Pathogen detection in patients with perihilar cholangiocarcinoma:Implications for targeted perioperative antibiotic therapy
Felix Dondorf ,Mximilin Grf Alddin Ali Dee Oliver Rohlnd Philipp Felgendreff,Michel ArdeltUtz SettmcherFlk Ruchfuss
a Department of General, Visceral and Vascular Surgery, Jena University Hospital, Jena 07747, Germany
b Research Program "Else Kr?ner-Forschungskolleg AntiAge", Jena University Hospital, Jena 07747, Germany
Keywords: Perihilar cholangiocarcinoma Klatskin tumor Cholangitis Targeted antibiotic therapy Biliary drainage
ABSTRACT Background: Cholestasis should be relieved by biliary drainage prior to major liver resection. This condition is often associated with bacterial colonization of the otherwise sterile biliary system. Cholangitis reduces the regenerative capacity of the remaining liver. Therefore,targeted antibiotic therapy is a key feature in perioperative treatment in patients with perihilar cholangiocarcinoma (pCCC).Methods: Between December 1999 and December 2017,251 pCCC patients were treated in our center. In total,115 patients underwent a microbiological analysis. In addition to the characterization of the specific microorganisms and antibiotic resistance,we analyzed subgroups according to preoperative intervention.Results: Enterococci (87/254,34%) and Enterobacteria (65/254,26%) were the most frequently detected genera. In 43% (50/115) of patients,Enterococcus faecalis was found in the bile duct sample. Enterococcus faecium (29/115) and Escherichia coli (29/115) were detected in 25% of patients. In patients with percutaneous transhepatic biliary drainage (3/8,38%) or stents (24/79,30%),Enterococcus faecium was diagnosed most frequently ( P < 0.05). Enterococcus faecium and Klebsiella oxytoca were significantly more frequently noted in the time period after 2012 ( P < 0.05). With regard to fungal colonization,the focus was on various Candida strains,but these strains generally lacked resistance.Conclusions: pCCC patients exhibit specific bacterial colonization features depending on the type of preoperative biliary intervention. Specifically,targeted antibiosis should be applied in this patient cohort to minimize the risk of biliary complications after major liver resection. In our cohort,the combination of meropenem and vancomycin represents an effective perioperative medical approach.
Introduction
Painless icterus is often the first symptom of perihilar cholangiocarcinoma (pCCC),which occurs due to slowly progressing cholestasis. Often,due to the increasing tumor obstruction and the resulting stasis,cholangitis can appear as a “superinfection”,which can worsen the overall course of the patient [1] . The stasis itself as well as cholangitis deteriorates liver function,which may be associated with a “small-for-size syndrome” postoperatively,especially after extended liver resection. Xiong et al. [2] showed that pCCC patients typically present with concomitant obstructive jaundice,which results in high surgical morbidity and mortality in those undergoing major liver resection. Addressing this issue is highly relevant in the context of this tumor entity. It was already shown that the incidence of in-hospital mortality is significantly higher in patients with preoperative cholangitis than in patients without [3] .
The only reasonable and curative therapy for pCCC is radical surgery with the goal of R0 resection. In addition to resection of the extrahepatic bile duct,resecting the central liver segments is also necessary,depending on the type of pCCC. Thus,this condition typically results in “enbloc” resection with a significant loss of functional liver parenchyma [4] . Liver resection in jaundiced patients is a potentially harmful procedure [5] . Given that regeneration of the cholestatic liver is often limited,preoperative bile duct drainage is recommended but controversially discussed [5] . Decompression of cholestasis is a topic of discussion in the literature,especially the type of decompression [6] . In addition to internal relief by means of a stent,percutaneous transhepatic biliary drainage(PTBD) can also be performed as well as a nasobiliary tube,which is especially favored in Asia [ 7,8 ].
According to Teng et al. [9],the aim of preoperative biliary drainage is to increase liver tolerance to operative trauma and therefore improve the regenerative capacity of the remaining liver.At our center,we prefer endoscopic biliary drainage. However,we are aware that this is a circulus vitiosus,as the transpapillary stent carries the risk of ascending infections [10] .
