Depression and race affect hospitalization costs of heart failure patients
Baqar A. Husaini, Robert S. Levine, Meggan L. Novotny, Van A. Cain, Uchechukwu K.A. Sampson, Majaz Moonis
Depression and race affect hospitalization costs of heart failure patients
Baqar A. Husaini1, Robert S. Levine2, Meggan L. Novotny1, Van A. Cain1, Uchechukwu K.A. Sampson3, Majaz Moonis4
Objective:Depression and anxiety are frequently observed in heart failure (HF) patients;however, the effect of such factors on hospitalization costs of HF patients, and whether such costs vary by race and gender remain poorly understood. This analysis delineated the prevalence of depression/anxiety among HF patients and estimated the effect of race and gender on hospitalization costs.
Methods:We examined the 2008 files of the Tennessee Hospital Discharge Data System(HDDS) on patients (≥20 years of age) with a primary diagnosis of HF (ICD-9 codes 402,404, and 428) along with demographic data, depression/anxiety diagnoses, hospital costs, and comorbidities. Among the HF sample (n=16,889) 53% were female and 23% were black. Race and gender differences in hospital costs were evaluated for the following three groups: (1) HF patients with depression/anxiety (HF+D); (2) HF-only patients without depression/anxiety (HFO);and (3) HF patients with other mental diagnoses (HF+M).
Results:HF was significantly (p<0.000) higher among blacks compared to whites, and higher among males than females. Nearly 25% of HF patients had depression/anxiety (more whites and females were depressed). HF patients averaged more than 3 comorbidities (blacks had a greater number of comorbidities and hospitalization cost for the year). Costs were higher among HF+Dpatients compared to HFOpatients. Among HF+Dpatients, costs were higher for black males compared with white males. These cost patterns prevailed largely because of higher comorbidities that required more re-admissions and longer hospital stays.
Conclusion:Race and depression/anxiety are associated with increased hospitalization costs of HF patients. The higher costs among blacks reflect the higher burden of comorbidities,such as hypertension and diabetes, which calls for widespread dissemination, adoption, and implementation of proven interventions for the control of these comorbidities.
Hospitalization costs; heart failure; race; gender; depression
Introduction
Prevalence of depression/anxiety in HF
Heart failure (HF) is the most common Medicare diagnosis, and consumes more Medicare treatment dollars than any other diagnosis. The incidence of HF has been reported [1] to be approximately 10 per 1000 population among those 65 years of age or older. One potential outcome of HF is depression or anxiety, which reportedly exists among20%–50% of HF patients; the variation in prevalence depends on how depression/anxiety was measured [2–11]. These estimates, which include pre-existing depression among cardiac patients [2], are similar to rates of depression among patients with coronary artery disease (CAD), but are two-to-three times the prevalence of depression in the general population[11]. Depression in HF patients adversely affects the quality of life [12–15], adds to poorer treatment outcomes [16–19],and leads to increased service use, hospital re-admissions,and higher mortality rates [20–31]. The effect of therapy for depression on HF patients remains inconclusive with respect to cardiac functioning, and therefore needs further examination [32–36]. Although depression is more often diagnosed among females and whites, co-existing anxiety is more often reported for black patients [37–40].
Effect of depression on health care costs
One study involving HF patients reported that 65% of health care costs is attributable to hospitalization [41]; however, these costs vary depending upon depression and other chronic conditions. For example, Sullivan and colleagues [27] reported that hospitalization costs of depressed HF patients were 29%higher compared to HF patients without depression. Similarly,other studies have reported between 31% and 54% higher costs for depressed HF patients compared to non-depressed HF patients [27, 29, 42, 43].
Very few studies have examined the effect of depression/anxiety on hospitalization costs by race and gender. Although the role of race in high health care costs has been demonstrated, the role of gender remains uncertain. For example,Burns and colleagues [30] reported that although female Medicare beneficiaries had a higher prevalence of depression and a higher use of outpatient services, the hospital costs attributable to depression were 47% higher among males compared to females ($15,060 vs. $10,240, p≤0.001). In another study, there were no differences in hospital costs between patients with anxiety and those with depression ($8613 vs.$8420 respectively) [31]. Because the effect of depression/anxiety on hospitalization costs of HF patients by race and gender is relatively unknown, we examined variations in such costs, as follows: (i) comparing heart failure plus depression patients (HF+D) with non-depressed patients (HFO) and HF patients with mental diagnoses other than depression/anxiety(HF+M); (ii) and examining variations in costs by race and gender in all three groups of HF patients.
Methods
Patient data
We used the 2008 Tennessee Hospital Discharge Data System(HDDS) to obtain relevant data on adult patients (>20 years of age) with a primary diagnosis of HF (ICD-9 codes 402, 404,and 428). Of 400,235 patients, 4.2% were discharged in 2008 with a primary diagnosis of HF (n=16,889). The HF sample included 53% females and 23% blacks with an average age of 72 years; the black patients tended to be younger (63 years)compared to white patients (75 years).
