death certificate. US Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics. Document 04-0377. Issued August 2004.
17. Ingram DD, Franco SJ. NCHS urban-rural Classification scheme for counties. Vital Health Stat 2012;(154):1–65.
18. Kawachi I, Kennedy BP. The Health of Nations: Why Inequality is Harmful to Your Health. New York, NY: The New Press; 2002.
19. Wu JR, Moser DK, Rayens MK, De Jong MJ, Chung ML,Riegel B, et al. Rurality and event-free survival in patients with heart failure. Heart Lung 2010;39(6):512–20.
20. Ross JS, Normand SL, Wang Y, Nallamothu BK, Lichtman JH, Krumholz HM. Hospital remoteness and thirty-day mortality from three serious conditions. Health Aff (Millwood)2008;27(6):1707–17.
21. Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health 2006;22(2):140–6.
22. Aneja S, Ross JS, Wang Y, Matsumoto M, Rodgers GP,Bernheim SM, et al. US cardiologist workforce from 1995 to 2007: modest growth, lasting geographic maldistribution especially in rural areas. Health Aff (Millwood) 2011;30(12):2301–9.
23. Joynt KE, Harris Y, Orav EJ, Jha AK. Quality of care and patient outcomes in critical access rural hospitals. J Am Med Assoc 2011;306(1):45–52.
24. Bahrami H, Kronmal R, Bluemke DA, Olson J, Shea S, Liu K,et al. Differences in the incidence of congestive heart failure by ethnicity: the multi-ethnic study of atherosclerosis. Arch Intern Med 2008;168(19):2138–45.
25. Franciosa JA, Taylor AL, Cohn JN, Yancy CW, Ziesche S,Olukotun A, et al. African-American Heart Failure Trial(A-HeFT): rationale, design, and methodology. J Card Fail 2002;8(3):128–35.
26. Taylor AL, Lindenfeld J, Ziesche S, Walsh MN, Mitchell JE,Adams K, et al., Outcomes by gender in the African-American Heart Failure Trial. J Am Coll Cardiol 2006;48(11):2263–7.
27. Husaini BA, Mensah GA, Sawyer D, Cain VA, Samad Z, Hull PC,et al. Race, sex, and age differences in heart failure-related hospitalizations in a southern state: implications for prevention.Circ Heart Fail 2011;4(2):161–9.
28. Medina-Inojosa J, Jean N, Cortes-Bergoderi M, Lopez- Jimenez F.The Hispanic paradox in cardiovascular disease and total mortality. Prog Cardiovasc Dis 2014;57(3):286–92.
29. Hennekens CH, Buring JE, Mayrent SL. Epidemiology in Medicine. Boston: Little, Brown and Co; 1987.
30. Redelings MD, Wise M, Sorvillo F. Using multiple cause-of death data to investigate associations and causality between conditions listed on the death certificate. Am J Epidemiol 2007;166(1):104–8.
31. Eberhardt MS, Pamuk ER. The importance of place of residence:Examining health in rural and nonrural areas. Am J Public Health 2004;94(10):1682–6.
1. Department of Family and Community Medicine, Baylor College of Medicine, Houston,TX, USA
2. Department of Sociology,Tennessee State University,Nashville, Tennessee, USA
3. Center for Prevention Research, Tennessee State University College of Agriculture,Nashville, Tennessee, USA
4. Department of Political Science, Texas Tech University,Lubbock, TX, USA
5. Department of Electrical Engineering and Computer Science, University of Tennessee,Knoxville, Tennessee, USA
6. Department of Family Medicine, National Center for Primary Care, Morehouse School of Medicine, Atlanta, Georgia,USA
Maria C. Mejia de Grubb, MD,MPH
Department of Family and Community Medicine
3701 Kirby Drive, Suite 600
Houston, TX 77098, USA
Tel.: +713-798-4735
E-mail: Maria.MejiadeGrubb@bcm.edu
8 April 2015;
24 April 2015
 Family Medicine and Community Health2015年2期
Family Medicine and Community Health2015年2期
- Family Medicine and Community Health的其它文章
- Evaluation of obstetrics procedure competency of family medicine residents
- Student self-assessment of strengths and needed improvements during a family medicine clerkship
- Depression and race affect hospitalization costs of heart failure patients
- Exploring point-of-care transformation in diabetic care: A quality improvement approach
- Hospitalizations and healthcare costs associated with serious,non-lethal firearm-related violence and injuries in the United States,1998–2011
- Adult immunization improvement in an underserved family medicine practice