The most common prophylactic antibiotics used during hepatopancreato-biliary surgery were first- or second-generation cephalosporins; however,variations in the regimens were noted [11] . If acute cholangitis is considered,current guidelines recommend initial treatment with a penicillin/beta-lactamase inhibitor combination,third/fourth-generation cephalosporin,fluoroquinolones or carbapenem [ 12,13 ].
The aim of the study was to analyze microbial contamination in cholestasis of pCCC patients and to obtain an overview of the common microorganisms and resistances to improve preoperative conditioning before major liver resection.
Methods
From December 1999 to December 2017,251 pCCC patients were treated in our center. Of these 251 patients,115 underwent an intraoperative microbiological diagnostic investigation. Of the 115 patients,10 had negative findings ( Fig. 1 ). The permission of the Ethics Committee was approved as part of patient care (No.2021-2204-data).
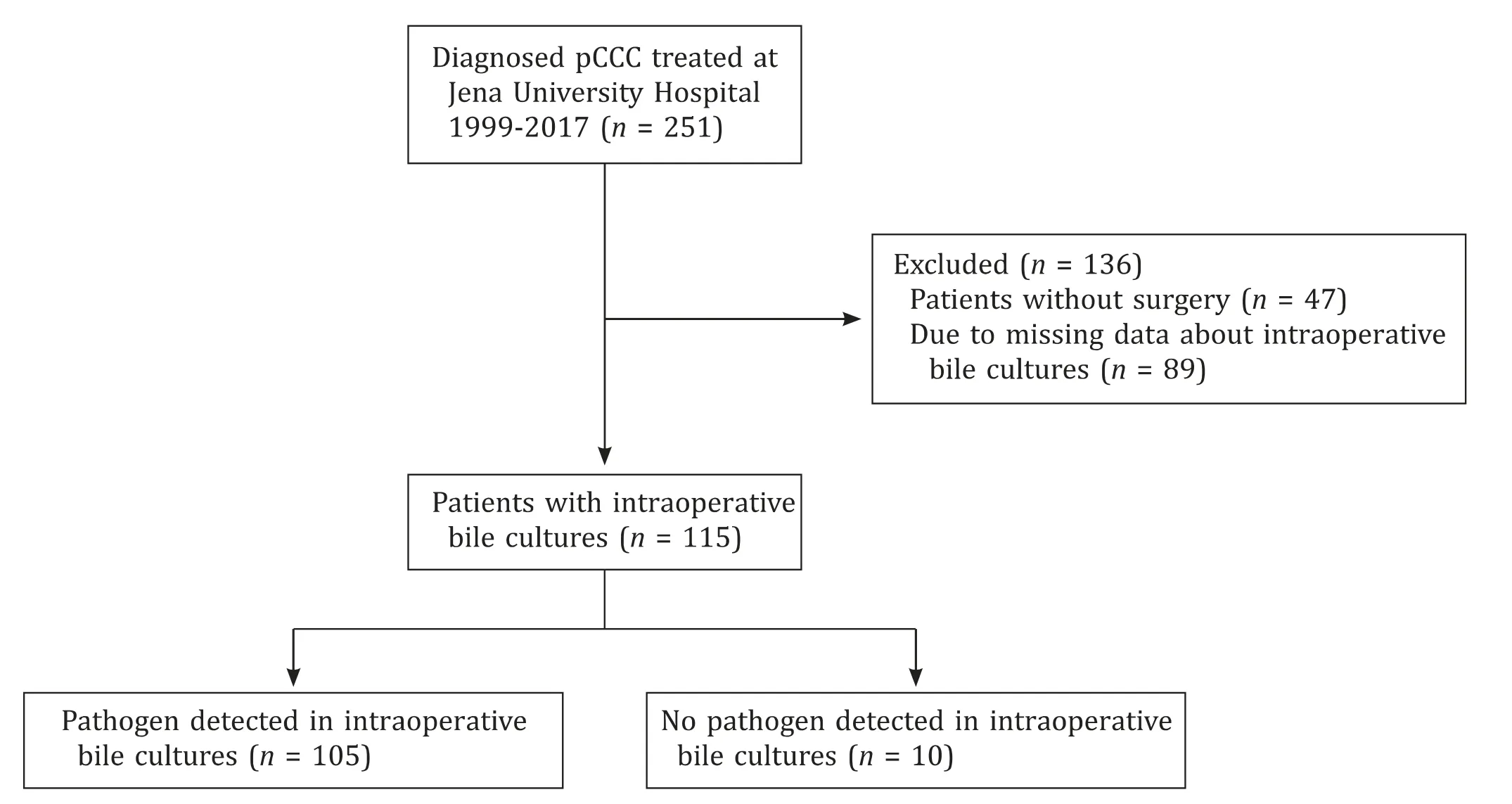
Fig. 1. Flowchart representation of patients selection in this study.
