Exploring point-of-care transformation in diabetic care: A quality improvement approach
Malvika Juneja, Maria C. Mejia de Grubb, Haijun Wang, Kiara Spooner, Roger J. Zoorob
Exploring point-of-care transformation in diabetic care: A quality improvement approach
Malvika Juneja, Maria C. Mejia de Grubb, Haijun Wang, Kiara Spooner, Roger J. Zoorob
Objective:This quality improvement project evaluated the impact of a point-of-care (POC)HbA1c stat lab intervention and a nurse-assisted expanded visit implemented among patients with uncontrolled type 2 diabetes (T2D) at a community health center in Houston, TX.
Methods:This was a before-and-after POC intervention among adult patients who received primary care services between 1 July 2014 and 31 December 2014 (baseline visit) and who had at least one 3-month follow-up visit.
Results:Three hundred eighty-seven patients were included in the study. The majority were <60 years of age (72.1%), female (60.5%), and Hispanic (63%), followed by black (16.5%)and Asian (11.1%). Almost 87% of the patients had uncontrolled T2D (HbA1c >9%) at baseline,with the highest average levels among Hispanic (10.9%) and black (10.7%) patients. There was a significant difference in the HbA1c level before (mean=10.65, SD=1.9291) and after(mean=9.25, SD=1.8187) intervention. The absolute reduction in the level of HbA1c was 1.4%(t=12.834, p<0.001), corresponding to a 13% overall percentage decrease from baseline.
Conclusion:There is a distinct advantage in using a stat HbA1c lab when combined with shared POC visits to assist patients with uncontrolled T2D in lowering the HbA1c, improving self-management, and reducing long-term costs.
Diabetes; point of care; stat HbA1c
Introduction
Diabetes is one of the leading causes of death and disability in the United States (US) and a major contributor to the alarming rise in per capita expenditures for health care [1, 2].Although diabetes control has been improving in recent years, optimal control of the three main diabetes care measures (hemoglobin A1c[HbA1c], blood pressure, and low-density lipoprotein-cholesterol) remains very low (12.2%)[3, 4]. Hence, there has been a paradigm shift in the management of diabetes [5] towards inclusion of point-of-care (POC) services as an essential component of primary care.In primary care settings, POC HbA1c testing may assist in making informed clinical decisions, optimizing treatment, and improving glycemic control [6–8].
Texas (TX) has one of the largest adult populations living with diabetes (9.7%),accounting for over $29 billion in total costs [2, 9]. To address the increasing prevalence and accompanying costs, federal and state efforts continue to be madethrough increased patient education opportunities, health care policy changes, and promotion of screening guidelines to health professionals especially in the primary care setting where majority of diabetics have type 2 diabetes (T2D) [8, 10, 11].
Local problem: Harris Health is a community-owned health care system for the nation’s third most populous county (Harris County, TX) [12] which serves an indigent population considered to be at high risk for uncontrolled diabetes (Fig. 1) [13]. In January 2014, a quality improvement (QI) program was implemented to optimize resource use aligned with the principles of Patient-Centered Medical Home (PCMH) and Integrated Care in Diabetes Management. Within this framework, the POC HbA1c lab was offered to maximize benefit to patients in addition to a nurse educator and a team assessment performed comprehensively at the time of the visit. The aim of this QI program was to assess the impact of a POC HbA1c stat lab intervention and a nurse-assisted expanded visit implemented among patients with uncontrolled diabetes (HbA1c >9) at a community health center in Houston, TX.
The primary improvement-related question that the study of the intervention was designed to answer was as follows: In a primary care setting, will a POC-expanded visit program show a reduction in the percentage of patients with uncontrolled diabetes? The secondary questions answered through this QI program included the following: (1) Will the implementation of this program reduce the need for ED visits and hospitalizations caused by complications among participants? And (2)Will the use of the screening algorithm affect cycle time and enhance the role of nurses in chronic disease management?
Methods
Study design and population
The study design was a before-and-after POC-expanded visit intervention of a practice-based QI project using an algorithm for optimal use of POC stat HbA1c testing under a standing order protocol that offered results to the provider at the time of the patient visit. The study population included adult patients(≥18 years of age) seen at an urban community health center(CHC) in Harris County, Houston, TX.