All diagnoses were made by attending physicians and appeared only when patients were treated for those diagnoses. Because 97% of the Tennessee population is comprised of non-Hispanic whites and blacks, our analysis was con fined to these two groups. The presence of secondary diagnoses from the HDDS files were used to define comorbidities, such as hypertension, diabetes, coronary heart disease (CHD),chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), and cardiovascular disease (CVD) events,affecting the patient. As there is a high overlap in symptoms of depression and anxiety (ranging from 48% to 91%) [44, 45],we combined the diagnoses of depression and anxiety as a single variable for our analyses [46].
Data analysis
The prevalence of HF hospitalized patients (per 100,000) was age-adjusted and indexed to the year 2000 census per methodology provided by the CDC [47] for the population at risk. We used two indices of comorbidities: (1) a simple count of all present comorbidities; and (2) the Charlson Index of Comorbidity[48], which measures the severity of the comorbidity for each patient. Comparison of HF comorbidities by race and gender were evaluated with a Pearson χ2test and a Fisher exact test.Further, we computed two types of hospital costs: (1) HF costs when a patient was discharged with a primary diagnosis of HF (HF Cost $); and (2) total hospital costs for year 2008,that is, when the same patient was re-admitted with diagnoses other than HF (Total Cost $). Finally, to determine the effect of depression/anxiety on hospital costs, we compared average race-gender costs for three HF groups: (1) HF patients with depression/anxiety (HF+D; n=4125), (2) HF patients without depression/anxiety or any mental diagnosis, that is HF-only(HFO; n=8306); and (3) HF patients with mental diagnoses other than depression/anxiety (HF+M; n=4458).
Results
Hospitalization costs of heart failure
Hospital costs invariably reflect the complexity of comorbidities, number of admissions, and length of hospitalization. We developed an index of patient comorbidities by counting the number of cardiovascular disease conditions and events (a total of 9 comorbidities) that were listed as secondary diagnoses. Table 1 (column 2) shows that the average HF cost for a patient was $36,184 annually and because these patients average approximately four complex comorbidities, the total hospital cost for the year was approximately 69% higher compared with a non-HF patient ($82,509 vs. $40,301 [columns 1 & 2], p≤0.001). The higher total hospital cost for HF patients appears to result from complexities of comorbidities as reflected by the Charlson scores (3.10 vs. 1.6, p≤0.001),which resulted in more re-admissions (2.83 vs. 1.49, p≤0.001),and longer hospitalizations (16.1 days vs. 7.4 days [columns 1 & 2], p≤0.001). These higher costs also reflect the age of HF patients; on average, HF patients tend to be older (72 vs.55 years), are more likely to have coronary heart disease(CHD; 66.5% vs. 23.2%, p≤0.001), and have higher rates of hypertension (87% vs. 52%, p≤0.001), diabetes (50% vs.23%, p≤0.001), stroke (14.3% vs. 8.5%, p≤0.001), myocardial infarctions (11.4% vs. 3.9%, p≤0.001), and chronic obstructive pulmonary disease (45.4% vs. 17.6%, Table 1 [columns 1 & 2], p≤0.001).
Effects of depression/anxiety on hospitalization costs(HF+Dvs. HF0& HF+M)
Table 1 shows that one-fourth (24.4%) of all HF patients had depression/anxiety. Interestingly, depression/anxiety was higher among white HF patients than black HF patients(27.4% vs. 14.5% [columns 3 & 4], p≤0.001), and higher among female than male HF patients (29.2% vs. 19.0% [columns 5 & 6], p≤0.001).
The effect of this variation in depression/anxiety on hospitalization costs was first examined by comparing the HF+Dgroup to those without depression/anxiety (HFO). Table 2 (columns 2 & 3) shows that HF+Dpatients had more comorbidities,such as hypertension, diabetes, coronary heart disease, atrial fibrillation, chronic kidney disease, and chronic obstructive pulmonary disease. Further, these comorbidities increased HF costs significantly for HF+Dpatients compared to HFOpatients(HF cost of $37,830 vs. 35,946, p≤0.001, and the total cost for the entire year increased by 46% [$109,390 vs. $68,503,p≤0.001]). These cost differences reflected not only the higher rate of comorbidities that HF+Dpatients had compared with HFOpatients, but also the higher rate of re-admissions (3.9 vs.2.2), and length of hospitalization (23.0 days vs. 12.3 days,p≤0.001). Similarly, cost trends emerged when HF+Dpatients were compared with HF+Mpatients ($109,390 vs. $83,733,p≤0.001 [a difference of 27%, Table 2, columns 2 & 4]).
Costs variations by race & gender in HF groups(HF+D, HFO, and HF+M)
Table 3 shows the cost variations by race and gender among HF+Dpatients. Both costs (HF costs as well as total costs) were significantly higher for black HF+Dpatients compared to white HF+Dpatients (HF costs for blacks were 31% higher [$49,038 vs. 36,040, p≤0.001] and total costs were 35% higher [$147,511 vs. $103,303, p≤0.001] {columns 1 & 2}). These higher costs appear, in part, because of a greater proportion of blacks who suffered from hypertension, diabetes, and chronic kidney disease that added to more re-admissions among blacks (4.6 vs.3.8 [columns 1 & 2], p≤0.001), and longer hospitalization than whites (29.6 days vs. 22.0 days, p≤0.001). In fact, blacks in other HF groups (HFO& HF+M) also had longer hospital stays and higher costs relative to whites (Table 3 [columns 5 & 6 and 9 &10]).