An intraoperative microbiological swab was routinely obtained from the bile duct. If available,the bile duct stent or the inserted PTBD was also sent for microbiological analysis.
According to our internal standard operating procedure (SOP),all patients received a single shot of cefuroxime/metronidazole(1.5 g/500 mg) preoperatively during the induction of anesthesia if there was no contraindication. Patients who exhibited an infected bile duct intraoperatively were treated prophylactically with antibiotics. In this case,cephalosporins were used. In patients who showed clinical or paraclinical signs of cholangitis postoperatively,antibiotics were selected depending on the intraoperative microbiology.
Due to the common antibiotics used in the literature [14],we focused on the main groups: penicillins,cephalosporins,fluoroquinolones and carbapenems. In addition,the most frequently used antibiotics in our institution were added after evaluation of the resistance findings. A total of 10 antibiotics and 3 antimycotics were shortlisted and analyzed.
In addition to the evaluation of the bacterial load,resistance was recorded. Subgroups were generated based on biliary drainage(stent/PTBD) and according to the following time periods: 1999-2011 (n= 51) and 2012-2017 (n= 64). The time intervals were chosen to create two approximately equal groups.
Statistical analysis was performed using SPSS statistical software (IBM,Armonk,NY,USA) and Microsoft Excel (Microsoft Corporation,Redmond,Washington,USA). Group differences were tested using Chi-square test. Significant differences between groups were defined asP<0.05.
Results
Characteristics of study patients
One hundred and fifteen patients were finally included,with a mean age of 63.1 years and 44 (38%) were females. A total of 254 microbiological findings were obtained from the 115 patients in whom intraoperative microbiology was evaluated. Regarding the 254 microbiological results,199 were from bile,and 55 from the stent/PTBD. In 89 patients (77%),several pathogens were cultured,in the sense of a multiple colonization and in 16 patients (14%)only one pathogen was diagnosed. Ten patients (9%) had no colonization of the bile. Of the 115 patients,79 had prior stenting,8 had PTBD,and 28 had no prior biliary drainage.
Characteristics of pathogens
In the microbiological examinations,Enterococci(87/254,34%)andEnterobacteria(65/254,26%) were detected most frequently.Furthermore,Candidae(22/254,9%),Streptococci(22/254,9%) andKlebsiella(21/254,8%) were also detected ( Fig. 2 ).
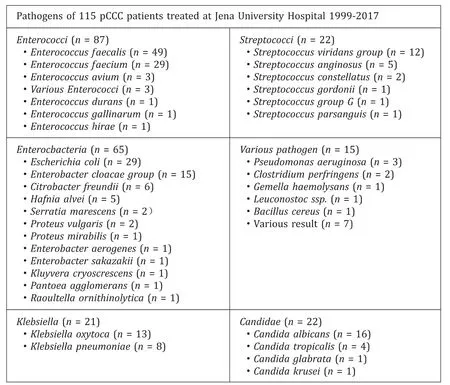
Fig. 2. Detection of the individual germs with the case number of detection in parentheses.
Enterococcusfaecaliswas the most frequently detected in the microbiological examination of the bile duct sample (50/115,43%).Enterococcusfaecium(29/115) andEscherichiacoli(29/115) were detected in 25% of patients. Colonization withCandidaalbicanswas detected in 14% (16/115) of patients. ForKlebsiellaoxytoca,the bile duct sample was positive in 11% (13/115) of the screened patients.
With regard to the interventions (stent/PTBD/none),Enterococ-cusfaeciumwas detected in only 7% (2/28) of patients without any biliary decompression. In patients with PTBD (3/8,38%) or a stent (24/79,30%),Enterococcusfaeciumwas thus detected more frequently (P= 0.037) ( Fig. 3 ).
