Full laparoscopic anatomical liver segment VII resection with preferred Glissonean pedicle and dorsal hepatic approach
Ji Zhou ,Ying-Hui Song ,Yu-Chen Qi ,Ou Li ,Guo-Yi Xi ,Meng-Jun Mo ,Chung Peng ,b,Su-Li Liu ,b,c,?
a Department of Hepatobiliary Surgery, Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Changsha 410 0 05,China
b Hunan Research Center of Biliary Disease, Changsha 410 0 05, China
c Central Laboratory of Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Changsha 410 0 05, China
d Department of Pathology, Hunan Provincial People’s Hospital (The First Affiliated Hospital of Hunan Normal University), Changsha 410 0 05, China
Anatomical liver resection was an option for liver cancer proposed by the Japanese scholar Masatoshi Makuuchi in 1985 [1] .Reich et al. performed the first laparoscopic liver resection in 1991 [2] . The safety and effectiveness of laparoscopic anatomical liver resection had been verified in recent years [2–4] . However,laparoscopic anatomical segment VII liver resection (LAS7) was the most difficult procedure because of complex adjacent structures,difficult exposure,and limited laparoscopic view [ 3,5 ]. Therefore,the LAS7 had only been explored in some large national and international medical centers. Ishizawa et al. [3] reported a surgical protocol to resect segment VII of the liver that included parenchymal separation from the foot to the head side,which was identical to open anatomical liver resection. However,the liver pedicle of segment VII is difficult to locate and ligate precisely; and it is diffi-cult to show the ischemic demarcation line completely. Herein we implemented a new,convenient approach for precise liver resection that can be used during LAS7.
From October 2019 to June 2021,12 patients underwent LAS7 with preferred Glissonean pedicle and dorsal hepatic approach in our department. Each patient underwent an adequate preoperative imaging evaluation,including preoperative CT and threedimensional (3D) reconstruction ( Fig. 1 ). Five patients had a history of hepatitis B and three had a history of cirrhosis. Table 1 showed the demographics of the patients and the perioperative data.
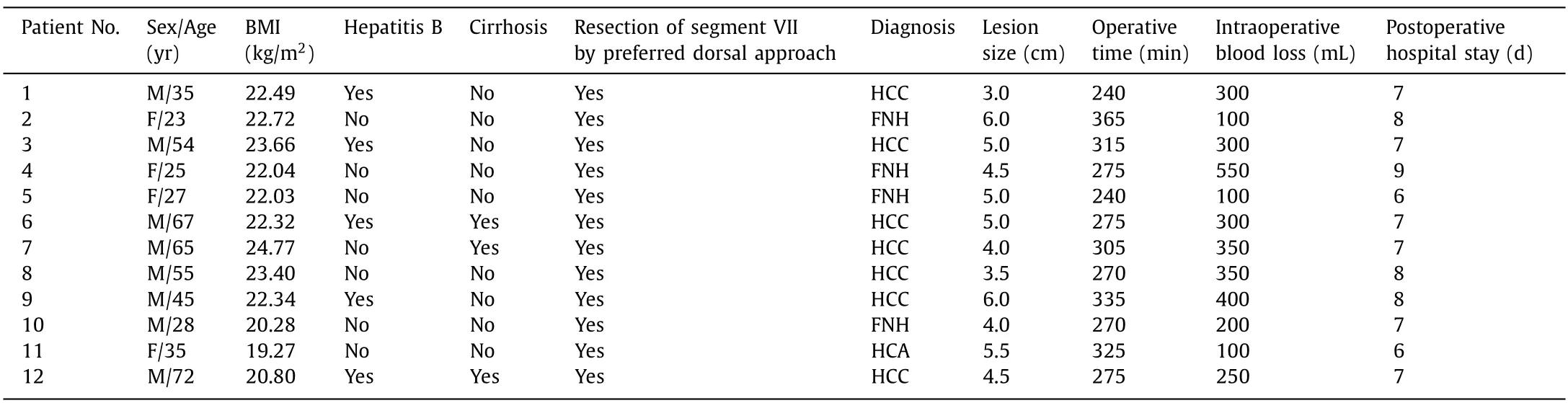
Table 1Patients’ demographics and perioperative data.