Figure 2 shows the algorithm designed for optimum use of the stat HbA1c lab in the clinic. Alignment of everyday schedules mandated for all physicians and nurses such that each patient’s last HbA1c was visible on the electronic medical record (EMR) master schedule. Those patients who lacked a HbA1c result in the last 1 to 2 years were screened with a 3-point questionnaire. If positive, a routine HbA1c was suggested to the physician through a “Screen for Diabetes” prompt,and nutrition and lifestyle handouts were given to enhance patient awareness. Patients with a HbA1c >9% were sent for an updated lab at check-in, followed by a nurse intervention, assessment, education goal setting, and referrals pended before the patient saw the physician. Stat Lab turnover within 15–20 min was ensured by the pathology staff. The physician used the lab for medication titration and the nurse evaluation for disease management. Nurses charged “Education” time in the encounter, then documented the goal in the after-visit summary to allow tracking of POC participants and to refer back to their management at the time of the next visit. Participating providers (n=14) and nurses (n=24) received an in-service education on the importance of glycemic control, evidenced-based guidelines on optimal HbA1c values, and what constituted the POC program.
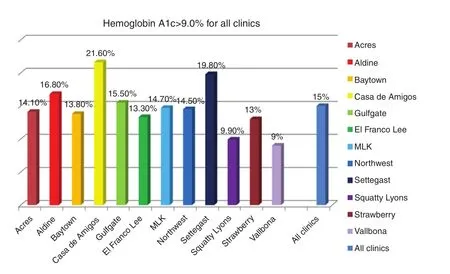
Fig. 1. Percentage of patients with uncontrolled diabetes by clinic in the Harris Health Healthcare System, Harris County, TX, 2014.
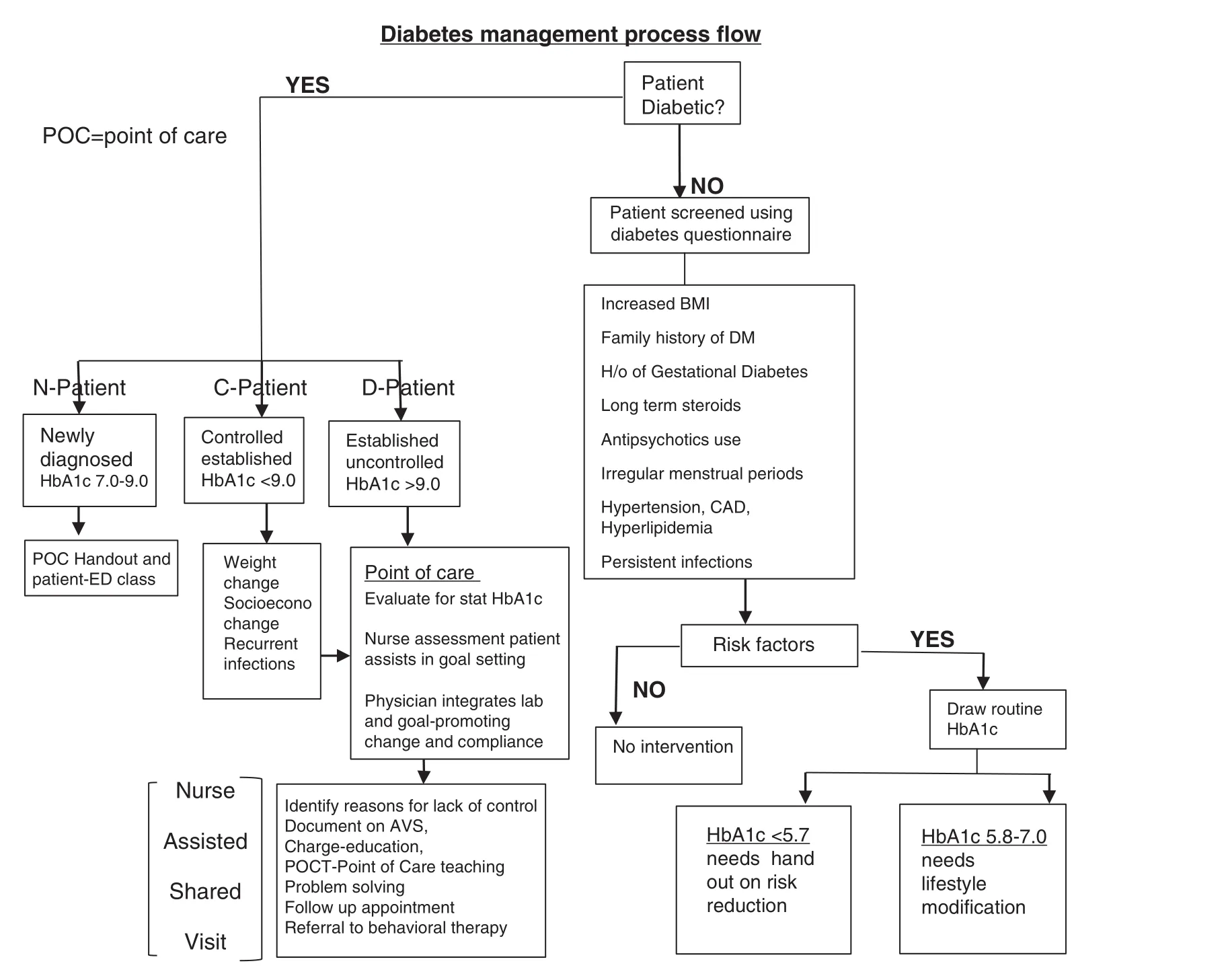
Fig. 2. Algorithm for optimal use of the point-of-care HbA1c (stat laboratory test) in the Community Health Center (CHC) in Houston, TX.
The study sample comprised approximately 500 patients attending the primary care clinic who participated in the POC QI program between 1 July 2014 and 31 December 2014 (baseline visit) and who had at least one visit 3 months after the first visit (follow-up visit). After accounting for missing data pertinent to the study and removing duplicates, 387 unique participants were included in the analysis. The study was approved by the Institutional Review Board of Baylor College of Medicine.
Methods of evaluation