Sensitivity of pathogens to antibiotics and antifungals
Considering all pathogens detected,the resistance situation for the selected antibiotics/antimycotics is shown in Fig. 4 .
The resistance situation of the selected antibiotics and antifungals was subsequently investigated on a pathogen-specific basis.Overviews of the sensitivities of the pathogens recorded,as shown in Fig. 5,were compiled.
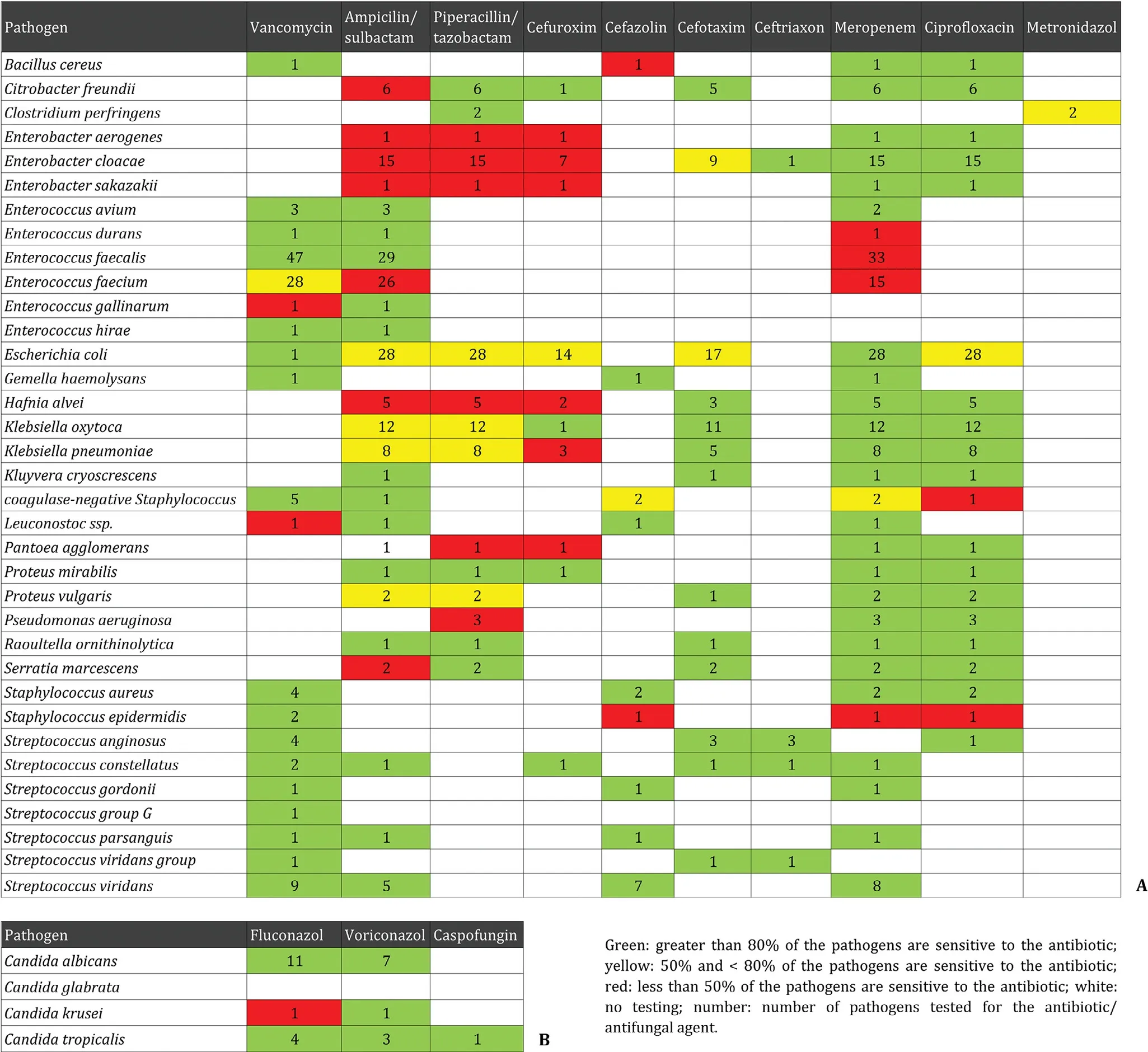
Fig. 5. Sensitivity status of the pathogens ( A ) and mycotic pathogens ( B ) detected.