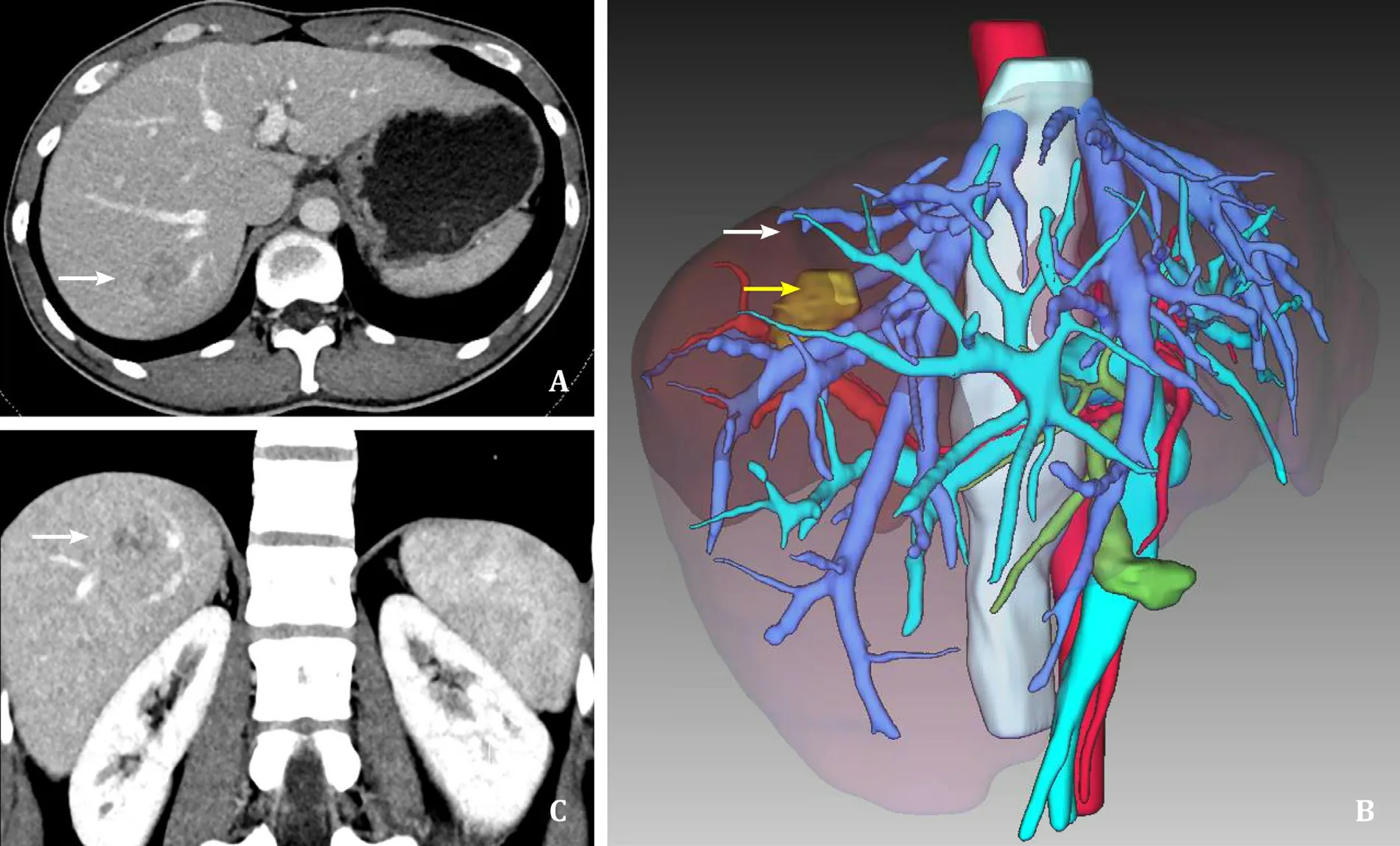
Fig. 1. Preoperative imaging evaluation. A: Preoperative CT imaging,segment VII mass (white arrow). B: Accurate preoperative three-dimensional CT scans,segment VII mass(yellow arrow) and segment VII (white arrow). C: Preoperative coronal CT imaging,segment VII mass (white arrow). CT: computed tomography.