The primary measures included documented HbA1c values at the time of the initial visit and a post-intervention HbA1c value documented at a follow-up visit approximately 3 months after the POC services were rendered. POC stat HbA1c levels were measured in venous samples using the A finion AS100 Analyzer System (Axis-Shield Diagnostics Ltd., Scotland),which has shown good correlation with the standard laboratory method and acceptable precision [14]. Other measures included patient demographic information (age, gender, and race/ethnicity) and number of emergency room visits pre- and post-POC service. All personal human information identifiers were removed before data analysis.
Descriptive statistics were performed and a paired t test was used to compare means and evaluate the change between HbA1c levels, and pre- and post-intervention periods. Pearson chi-square test was used to assess if there was a relationship between independent variables. The null hypothesis was rejected for a p<0.05 for all comparisons. All statistical analyses were performed using SPSS (version 22).
A brief survey assessing nurse satisfaction with the POC program implementation at the end of the study period was used to assess the nurses’ perceptions of their role in chronic disease management. The impact of the algorithm on cycle time was also assessed by tracking provider encounters.
Results
Three hundred eighty-seven adult patients met our inclusion criteria; specifically, the patients had a baseline visit and a three-month visit during the post-intervention period(Table 1). Patients were generally <60 years of age (72.1%),60.5% were women, and 63% were Hispanic (16.5% black and 11.1% Asian). Because the CHC largely serves an underserved population, it was important to account for immigration status showing that nearly one-third of patients (32.3%) were undocumented immigrants.
The proportion of patients with HbA1c levels >9% (uncontrolled diabetes) decreased from 86.8% at baseline to 49.4%at the post-intervention follow up. There were no statistically significant differences in HbA1c levels at baseline by gender,age group, or residency status; however, the baseline HbA1c was statistically significant different by race and ethnicity with higher average levels for Hispanics (10.9%), blacks (10.7%),whites (10.1%), and Asians (9.7%; p=0.001).