Furthermore,the frequencies of the selected pathogens were investigated in two groups divided according to the time period of the cases (1999-2011 and 2012-2017),as shown in Fig. 6 .
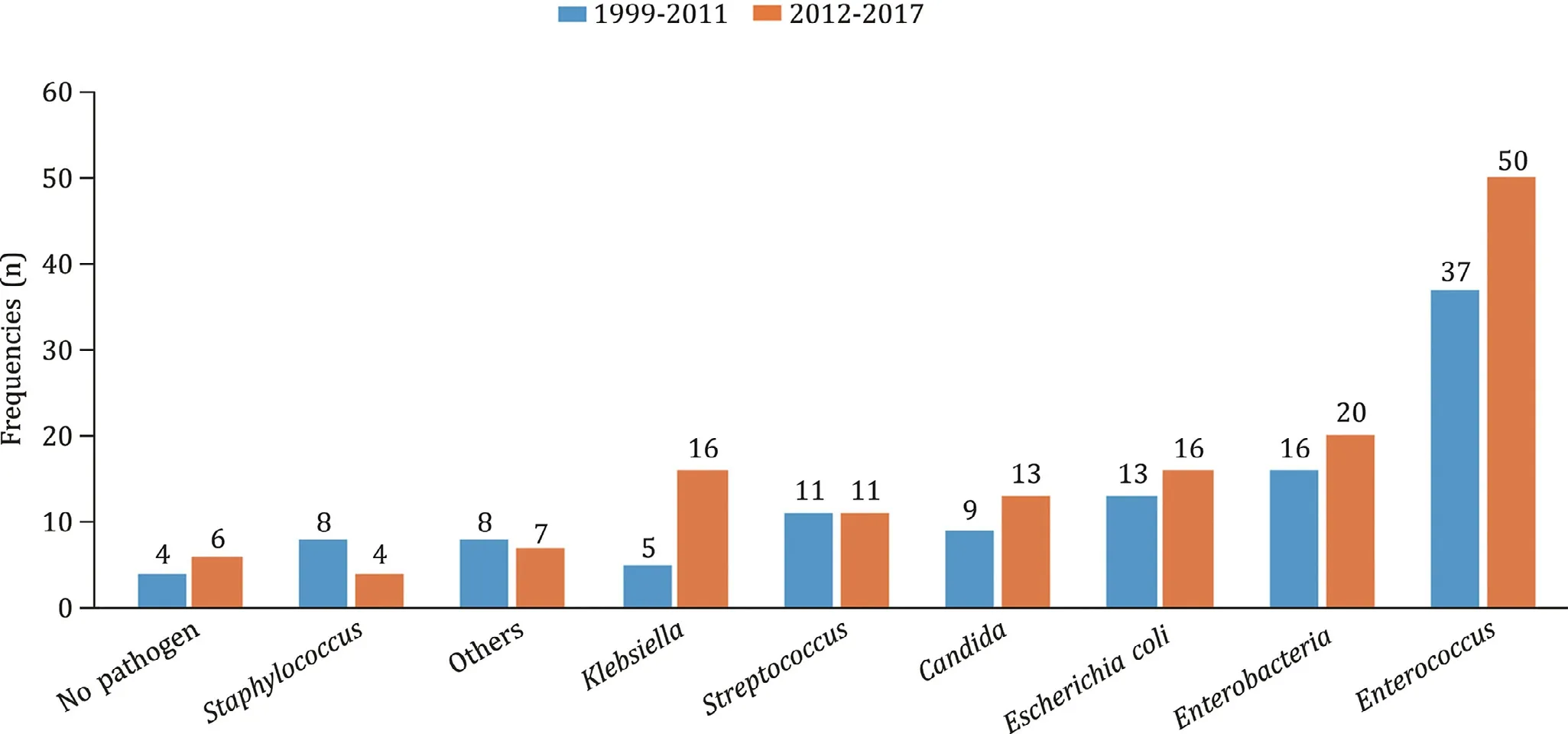
Fig. 6. Verification of the germ load divided based on the period of detection.