A similar effect of depression on health care costs among blacks in the HF+Dgroup also emerged for gender comparisons. Males had higher costs than females ($125,294 vs.99,903 [Table 3, cols. 3 & 4], p≤0.001). Similar cost differentials also appeared in other HF groups (columns 7 & 8 and 11 & 12). These higher costs among males (Table 3 [columns 3 & 4]) were largely caused by more comorbidities (4.5 vs.4.0, p≤0.001), more re-admissions (4.2 vs. 3.8, p≤0.001), andlonger hospital stays (24.8 days vs. 22.1 days,p≤0.001). In fact, a gender breakdown by race revealed that higher costs for males accrued for both black and white males compared to their respective female peers.
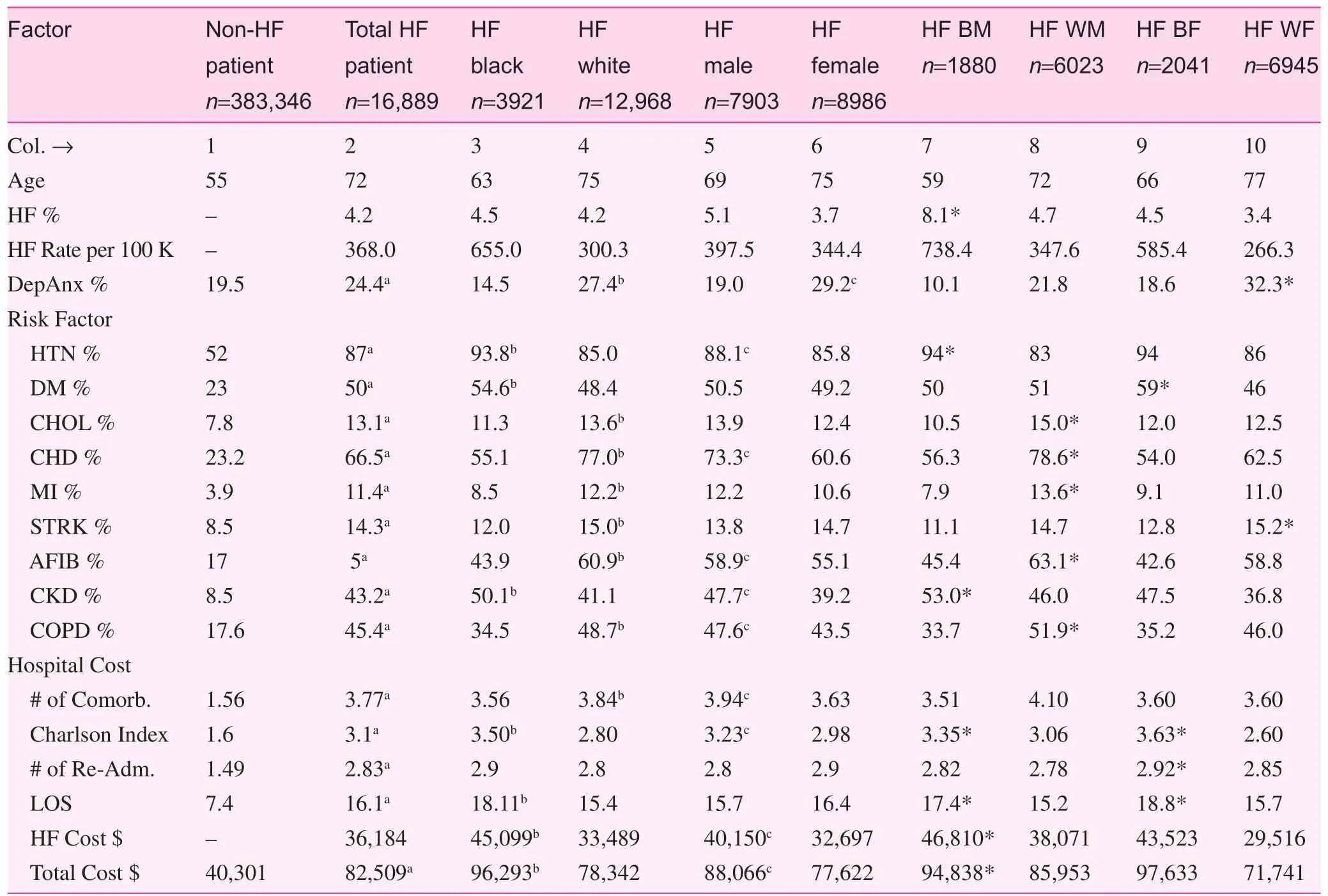
Table 1. Heart failure sample cardiovascular risk factors and annual hospitalization cost variables by race and gender
Discussion
Our study has produced some interesting findings. First,the average hospitalization cost for HF treatment alone was$36,184, and because these patients were also treated on average for more than three comorbidities, the total hospital cost for a year increased to $82,509. These higher costs occurred among blacks and males and among those HF patients who were also afflicted with depression and anxiety. The effect of depression/anxiety in increasing total hospitalization costs was nearly 46% higher for HF+Dpatients compared with HF patients who did not have such emotional afflictions. Theestimated higher costs attributable to depression/anxiety is similar to other studies that reported increased costs ranging from 29% to 54% because of depression/anxiety among HF patients [27, 29, 30, 42, 43].