Table 2 shows the HbA1c levels before (at baseline,mean=10.65, SD=1.9291) and after (mean=9.25, SD=1.8187)the intervention. The absolute reduction in the level of HbA1c was 1.4% (t=12.89, p<0.000), which was equivalent to an overall percentage decrease of 13% during the post-intervention period (Table 2). With an improvement in the HbA1c level, statistically significant differences were noted by race, ethnicity,and gender. Hispanics had the highest decrease in the average HbA1c level (–1.66%), followed by blacks (–1.38%), Asians(–0.66%), and whites (–0.68%). Figure 3 shows the overall decrease in HbA1c level for Hispanics (15%), blacks (13%),Asians (7%), and whites (7%). Male patients were shown to have a greater percentage decrease in the HbA1c level (16%)compared to females (11%). No statistically significant differences were noted in HbA1c changes by age group or residency status.
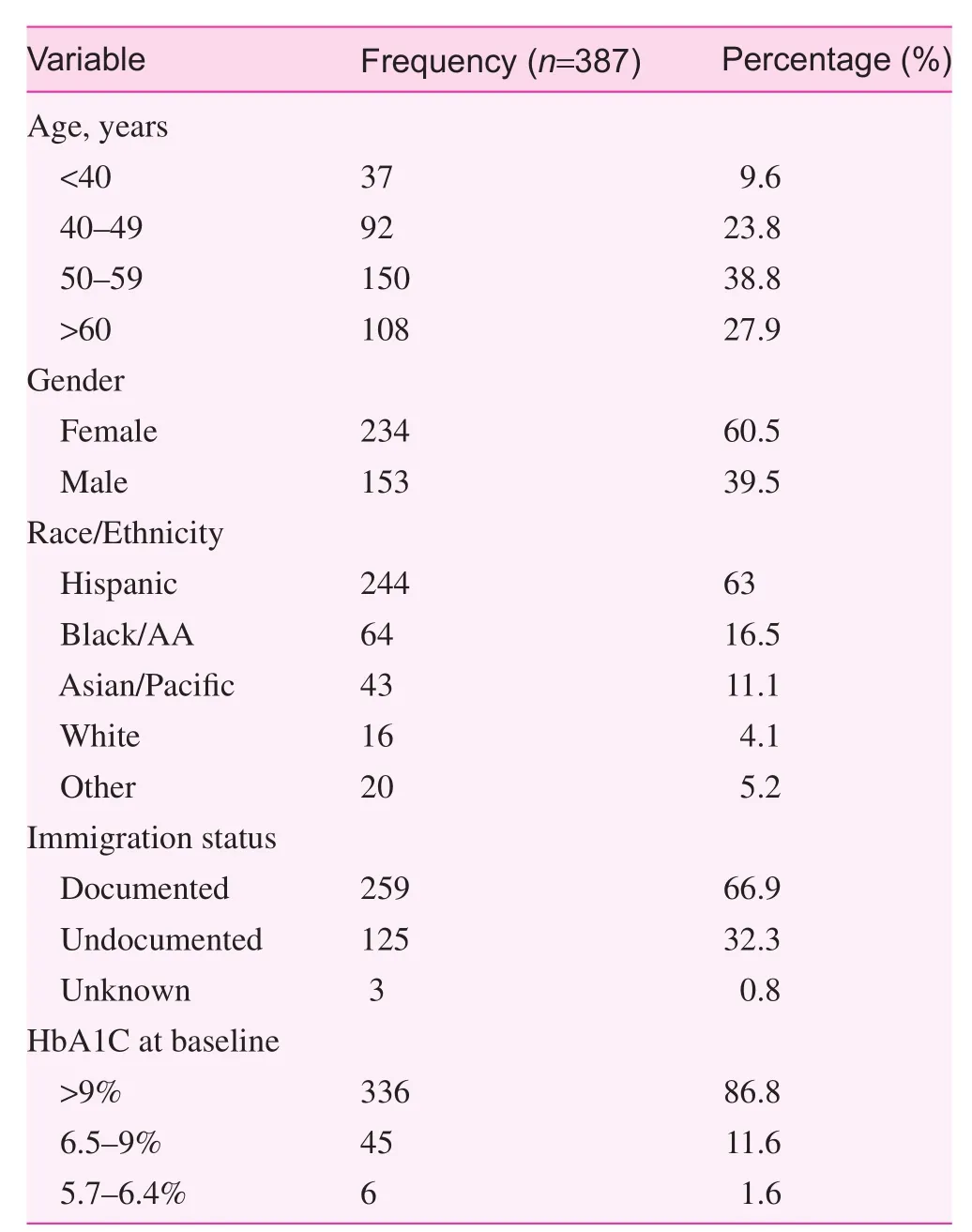
Table 1. Characteristics of study sample
We reviewed preventable diabetes-related urgent care/emergency room (ER) visits 6 months prior and 6 months postbaseline POC visit to assess the impact of the program on ER use. Two hundred forty of 387 patients in the study sample with complete ER visits records were included in the analysis. Sixty-eight percent (n=164) of the patients did not have any pre- or post-ER visits during the study period, although the HbA1c level decreased by 13% (pre-ER=10.47% vs. post-ER=9.12%). Among 57 patients with ≥1 pre-intervention ERvisits, but no post-intervention ER visits, the average number of ER visits decreased by 34% (pre-ER=1.6 vs. post-ER=1.05)and the HbA1c decreased by 16% (pre-ER=11.05 vs. post-ER=9.25%) during the post-intervention period. Nineteen patients with no ER visits at the time of intervention and >1 post-intervention ER visits exhibited a change from a 0 to an average of 1.3 visits in addition to a HbA1c drop of 14% (pre-ER=10.76 vs. post-ER=9.26).