The patients were placed in the left reclined position that was maintained in an oblique position of left with the head high and the feet low at approximately 30 degrees. Importantly,it was an essential step to find the liver pedicle of segment VII and block it.The surgeon was located on the left side of the patient to perform the dissection of the second hepatic hilum,the right perihepatic ligament and the right posterior liver pedicle. After that,the liver pedicle of segment VII was found and blocked. Then,the surgeon turned to the right side of the patient to perform the dissection of the third hepatic hilar and liver parenchyma. The first assistant and the laparoscopic lens holder stood on the left side of the patient.The laparoscopic display screen was placed on the side of the patient’s head. The trocar hole layout used five bushings placed in a fan shape ( Fig. 2A ).
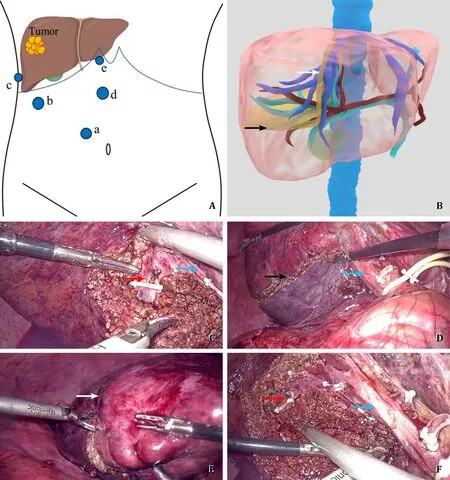
Fig. 2. Intraoperative picture. A: Locations of the trocars. a: 10 mm trocar on 5 cm slightly medially below the right midclavicular line; b: 12 mm trocar on 2 cm below the rib margin in the right anterior axillary line; c: 5 mm trocar on the 8th intercostal space in the right mid-axillary line; d: 12 mm trocar on 5 cm below the xiphoid process of the ventral midline; e: 5 mm trocar on the right of the xiphoid. B: Simulation of intraoperative resection of liver,including two resection surfaces,sagittal plane(white arrow),the coronal plane (black arrow). C: The liver pedicle of segment VII (red arrow) was located and severed along the right liver pedicle (blue arrow). D: Ischemia demarcation line on visceral surface of the liver (black arrow),the right liver pedicle (blue arrow). E: Ischemia demarcation line on diaphragmatic surface of the liver (white arrow). F: The liver pedicle of segment VII (red arrow) and the right liver pedicle (blue arrow).
In total,the operation was guided by four hepatic resection routes and two hepatic resection planes ( Fig. 2B ). The sagittal plane of the segment VII liver resection was determined on the right side of the inferior vena cava (IVC) and the right hepatic vein(RHV). The coronal plane of the segment VII liver resection was determined by the ischemic demarcation line on the surface of the liver and the horizontal line of the right branch of the portal vein.Firstly,the surgeon severed the round hepatic ligament and the right coronal ligament to fully dissociate the second hepatic portal. The liver was pulled down to expose the root of the RHV into the IVC as long as possible. Then the operator cut the omentum to the preset pringle blocking band and temporarily blocked it,exposing the right posterior liver pedicle along the Rouviere sulcus. Subsequently,the surgeon incised the liver parenchyma approximately 2 cm deep,dissociated along the right posterior pedicle of the liver,and dissected several thick liver pedicles of segment VI. The liver pedicle of segment VII (pedicle VII,P7) was exposed externally and posteriorly to the hepatic dorsal of the head side ( Fig. 2C ). The P7 was suspended and clamped with a laparoscopic vascular clamp. The surgeon stopped clamping the hepatoduodenal ligament,then the boundary of ischemia delimitation between the liver segment VII and the VI or VIII segments was observed to confirm the real liver pedicle of segment VII ( Fig. 2C ).Electrocoagulation lines were recorded along the dorsal liver using an ultrasound scalpel according to the boundary of the ischemia area ( Fig. 2D and E ). After recording the boundary line of liver segment VII by electrocoagulation,the P7 was routinely severed ( Fig. 2F ). The right hepatic vein trunk was found in the vein after finding the end of the vein between segment VI and VII during the operation. Switching to an anterior approach for hepatic dissection,the surgeon traced the pre-cut line with electrocoagulation on the diaphragmatic surface of the liver. The RHV and the right side of the IVC were used as the plane of hepatic dissection.