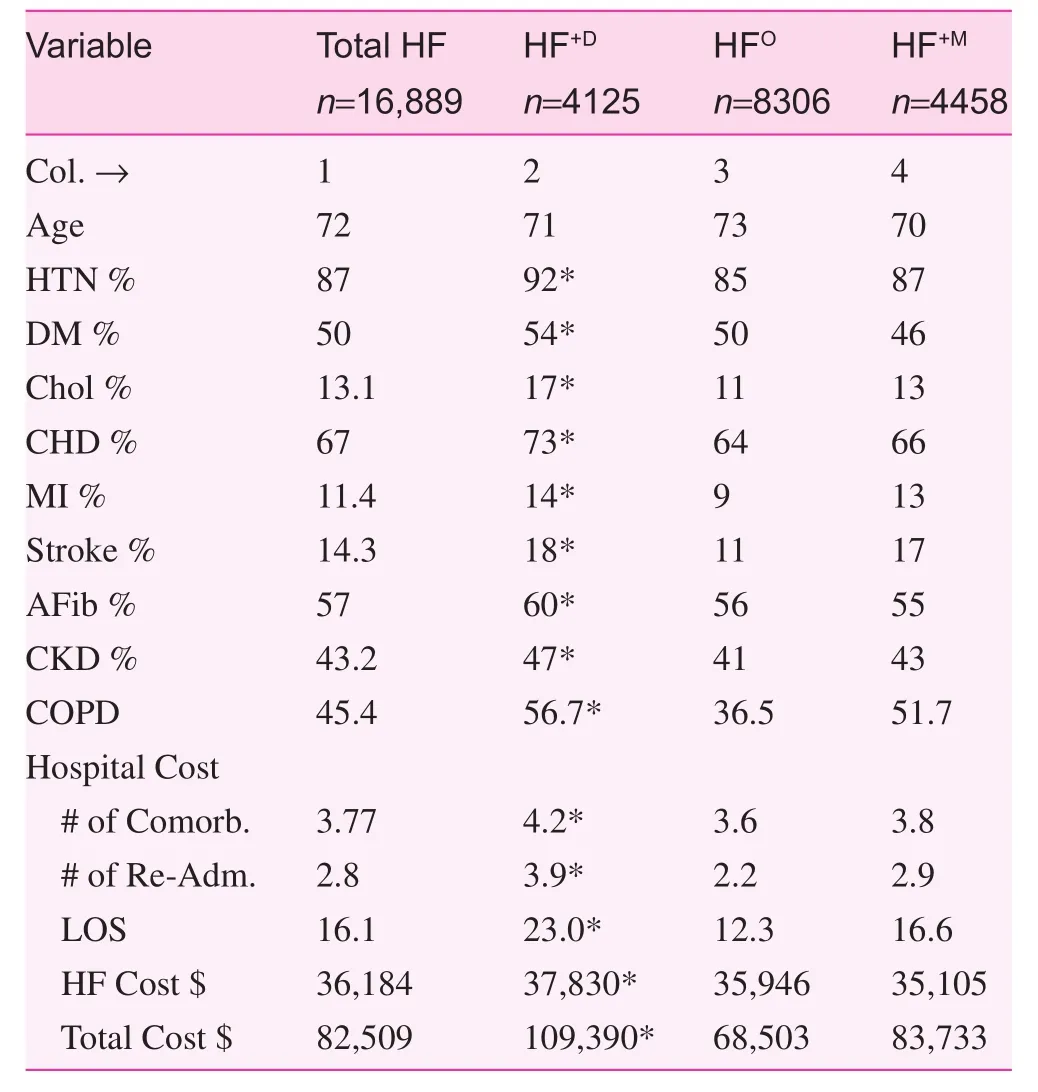
Table 2. Cardiovascular risk factors and annual hospitalization cost by HF group.
Additionally, some interesting patterns also emerged in our data. For example, although having other mental illnesses (HF+M) increased hospitalization costs compared with HFOpatients, depression/anxiety among HF patients notably increased hospitalization costs because of the complexities of greater comorbidities resulting in longer hospitalization.Clearly, HF patients use more resources while hospitalized,and this higher economic burden may possibly continue when the patient returns to the community without needed resources [42].