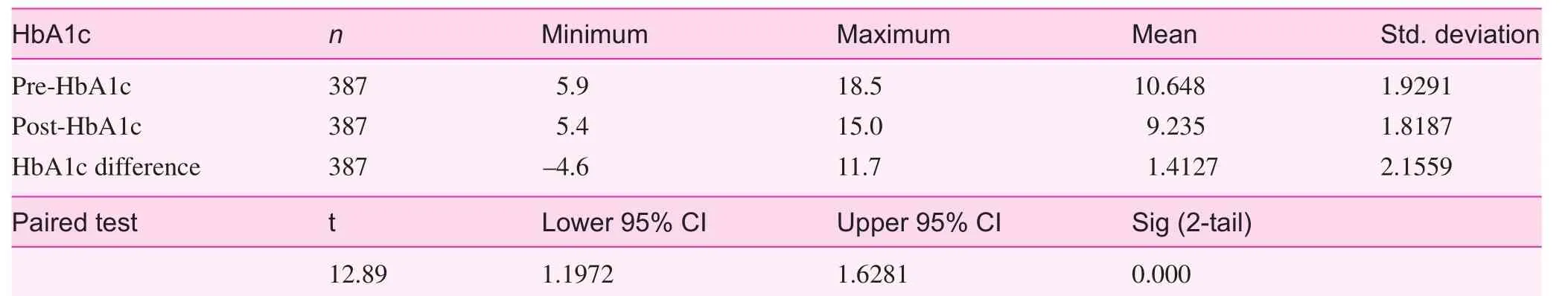
Table 2. Pre- and post-POC HbA1c
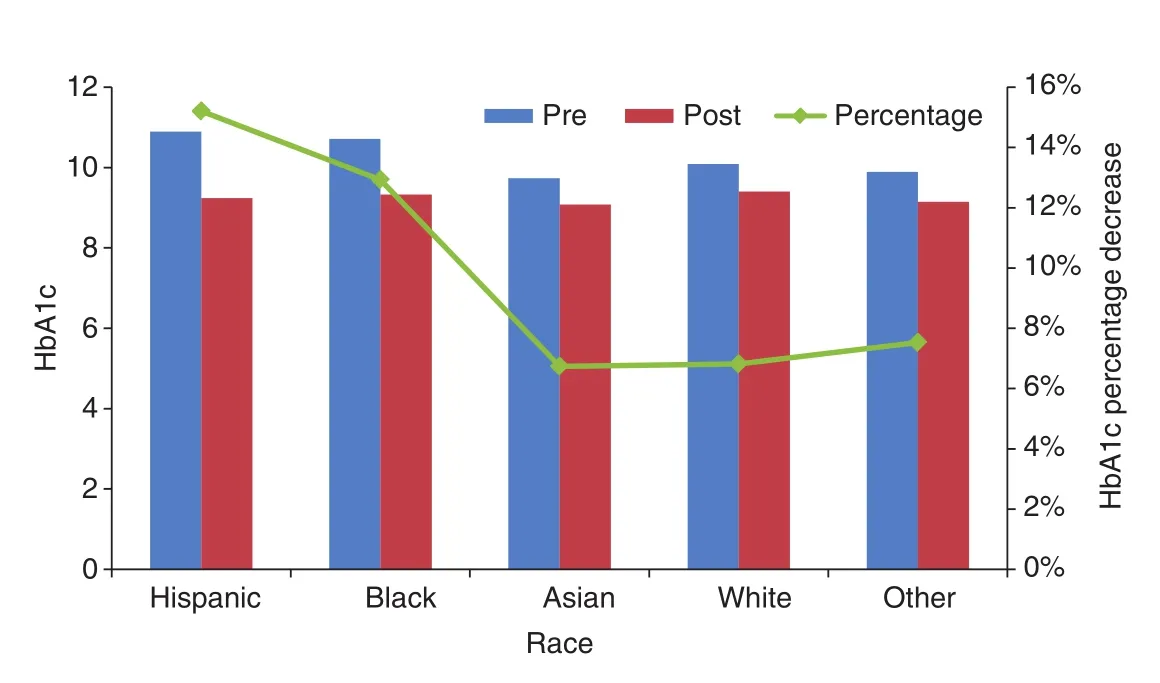
Fig. 3. HbA1c level before and after POC intervention and percentage of decrease by race and ethnicity.
The survey administered among nurses revealed an 87%willingness to participate in the POC program. Although 93%of the nurses felt that the POC approach helped to improve diabetes screening and control, only 66% felt that the nurse(RN) assessment and teaching component added any bene fit to patients with uncontrolled diabetes.
Discussion
We report a 13% improvement in glycemic control after implementation of a POC extended visit program among a group of patients with generally uncontrolled type 2 diabetes (nearly 87%) in a community health primary care setting. This POC model included POC HbA1c testing and nurse evaluation/education components. We used stat HbA1c as a new evaluation tool to accurately identify patients with uncontrolled diabetes and improve disease management. Previous studies support POC HbA1c as a useful of fice-based practice to assist providers in improving diabetes management among this patient population [15–17]. POC HbA1c testing could help titrate medications appropriately without the risk of hypoglycemia,and reduce frustration with missed laboratory appointments and missed recalls that follow regular next day results. With increased glycemic control, the risks and progression of diabetes-related complications may be reduced [6–8, 18, 19].