LAS7 was completed from the surface to depth,and from the foot side to cephalic side,until the right posterior side of the RHV and the right side of the posterior IVC were fully exposed. The residual liver section showed the residual P7 ( Fig. 2F ). At the end of the liver section,the right hepatic vein and the right liver pedicle were fully exposed and preserved ( Fig. 3 ).
None of the cases was converted to open surgery in our study.The average duration of the surgery was 290.83 ± 38.37 min,and the average volume of blood loss was 275.00 ± 135.68 mL. The average size of the lesion was 4.67 ± 0.94 cm. The average size of hepatocellular carcinoma (HCC) was 4.43 ± 1.02 cm. The average postoperative hospital stay was 7.25 ± 0.87 days. No significant postoperative complications were observed. Pathological diagnosis showed 7 HCC cases,4 focal nodular hyperplasia (FNH),and 1 hepatocellular adenoma (HCA). Most importantly there was no recurrence of HCC within a median follow-up of 24 months. Our study also showed that smaller size of HCC was safe and suitable for LAS7 ( Table 1 ).The postoperative follow-up was approximately 6-48 months after the operation.
There was no clear boundary between the hepatic segment VII and the caudal lobe of the liver,making it difficult to pursue orientation during surgical liver resection. Our novel surgical approach for anatomical segment VII liver resection mainly includes four crucial point: (i) the right liver pedicle,(ii) the inferior vena cava,(iii) the right hepatic vein,and (iv) the ischemia boundary on the liver surface to achieve anatomical hepatic VII resection. We recommend that segment VII and the right caudate lobe were removed guided by four hepatic resection routes and two hepatic resection planes ( Fig. 2B ). Therefore,we could achieve a clear surgical route and a standardized surgical procedure. Guided by the right liver pedicle with preoperative 3D reconstruction technology( Fig. 1B ),the liver pedicle of segment VII was searched precisely with the liver parenchyma incised [ 6,7 ].
Hepatic blood flow was blocked to form the ischemia demarcation line of hepatic surface ( Fig. 2D and E ). The ischemic demarcation line on liver surface and the right liver pedicle was used as the plane of hepatic resection for segment VII. Importantly,the liver pedicle of segment VI should be protected during the operation. According to the principle of hepatic lobe Couinaud segmentation,guided by the right hepatic vein,segment VII was located on the right side of the right hepatic vein. Liver resection of segment VII in the right hepatic vein and the midline of the inferior vena cava was used as the plane of hepatic dissection [ 8,9 ]. Under the guidance of middle line of the IVC and the RHV,the right caudal lobotomy was combined to ensure the safety of the resection margin and the accuracy of the surgical resection route ( Fig. 2F ).
As the laparoscopic equipment was updated,with the application and popularization of the ultrasonic knife,laparoscopic liver resection technology improved rapidly [10] . The safety and efficacy of laparoscopic anatomical liver resection have been verified [5] . To ensure the safety and feasibility of laparoscopic segment VII liver resection,it was necessary to understand the difficulty of the LAS7,and formulate a feasible preoperative resection strategy. With the development and widespread application of 3D reconstruction,surgeons have gained a deeper understanding of the special anatomical structure and complex vascular system of the liver [ 11,12 ]. Furthermore,it was essential to adequately expose segment VII by adjusting the surgical position of the patient as well as disassociating or pulling the right liver [ 13,14 ]. In our cases,virtual liver resection and 3D reconstruction were performed to present the relationship between the tumor and surrounding blood vessels. These were designed to achieve R0 resection.
Correct surgical approach planning and intraoperative ultrasound were used to confirm and correct the plane of the severed liver in real-time to reduce turning and ensure anatomical liver resection. With the accumulation of experience in laparoscopic hepatectomy,the improvement of theory,and the advancement of technology,LAS7 was made feasible in some of the major hepatobiliary surgery centers. At the same time,patients could achieve a better postoperative survival.
The operator had to be familiar with the strategy of the preferred Glissonean pedicle with dorsal hepatic approach in LAS7.First,our surgical strategy was to reduce the risk of metastasis due to extrusion of the segment VII tumor. With our novel approach,the liver pedicle of segment VII was handled preferentially,and the hepatic venous branches outflow needed to be handled later.Second,The operator avoided the corresponding congestion of segment VII caused by cutting the hepatic venous branches,which could cause bleeding on the wound surface and lead to unclear or even more serious consequences of the operative field [ 9,15 ]. Third,bipolar electrocoagulation was used to deal with every bleeding area of the liver section to make the resection plane dry and clean.The surgical field of vision must be clear to ensure an accurate operation. If bleeding was not controlled in time,it would cause unclear vision and affect the operation. Fourth,the right posterior inferior vein of the liver should not be severed to prevent obstruction of vascular reflux in the segment VI of the liver.