Our analyses of racial differences revealed a more complex pattern. Although whites with HF had a higher prevalence of depression/anxiety (possibly related to older age or a pre-existing condition), black HF patients (both males and females) had incurred the greatest hospitalization costs. This was especially true of black males, whose hospitalization costs appear to be related to a greater number of comorbidities that may have produced more complex conditions. These observations were especially striking because black men were the youngest in our race-gender groups. Previous observations regarding the possibility of racial bias and discrimination in accessing services [49] may add to worsening of conditions in blacks, which results in higher costs. Further, higher per capita hospital costs among blacks (in particular black males) suggest that HF+Dblack males may seek services late in the progression of their disease [50], which in turn requires more services and longer hospitalization. In addition, given the general trend of increased prevalence of depression/anxiety combined with comorbid conditions, our data raise the concern that cultural differences in the expression of depressed symptoms may be different for blacks, and thus may not be measureable by our current standard instruments. Data on this postulation is limited.
Gender differences in hospital costs also require further research. Although more males than females have HF, a greater number of HF female patients had depression. Despite the total health care costs being higher among men, the fact that women outnumbered men in the HF+Dgroup (64% vs.36%) suggests that considerable savings might be realized if costs attributable to depression/anxiety are reduced among women first.
Finally, we noted that these HF patients had numerous comorbidities, such as hypertension, diabetes, and chronic kidney disease, that were highly prevalent among blacks; however, the high prevalence of these medical disorders among blacks calls for optimal therapy [51, 52] and both primary and secondary preventive programs to reduce hospitalizationin underserved communities. Further reduction in hospitalization may also be achieved through coordination of community-based resources for the HF patients who have complex co-existing conditions. Overall, it is important to recognize the need to focus on widespread dissemination, adoption, and implementation of proven interventions for the control of HF and its associated comorbidities.
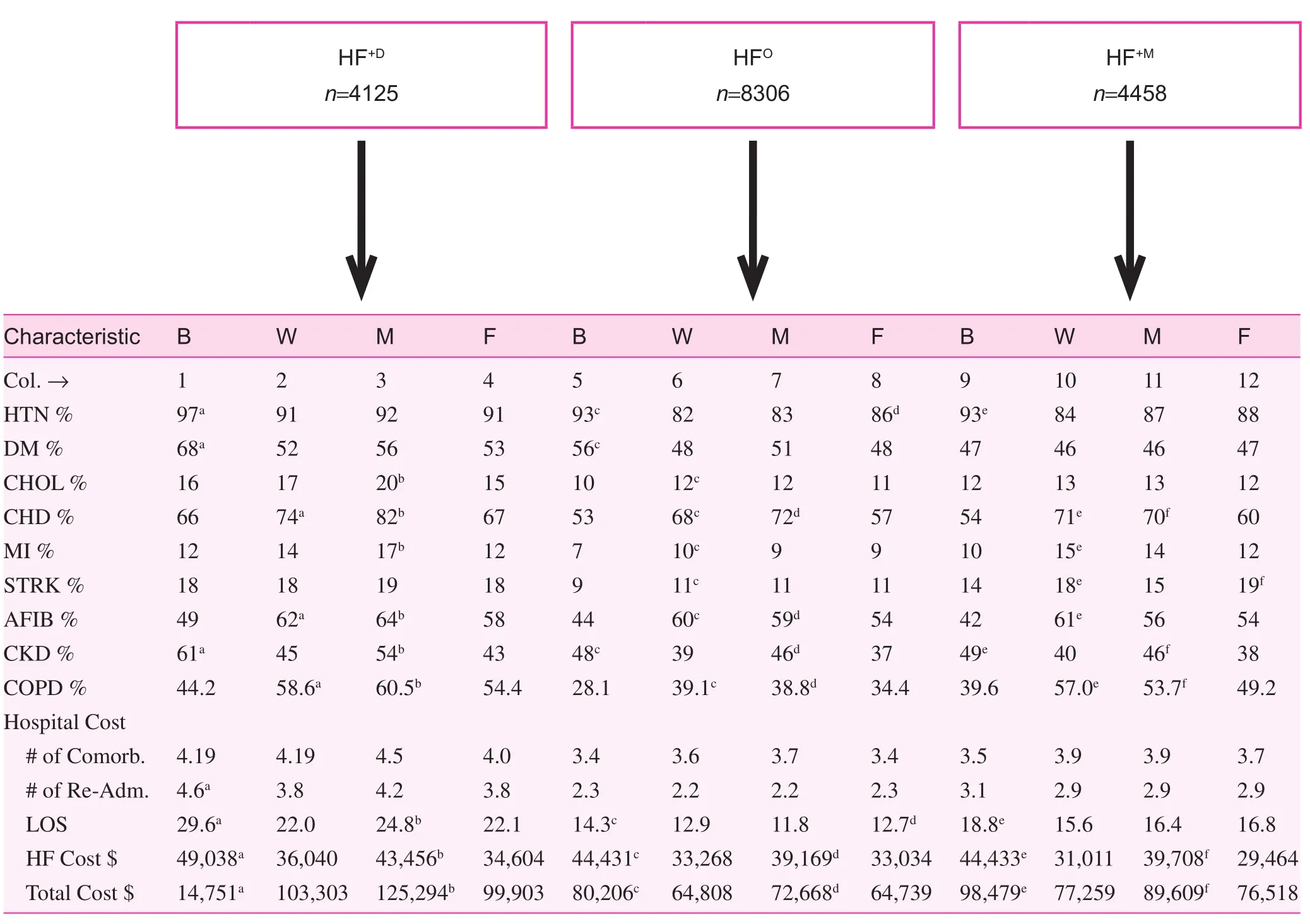
Table 3. Heart failure patient characteristics and hospital costs of three heart failure groups by race and gender
Limitations
Our findings were limited because the hospital discharge files (HDDS) do not include patients from the Department of Veterans Affairs (VA) hospitals or mental health hospitals.Further, the HDDS data are administrative files compiled by the Division of Health Statistics (Tennessee Department of Health). These files provide limited demographic information, such as patient age, gender, race/ethnicity,county of residence, postal zip code, date of admission/discharge, primary and secondary diagnoses (ICD-9 codes),principal procedure codes, and costs. These files do not provide data pertaining to patient marital status, education,or annual income. No clinical data are provided regarding medications used, tests performed, test results, severity or duration of illness, or symptom in dices used in arriving at clinical judgments/diagnoses. Further, these files lack details of diagnoses or comorbid conditions, which may shed additional light on racial and gender differences in health care costs. For the sake of maintaining confidentiality of records, patient-assigned identification numbers change every year, and hence it is not possible to follow a patient in the hospital discharge data beyond a given year. Because these potential confounding factors might affect the magnitude of observed racial differences, there is a need for caution in interpreting the results, and for additional research based on expanded data. Despite these and other limitations,however, we believe the present data provide useful insights regarding the impact of depression on hospitalization costs in Tennessee. Additionally, the HF sample, including 23%blacks, represents the demographic characteristics of the Tennessee population.