In traditional office visits, providers face challenges with non-adherence to medications, missed office and laboratory appointments, patient hesitation for multiple co-pays, and difficult reversal of uncontrolled diabetes [20, 21]. Expanded patient visits, including POC services, are therefore seen as an improved platform of delivery of care for such patient encounters [22, 23]. Indeed, the American Diabetes Association recommends POC HbA1c testing as it provides an opportunity for more appropriate patient management [8]. Although stat HbA1c lab results have aided clinical decisions in the emergency room,HbA1c lab use in ambulatory diabetes management is not well established because of cost concerns [24, 25]. Optimal resource use could thus require use restricted for patients with uncontrolled diabetes and would depend on the value society would place on maintaining a patient within the therapeutic range[26]. In our study, we found an approximate 34% reduction of preventable diabetes-related ER visits which could entail a long-term patient care savings that should be taken into consideration for budget purposes [27]. In fact, a recent analysis of HbA1c measurement to monitor glycemic control in patients with diabetes in Ontario showed that POC could have saved the province $1,175,620 to $4,702,481 in 2013/2014 [28].
Harris Health, a community-owned health system affiliated with Baylor College of Medicine, serves indigent patients;the HbA1c level is >9% in approximately 14% of patients.Consequently, there was a need to revisit the diabetes care delivery system in terms of increasing efficacy of each visit by creating an algorithm for POC care. The primary goal of our algorithm was to optimally use and cost-contain the new HbA1c stat test. The secondary goal was to trigger a standardized screening protocol for every patient seen in the clinic as part of a PCMH model. The most important bene fit was to select high-risk patients with a HbA1c >9% for a standardized intervention and expand the visit for more comprehensive care.