A comparison of the time intervals shows significant differences forEnterococcusfaeciumandKlebsiellaoxytoca. The pathogenEnte-rococcusfaeciumwas only detected in 16% of cases in the earlier period,but this value increased to 33% in the later period (P<0.05).Klebsiellaoxytocawas detected in only 4% of patients treated until 2011. In the later period,17% of the patient samples were colonized withKlebsiellaoxytoca(P<0.05). The frequencies ofEnte-rococcusfaecalis,EscherichiacoliandCandidaalbicansdid not differ significantly ( Table 1 ).
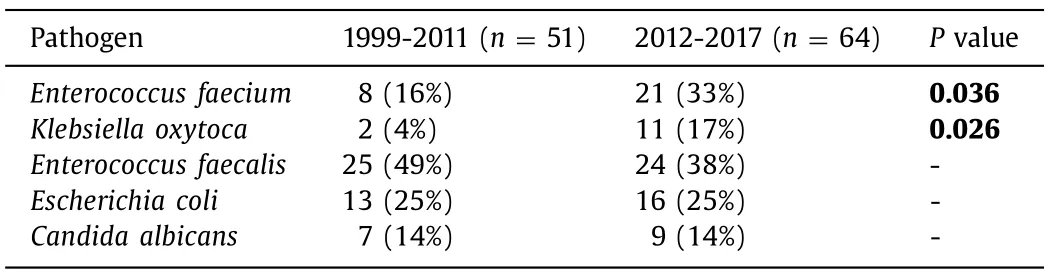
Table 1Percentage distribution of pathogen detections,according to time period (1999-2011 and 2012-2017).
The sensitivity ofEnterococcusfaecalisto vancomycin and ampicillin/sulbactam showed at 100% regardless of the study period.The sensitivity ofEnterococcusfaecalisto meropenem decreased from 28% in 1999-2011 to 0% in 2012-2017.
Sensitivity ofEnterococcusfaeciumto vancomycin showed about equivalent [75% (1999-2011) and 80% (2012-2017)]. Sensitivity to ampicillin/sulbactam showed very low in both periods (0% vs. 30%).Sensitivity ofEnterococcusfaeciumto meropenem showed at 0% in both periods studied.
For the pathogenKlebsiellaoxytoca,improved sensitivity values were observed for ampicillin/sulbactam (0% vs. 70%) and piperacillin/tazobactam (50% vs. 80%) in the later period. No changes in sensitivity levels were observed for cefotaxime (100%vs. 90%),meropenem nor ciprofloxacin (both 100%).
When considering the pathogenEscherichiacoli,all antibiotics tested showed improved sensitivity in the later period:ampicillin/sulbactam (46% vs. 67%),piperacillin/tazobactam (46%vs. 80%),cefuroxime (58% vs. 100%),cefotaxime (0% vs. 87%),and ciprofloxacin (46% vs. 80%).Escherichiacoliappeared to be well sensitive only to meropenem in both time periods (92%vs. 100%).
Discussion
The aim of our study was to investigate the bacteria present and the resistance situation for antibiotics/antimycotics of pCCC patients and to potentially improve perioperative treatment with the administration of an adequate antibiotic in this highly specialized patient cohort.
Vancomycin was the only antibiotic that demonstrated sensitivity in the majority of pCCC patients withEnterococcusfaeciumandEnterococcusfaecalisin our cohort. The agents ciprofloxacin,meropenem and cefotaxime showed 100% sensitivity againstKleb-siellaoxytoca. Meropenem showed very good coverage for the pathogenEscherichiacoli. Thus,the combination of meropenem and vancomycin appeared to provide optimal coverage against the most common pathogens in the patients studied. pCCCs can only be curatively treated through radical surgery,which is often associated with significant parenchymal loss of the liver. Postoperatively,this can lead to a small-for-size syndrome due to low future remnant liver volume,requiring patients to remain hospitalized for longer periods of time. Chen et al. [15] also observed this circumstance. For patients with complications,surgery typically requires a long hospital stay,delayed antineoplastic therapy,and a high economic burden.
Preoperative conditioning for pCCC patients is essential to minimize the risk of postoperative complications. In addition to portal vein embolization,biliary drainage also plays an important role.Currently,the use of preoperative biliary drainage in jaundiced patients remains one of the most debated issues [ 5,16 ].