Conclusion
HF patients with depression/anxiety have higher hospitalization costs compared with those without such diagnoses or compared with those with other mental health diagnoses in these data. Both primary and secondary prevention programs,along with community-based resources, are needed to reduce length of hospital stays for HF patients. Although blacks have higher hospital costs than whites, epidemiologic studies are needed to examine whether or not the high health care costs among blacks are caused by delays in treatment and/or poor access to services, which in turn may lead to more complex problems, more extensive treatments, and longer hospitalizations. Although further studies are needed to unmask the factors that underpin the findings in this study, there appears to be a clear need for concerted efforts to improve the dissemination, adoption, and implementation of evidence-based interventions for HF and its associated comorbidities across all patient groups in an effort to maximize the population health impact and reduce the economic burden of HF on our health care system.
Acknowledgements
This paper was presented at the World Congress of Cardiology,Dubai, UAE.
conflict of Interest
The authors declare no conflict of interest.
Funding
The work was partially supported by several grants to Tennessee State University (CDC grant #ED072081100, a NCI grant [5U54CA163066; B. Husaini, PI]). Partial support for Levine, Husaini, and Cain was also provided by NIH grant #P20MD000516 (National Center on Minority Health & Health Disparity to Meharry Medical College).Sampson’s effort was supported, in part, by the Harold Amos Medical Faculty Award of the Robert Wood Johnson Foundation.
Authors’ contributions: Husaini B, Levine R, and Sampson U wrote the manuscript text; Cain V, Novotny M, and Husaini,B analyzed the data and prepared the tables; Moonis M was involved with discussion development. All authors reviewed and approved the manuscript.
1. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics – 2013 update:a report from the American Heart Association. Circulation 2013;127(1):e6–245.
2. Huffman JC, Smith FA, Blais MA, Taylor AM, Januzzi JL, Fricchione GL. Pre-existing major depression predicts in-hospital cardiac complications after acute myocardial infarction. Psychosomatics 2008;49(4):309–16.
3. Saveanu RV, Mayes T. Diagnosing depression in congestive heart failure. Heart Fail Clin 2011;7(1):75–9.
4. Pena FM, Modenesi Rde F, Piraciaba MC, Marins RM, Souza LB, Barcelos AF, et al. Prevalence and variables predictive of depressive symptoms in patients hospitalized for heart failure.Cardiol J 2011;18(1):18–25.
5. Shen BJ, Eisenberg SA, Maeda U, Farrell KA, Schwarz ER,Penedo FJ, et al. Depression and anxiety predict decline in physical health functioning in patients with heart failure. Ann Behav Med 2011;41(3):373–82.
6. Pena FM, da Silva Soares J, Paiva BT, Piraciaba MC, Marins RM,Barcellos AF, et al. Sociodemographic factors and depressive symptoms in hospitalized patients with heart failure. Exp Clin Cardiol 2010;15(2):e29–32.
7. Cully JA, Johnson M, Moffett ML, Khan M, Deswal A. Depression and anxiety in ambulatory patients with heart failure. Psychosomatics 2009;50(6):592–8.
8. Lea P. The effects of depression in heart failure. Dimens Crit Care Nurs 2009;28(4):164–8.
9. Delville CL, McDougall G. A systematic review of depression in adults with heart failure: instruments and incidence. Issues Ment Health Nurs 2008;29(9):1002–17.