Each of fice visit is a valuable POC for patients with uncontrolled diabetes and it can be used for assessment, education,and collaborative goal setting by the nurse provider-patient team without impacting cycle time (total time from the beginning to the end of the clinical encounter) or rearranging schedules. Within this framework of POC delivery of diabetic care,there is coupling of a stat HbA1c lab with nurse-assisted education and assessment. Although the majority of nurses participating in our program evaluation felt that the POC approach could help to improve diabetes screening and control, only two-thirds of nurses felt that nurse-led teaching added any bene fit to self-management of uncontrolled diabetes. Similar findings were reported by health care providers in a multinational study who agreed that diabetes self-management is suboptimal and needs improvement [29]; however, perceptions of how to encourage self-management might differ between providers and patients with diabetes, thus requiring further attention to psychological and social factors.
Therefore, the present study showed that incorporating POC HbA1c testing in diabetic care could improve glycemic control by providing rapid, accurate, and reliable results. We found little or no impact of this intervention on cycle time, yet noticed increased patient satisfaction and a statistically signifi-cant drop in HbA1c levels. Because optimum care of diabetic patients is dependent on the interaction of the health care providers and the patient, POC HbA1c results and POC educational services enhance this interaction by allowing immediate face-to-face counseling of patients.
There were some limitations with this study, including potential variations in the adherence to the algorithm given differences in provider practices and adoption of a new integrated model of care. Although QI projects are not designed to develop generalizable knowledge or to test a hypothesis for causality, this was a single group pre-post comparison pilot project in a single institution that did not include a control group, which limited its generalizability. This POC extended visit project, however, presents useful and important patient and provider data regarding the implementation of the program for clinical, practical, or administrative purposes. Encouraging results support the need for a larger scale multi-practice experience.
Acknowledgements
The authors would like to thank Nicol J. Ruiz and Shivanki Juneja for their efforts with data collection for this project.
conflict of interest
The authors declare no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-pro fit sectors.
1. Yang W, Dall TM, Halder P, Gallo P, Kowal SL, Hogan PF.Economic costs of diabetes in the US in 2012. Diabetes Care 2013;36(4):1033–46.
2. Centers for Disease Control and Prevention, National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014. Atlanta, GA: US Department of Health and Human Services, 2014.
3. Fitch K, Pyenson BS, Iwasaki K. Medical claim cost impact of improved diabetes control for medicare and commercially insured patients with type 2 diabetes. J Manag Care Pharm 2013;19(8):609–20, 620a–620d.
4. Cheung BM, Ong KL, Cherny SS, Sham PC, Tso AW, Lam KS.Diabetes prevalence and therapeutic target achievement in the United States, 1999 to 2006. Am J Med 2009;122(5):443–53.
5. Renders CM, Valk GD, Grif fin SJ, Wagner EH, Eijk Van JT,Assendelft WJ. Interventions to improve the management of diabetes in primary care, outpatient, and community settings: a systematic review. Diabetes Care 2001;24(10):1821–33.
6. Petersen JR, Finley JB, Okorodudu AO, Mohammad AA,Grady JJ, Bajaj M. Effect of point-of-care on maintenance of glycemic control as measured by A1C. Diabetes Care 2007;30(3):713–5.
7. Egbunike V, Gerard S. The impact of point-of-care A1C testing on provider compliance and A1C levels in a primary setting.Diabetes Educ 2013;39(1):66–73.
8. American Diabetes Association. Standards of medical care in diabetes–2014. Diabetes Care 2014;37(Suppl 1):S14–80.
9. Texas Department of State Health Services, The Burden of Diabetes In Texas, E. Of fice of Surveillance, and Research Health Promotion and Chronic Disease Prevention Section., Editor.2013: Austin, TX.
10. Texas Diabetes Council, Changing the course: A plan to prevent and control diabetes in Texas, T.D.o.S.H. Services., Editor. 2011:Austin, TX.
11. Texas Diabetes Council, Statewide Assessment of Existing Programs for the Prevention and Treatment of Diabetes, T.D.o.S.H.Services, Editor. 2014: Austin, TX.
12. Harris Health System. Access Care [March 17, 2015]; Available from: www.harrishealth.org/en/patients/access-care/pages/default.aspx.