A meta-analysis performed by Teng et al. [9] demonstrated that preoperative biliary drainage is associated with a greater risk of several types of infection and morbidities,but its ability to reduce postoperative hepatic insufficiency cannot be ignored. Nevertheless,biliary drainage is indicated for patients with cholangitis,hyperbilirubinemia-induced malnutrition,and hepatic insufficiency and for patients undergoing preoperative antineoplastic therapy or portal vein embolization [17] .
We showed thatEnterococciconstitutes the leading bacterial genus. This finding can be explained mainly by the interventions of endoscopic retrograde cholangiopancreatography (ERCP) and the deactivation of the natural barrier of the sphincter of Oddi with the stent in place [18] . Only a small proportion of patients without intervention had a colonized bile duct,and colonization was significantly more common in patients who underwent biliary interventions.
Overall,surgery for pCCC is associated with high complication rates mainly due to liver resection in a compromised organ.Therefore,preoperative conditioning of patients at all levels is favored. Treatment of cholangitis should also play a role because patients with preoperative cholangitis have significantly reduced overall survival [19] . In addition to overall survival,Sakata et al. [3] demonstrated that the perioperative use of appropriate antibiotics is an effective practice that reduces the incidences of surgical site infection and subsequent in-hospital mortality.Wang et al. [19] demonstrated that preoperative cholangitis was closely associated with increased risks of morbidity and mortality in patients with hilar cholangiocarcinoma,and that hepatic failure,infection,and sepsis were significantly increased in the preoperative cholangitis group. This was additionally illustrated by other colleagues who also observed a strong association with cholangitis and reported that preoperative cholangitis negatively affects postoperative infections,impairs the regenerative capacity of the liver,and increases the morbidity rate and postoperative hospital stay [20] .
A high proportion of bacteria resistant to penicillins was noted. Resistance to ampicillin-sulbactam,piperacillin-tazobactam,ciprofloxacin and imipenem has been observed by Scheufele et al. [21] .
We found that our perioperative standard antibiotic treatments(cefuroxime/metronidazole) do not seem to be useful in our cohort because resistance to these antibiotics can occur. If cephalosporinbased antibiotic regimens are favored,we believe that ceftriaxone should be prioritized.
Colonization withCandidaalbicanscan be explained by recurrent interventions,as Lübbert et al. and Gotthardt et al. have previously shown,given that risk factors for the presence ofCandidain the bile duct include biliary stenting,malignant strictures,and repeated interventions [ 22,23 ]. In our data,we observed a high sensitivity of the fungi to antimycotics. However,regular use of antifungal drugs in the presence of colonization is not necessary in our opinion given that fungal colonization of the bile ducts does not lead to candidemia. In addition,the literature also does not consider regular antifungal treatment in colonization,but treatment should be administered when patients may not respond to antibiotics and biliary drainage [24] .
One of the main points of consideration of the work was the question of whether tumor localization can have an influence on the pathogens and colonization of the bile. Chen et al. [15] demonstrated that the microbial spectrum of pCCC differs from that of distal biliary obstruction. In this regard,data already exist on pancreatic head carcinoma,but data on pCCC are limited. For example,Müssle et al. [25] highlighted that only a few studies mentioned a correlation between bacterobilia and the pathological tumor type.
One point that remains unclear is the fact thatEntero-coccusfaeciumandKlebsiellaoxytocawere detected more frequently in the time interval from 2012. Müssle et al. [25] considered that higher rate ofEnterococcusspecies might be due to biliary obstruction and the widespread use of endoscopic biliary stents. Another contributing factor could be the selection of microorganisms by the use of antibiotics. Bornscheuer et al. [26] reported that in view of the increasing number of multidrug-resistant Gram-negative bacteria andKlebsiellain the community,it should be noted that these organisms are not adequately covered by cephalosporins,penicillin derivatives,or fluoroquinolones.
Considering this point as well as the resistance situation,a broad antibiotic should be favored in pCCC patients who have already received a stent. In our opinion,a carbapenem (meropenem)in combination with vancomycin should be chosen to cover theEnterococcalgap [27] . This notion was also postulated by Bornscheuer and colleagues [26] . These scientists additionally reported thatEnterococcusis an important pathogen and therefore,vancomycin should be added in all cases of severe acute cholangitis [ 18,26 ].