In our study,the 12 patients were successfully treated with LAS7 using a preferred Glissonean pedicle and dorsal hepatic approach. Compared to those who underwent conventional anatomical hepatic segment VII resection,our patients had less intraoperative bleeding,better postoperative recovery,and shorter postoperative hospital stay. The preferred Glissonean pedicle hepatectomy conformed to the concept of anatomic hepatectomy. Focusing on the liver pedicle,an anatomical hepatectomy was performed at the ischemic boundary after occlusion of the P7 to make the operation more precise [16] . It reduced the risk of surgical bleeding,ensured structural integrity and maximized functional volume of the remaining liver,and surgically benefited the patient. In comparison,traditional hepatectomy required a free perihepatic ligament and repeated liver reversal which increase the risk of tearing the hepatic vein. In conventional segment VII liver resection,the liver parenchyma above the level of the right hepatic vein was first severed after the completion of the P7 occlusion and the appearance of the ischemia demarcation line [17] . With our novel approach,the hepatic parenchyma below the plane of the right hepatic vein was separated through dorsal hepatic approach to reach the plane of the main right hepatic vein. Laparoscopically,the root of the right hepatic vein can be revealed first from the dorsal side and gradually exposed to the periphery,reducing hepatic vein injury and the risk of intraoperative bleeding.
In conclusion,the LAS7 with preferred Glissonean pedicle and dorsal hepatic approach is a complex liver resection operation with a long learning curve. It should be performed in large hepatobiliary surgery centers by experienced hepatobiliary surgeons. In our study,the approach was safe and feasible. Therefore,this surgical approach could be a new option for the treatment of patients with liver lesions in segment VII.
Acknowledgment
None.
CRediT authorship contribution statement
JiaZhou:Data curation,Formal analysis,Writing – original draft,Writing – review & editing.Ying-HuiSong:Data curation,Formal analysis,Funding acquisition,Writing – original draft,Writing – review & editing.Yu-ChenQi:Data curation,Formal analysis,Writing – original draft,Writing – review & editing.OuLi:Conceptualization,Writing – review & editing.Guo-YiXia:Conceptualization,Writing – review & editing.Meng-JunMo:Conceptualization,Writing – review & editing.ChuangPeng:Data curation,Funding acquisition,Writing – review & editing.Su-LaiLiu:Data curation,Formal analysis,Funding acquisition,Writing – review & editing.
Funding
This study was supported by grants from Clinical Medical Technology Innovation Guidance Project of Hunan Provincial Science and Technology Department (2020SK50915),Youth Talent of Hunan Province (2020RC3066),Natural Science Fund for Excellent Young Scholars of Hunan Province (2021JJ20003),Hunan Provincial Natural Science Foundation of China (2020JJ5610),Project of Hunan Provincial Health Commission (202104010997),Chen Xiao-Ping Foundation for Development of Science and Technology of Hubei Province (CXPJJH12000001-2020322),Natural Science Foundation of Changsha (kq2007023/kq2004115),and The Project of Improving the Diagnosis and Treatment Capacity of Hepatobiliary,Pancreas and Intestine in Hunan Province (Xiangwei [2019] No. 118).
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Hunan Normal University. Written informed consent for publication was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年5期
Hepatobiliary & Pancreatic Diseases International2023年5期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Right hepatectomy with a cholangiojejunostomy and hepaticojejunostomy for unilobar Caroli’s syndrome
- Total three-dimensional laparoscopic radical resection for Bismuth type IV hilar cholangiocarcinoma
- A surgical technique using the gastroepiploic vein for portal inflow restoration in living donor liver transplantation in a patient with diffuse portomesenteric thrombosis
- Combined hepatic segment color rendering technique improves the outcome of anatomical hepatectomy in patients with hepatocellular carcinoma
- Targeting mitochondrial transcription factor A sensitizes pancreatic cancer cell to gemcitabine
- Pathogen detection in patients with perihilar cholangiocarcinoma:Implications for targeted perioperative antibiotic therapy