10. Watson K, Summers KM. Depression in patients with heart failure: clinical implications and management. Pharmacotherapy 2009;29(1):49–63.
11. Rutledge, T, Reis VA, Linke SE, Greenberg BH, Mills PJ.Depression in heart failure: a meta-analytic review of prevalence,intervention effects, and associations with clinical outcomes.J Am Coll Cardiol 2006;48(8):1527–37.
12. Bekelman DB, Havranek EP, Becker DM, Kutner JS,Peterson PN, Wittstein IS, et al. Symptoms, depression,and quality of life in patients with heart failure. J Card Fail 2007;13(8):643–8.
13. Lesman-Leegte I, Jaarsma T, Coyne JC, Hillege HL,Van Veldhuisen DJ, Sanderman R. Quality of life and depressive symptoms in the elderly: a comparison between patients with heart failure and age- and gender-matched community controls.J Card Fail 2009;15(1):17–23.
14. Volz A, Schmid JP, Zwahlen M, Kohls S, Saner H, Barth J.Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. J Behav Med 2011;34(1)13–22.
15. Faller H, Steinbüchel T, St?rk S, Schowalter M, Ertl G,Angermann CE. Impact of depression on quality of life assessment in heart failure. Int J Cardiol 2010;142(2):133–7.
16. Sherwood A, Blumenthal JA, Hinderliter AL, Koch GG,Adams KF Jr, Dupree CS, et al. Worsening depressive symptoms are associated with adverse clinical outcomes in patients with heart failure. J Am Coll Cardiol 2011;57(4):418–23.
17. Lesman-Leegte I, van Veldhuisen DJ, Hillege HL, Moser D,Sanderman R, Jaarsma T. Depressive symptoms and outcomes in patients with heart failure: data from the COACH study. Eur J Heart Fail 2009;11(12):1202–7.
18. Macchia A, Monte S, Pellegrini F, Romero M, D’Ettorre A,Tavazzi L. Depression worsens outcomes in elderly patients with heart failure: an analysis of 48,117 patients in a community setting. Eur J Heart Fail 2008;10(7):714–21.
19. Freedland KE, Carney RM, Rich MW. Effect of depression on prognosis in heart failure. Heart Fail Clin 2011;7(1):11–21.
20. Zuluaga MC, Guallar-Castillón P, Rodríguez-Pascual C,Conde-Herrera M, Conthe P, Rodríguez-Artalejo F. Mechanisms of the association between depressive symptoms and long-term mortality in heart failure. Am Heart J 2010;159(2):231–7.
21. Jenner RC, Strodl ES, Schweitzer RD. Anger and depression predict hospital use among chronic heart failure patients. Aust Health Rev 2009;33(4):541–8.
22. Song EK, Lennie TA, Moser DK. Depressive symptoms increase risk of rehospitalisation in heart failure patients with preserved systolic function. J Clin Nurs 2009;18(13):1871–7.
23. Jünger J, Schellberg D, Müller-Tasch T, Raupp G, Zugck C,Haunstetter A, et al. Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 2005;7(2):261–7.
24. Jiang W, Alexander J, Christopher E, Kuchibhatla M,Gaulden LH, Cuffe MS, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med 2001;161(15):1849–56.
25. Azevedo A, Bettencourt P, Fri?es F, Alvelos M, Abreu-Lima C,Hense HW, et al. Depressive symptoms and heart failure stages.Psychosomatics 2008;49(1):42–8.
26. Sherwood A, Blumenthal JA, Trivedi R, Johnson KS,O’Connor CM, Adams KF Jr, et al. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med 2007;167(4):367–73.
27. Sullivan M, Simon G, Spertus J, Russo J. Depression-related costs in heart failure care. Arch Intern Med 2002;162(16);1860–6.
28. Sayers SL, Hanrahan N, Kutney A, Clarke SP, Reis BF,Riegel B. Psychiatric comorbidity and greater hospitalization risk, longer length of stay, and higher hospitalization costs in older adults with heart failure. J Am Geriatr Soc 2007;55(10):1585–91.
29. Rumsfeld JS, Jones PG, Whooley MA, Sullivan MD, Pitt B,Weintraub WS, et al. Depression predicts mortality and hospitalization in patients with myocardial infarction complicated by heart failure. Am Heart J 2005;150(5):961–7.
30. Burns MJ, Cain VA, Husaini BA. Depression, service utilization and treatment costs among medic are elderly: Gender Differences. Home Health Care Serv Q 2001;19(3):35–44.
31. Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail 2005;11(6):455–63.
32. Echols MR, Jiang W. Clinical trial evidence for treatment of depression in heart failure. Heart Fail Clin 2011;7(1):81–8.
33. Tousoulis D, Antonopoulos AS, Antoniades C, Saldari C,Stefanadi E, Siasos G, et al. Role of depression in heart failure–choosing the right antidepressive treatment. Int J Cardiol 2010;140(1):12–8.