Jethwa et al. [28] also demonstrated this for pCCC patients with percutaneous drainage and recommended that patients who are managed surgically should be treated with either vancomycin or teicoplanin. Gavazzi et al. [18] recommended that antibiotic prophylaxis in stented patients should include aβ-lactamase antibiotic active againstEnterococcusspp. [18] .
Overall,we recommend broad perioperative antibiotic therapy,which primarily coversEnterococci. Of course,it must also be noted that these antibiotics,i.e.,meropenem or vancomycin,are typically considered reserve therapies and therefore,they must be used with caution. However,Tanaka et al. [11] stated that broadspectrum antibiotics are more beneficial in patients at a high risk of surgical infection than second-generation cephalosporins.Scheufele et al. [21] also postulated that biliary drainage is associated with a more antibiotic-resistant bacteria in the bile,which may require changing the type of perioperative antibiotics used for prophylaxis or treatment. And as Okamura et al. [29] demonstrated,prophylactic administration of therapeutic antibiotics is reasonable; however,preoperative biliary culture samples should be used if available.
Regional differences exist in the microbial counts and in the resistograms [14] . The differences must be considered when selecting antibiotics,as theEnterococcalgap must always be addressed in this patient population with recurrent biliary tract interventions.
One limitation of this study is the fact that the duration of antibiosis was not investigated. Thus,further work is necessary to shed light on the duration of this propagated antibiosis. Does the perioperative single shot provide a significantly better effect? Is continued antibiosis beyond the time of surgery associated with an improvement in the outcome of these patients? Further work is needed to improve the treatment of this special patient category at any level. Given that Wang et al. [19] demonstrated that cholangitis directly affects the outcomes after radical resection in pCCC patients,effective strategies should be implemented to reduce the risk of preoperative cholangitis and improve the prognosis of pCCC patients.
Continuing work, especially studies regarding the pre/perioperative conditioning in pCCC,must be the goal of further research. We agree with the statement of other authors who clarified that preoperative cholangitis remains a major determinant of outcomes in pCCC,and we believe that prospective studies are needed to optimize the preoperative approach in these patients to minimize the risks of postoperative liver failure [30] .
In conclusion,our study contributes a small part to the clarification,and we are of the opinion that given germ load of this patient population,perioperative antibiosis with meropenem and vancomycin has to be considered reasonable,especially in patients in whom biliary decompression has already occurred.
Acknowledgments
None.
CRediT authorship contribution statement
FelixDondorf:Conceptualization,Data curation,Formal analysis,Investigation,Methodology,Writing - original draft,Writing -review & editing.MaximilianGraf:Data curation,Formal analysis,Investigation,Methodology,Resources.AladdinAliDeeb:Data curation,Investigation,Validation.OliverRohland:Conceptualization,Formal analysis,Investigation,Validation.PhilippFelgendreff:Data curation,Investigation,Validation,Visualization.Michael Ardelt:Data curation,Investigation,Validation.UtzSettmacher:Conceptualization,Data curation,Methodology,Project administration,Supervision.FalkRauchfuss:Conceptualization,Formal analysis,Project administration,Supervision,Writing - original draft.
Funding
None.
Ethical approval
This study was approved by the Ethics Committee of Jena University Hospital (No. 2021-2204-data).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年5期
Hepatobiliary & Pancreatic Diseases International2023年5期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Right hepatectomy with a cholangiojejunostomy and hepaticojejunostomy for unilobar Caroli’s syndrome
- Total three-dimensional laparoscopic radical resection for Bismuth type IV hilar cholangiocarcinoma
- A surgical technique using the gastroepiploic vein for portal inflow restoration in living donor liver transplantation in a patient with diffuse portomesenteric thrombosis
- Full laparoscopic anatomical liver segment VII resection with preferred Glissonean pedicle and dorsal hepatic approach
- Combined hepatic segment color rendering technique improves the outcome of anatomical hepatectomy in patients with hepatocellular carcinoma
- Targeting mitochondrial transcription factor A sensitizes pancreatic cancer cell to gemcitabine