13. Harris County Healthcare Alliance. The State of Health in Houston/Harris County 2015-2016 [March 17, 2015]; Available from: http://houstonstateofhealth.org/soh_doc/.
14. Sánchez-Mora C, S Rodríguez-Oliva M, Fernández- Riejos P,Mateo J, Polo-Padillo J, Goberna R, et al. Evaluation of two HbA1c point-of-care analyzers. Clin Chem Lab Med 2011;49(4):653–7.
15. Health Quality Ontario. Community-based care for the management of type 2 diabetes: an evidence-based analysis. Ont Health Technol Assess Ser 2009;9(23):1–40.
16. Antoline C, Kramer A, Roth M. Implementation and methodology of a multidisciplinary disease-state-management program for comprehensive diabetes care. Perm J 2011;15(1):43–8.
17. Maislos M, Weisman D. Multidisciplinary approach to patients with poorly controlled type 2 diabetes mellitus: a prospective,randomized study. Acta Diabetol 2004;41(2):44–8.
18. Delamater AM. Clinical use of hemoglobin A1c to improve diabetes management. Clinical Diabetes 2006;24(1):6–8.
19. Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care 2005;28(4):816–22.
20. Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care 2004;13(Suppl 1):i85–90.
21. Parchman ML, Romero RL, Pugh JA. Encounters by patients with type 2 diabetes–complex and demanding: an observational study. Ann Fam Med 2006;4(1):40–5.
22. American Diabetes Association. (1) Strategies for improving care. Diabetes Care 2015;38(Suppl):S5–7.
23. Weiner BJ, Helfrich CD, Savitz LA, Swiger KD. Adoption and implementation of strategies for diabetes management in primary care practices. Am J Prev Med 2007;33(1 Suppl):S35–44; quiz S45–9.
24. Brown JB, Harris SB, Webster-Bogaert S, Porter S. Point-of-care testing in diabetes management: what role does it play? Diabetes Spectrum 2004;17(4):244–8.
25. Sicard DA, Taylor JR. Comparison of point-of-care HbA1c test versus standardized laboratory testing. Ann Pharmacother 2005;39(6):1024–8.
26. Laurence CO, Moss JR, Briggs NE, Beilby JJ; PoCT Trial Management Group. The cost-effectiveness of point of care testing in a general practice setting: results from a randomised controlled trial. BMC Health Serv Res 2010;10:165.
27. Davidson MB, Ansari A, Karlan VJ. Effect of a nurse-directed diabetes disease management program on urgent care/ emergency room visits and hospitalizations in a minority population.Diabetes Care 2007;30(2):224–7.
28. Chadee A, Blackhouse G, Goeree R. Point-of-care hemoglobin A1c testing: a budget impact analysis. Ont Health Technol Assess Ser 2014;14(9):1–23.
29. Holt RI, Nicolucci A, Kovacs Burns K, Escalante M, Forbes A,Hermanns N, et al. Diabetes Attitudes, Wishes and Needs second study (DAWN2): cross-national comparisons on barriers and resources for optimal care–healthcare professional perspective.Diabet Med 2013;30(7):789–98.
Department of Family and Community Medicine, Baylor College of Medicine, Houston, TX, USA
S:Malvika Juneja, MD and Maria C. Mejia de Grubb, MD, MPH
Department of Family and Community Medicine, Baylor College of Medicine, 3701 Kirby Drive, Suite 600, Houston, TX 77098, USA
Tel.: +713-798-4735
E-mail: juneja@bcm.edu,
maria.mejiadegrubb@bcm.edu
14 April 2015;
4 May 2015
 Family Medicine and Community Health2015年2期
Family Medicine and Community Health2015年2期
- Family Medicine and Community Health的其它文章
- Evaluation of obstetrics procedure competency of family medicine residents
- Student self-assessment of strengths and needed improvements during a family medicine clerkship
- Depression and race affect hospitalization costs of heart failure patients
- Rural congestive heart failure mortality among US elderly,1999–2013: Identifying counties with promising outcomes and opportunities for implementation research
- Hospitalizations and healthcare costs associated with serious,non-lethal firearm-related violence and injuries in the United States,1998–2011
- Adult immunization improvement in an underserved family medicine practice