34. Fraguas R, da Silva Telles RM, Alves TC. A double-blind,placebo-controlled treatment trial of citalopram for major depressive disorder in older patients with heart failure: the relevance of the placebo effect and psychological symptoms.Contemp Clin Trials 2009;30(3):205–11.
35. Cully JA, Jimenez DE, Ledoux TA, Deswal A. Recognition and treatment of depression and anxiety symptoms in heart failure.Prim Care Companion J Clin Psychiatry 2009;11(3):103–9.
36. Silver MA. Depression and heart failure: an overview of what we know and don’t know. Cleve Clin J Med 2010;77(Suppl 3):S7–11.
37. Evangelista LS, Ter-Galstanyan A, Moughrabi S, Moser DK.Anxiety and depression in ethnic minorities with chronic heart failure. J Card Fail 2009;15(7):572–9.
38. Gottlieb SS, Khatta M, Friedmann E, Einbinder L, Katzen S,Baker B, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol 2004;43(9):1542–9.
39. Havranek EP, Spertus JA, Masoudi FA, Jones PG, Rumsfeld JS.Predictors of the onset of depressive symptoms in patients with heart failure. J Am Coll Cardiol 2004;44(12):2333–8.
40. Sullivan MD, Newton K, Hecht J, Russo JE, Spertus JA.Depression and health status in elderly patients with heart failure:a 6-month prospective study in primary care. Am J Geriatr Cardiol 2004;13(5):252–60.
41. Lee WC, Chavez YE, Baker T, Luce BR. Economic burden of heart failure: A summary of recent literature. Heart Lung 2004;33(6):362–71.
42. Wexler DJ, Chen J, Smith GL, Radford MJ, Yaari S,Bradford WD, et al. Predictors of costs of caring for elderly patients discharged with heart failure. Am Heart J 2001;142(2):350–7.
43. Liao L, Anstrom KJ, Gottdiener JS, Pappas PA, Whellan DJ,Kitzman DW, et al. Long term costs and resource use in elderly participants with congestive heart failure in the Cardiovascular Health Study. Am Heart J 2007;153(2):245–52.
44. Zimmerman M, McDermut W, Mattia JI. Frequency of anxiety disorders in psychiatric outpatients with major depressive disorder. American Journal of Psychiatry 2000;157(8):1337–40.
45. Bowen RC, Kohout J. The relationship between agoraphobia and primary affective disorders. Can Psychiatr Assoc J 1979;24(4):317–22.
46. Husaini B, Levine R, Sharp L, Cain V, Novotny M, Hull P, et al.Depression Increases Stroke Hospitalization Cost: An Analysis of 17,010 Stroke Patients in 2008 by Race and Gender. Stroke Res Treat 2013;2013:846732. DOI: 10.1155/2013/846732.
47. Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. Healthy People 2010 Stat Notes 2001;(20):1–10.
48. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies:Development and validation. J Chronic Dis 1987;40(5):373–83.
49. Chae DH, Nuru-Jeter AM, Adler NE, Brody GH, Lin J,Blackburn EH, et al. Discrimination, racial bias, and telomere length in African-American men. Am J Prev Med 2014;46(2):103–11.
50. Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB,Dracup K, et al. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke. Circulation 2006;114(2):168–82.
51. Egan BM, Zhao Y, Li J, Brzezinski WA, Todoran TM, Brook RD,et al. Prevalence of optimal treatment regimens in patients with apparent treatment-resistant hypertension based on of fice blood pressure in a community-based practice network. Hypertension 2013;62(4):691–7.
52. Banegas JR, Navarro-Vidal B, Ruilope LM, de la Cruz JJ,López-García E, Rodríguez-Artalejo F, et al. Trends in Hypertension control among the older population of Spain from 2000 to 2001 to 2008 to 2010. Circ Cardiovasc Qual Outcomes 2015;8(1):67–76.
1. Center for Prevention Research,Tennessee State University, Nashville, TN, USA
2. Department of Family and Community Medicine, Baylor College of Medicine, Houston, TX, USA
3. Vanderbilt University Medical Center, Nashville, TN, USA
4. Department of Neurology, Memorial Hospital, Worcester, MA,USA
Baqar A. Husaini
Center for Preventive Research,Tennessee State University, 3500 John Merritt Blvd., Nashville,TN 37209, USA
Tel.: +615-210-1132
Fax: +615-963-5068
E-mail: bhusaini@tnstate.edu
10 April 2015;
5 May 2015
 Family Medicine and Community Health2015年2期
Family Medicine and Community Health2015年2期
- Family Medicine and Community Health的其它文章
- Evaluation of obstetrics procedure competency of family medicine residents
- Student self-assessment of strengths and needed improvements during a family medicine clerkship
- Rural congestive heart failure mortality among US elderly,1999–2013: Identifying counties with promising outcomes and opportunities for implementation research
- Exploring point-of-care transformation in diabetic care: A quality improvement approach
- Hospitalizations and healthcare costs associated with serious,non-lethal firearm-related violence and injuries in the United States,1998–2011
- Adult immunization improvement in an underserved family medicine practice
