Increased incidence of indeterminate pancreatic cysts and changes of management pattern: Evidence from nationwide data
Jewoo Prk , , Jinkyeong Prk , , Yoon Suk Lee , Kwngrok Jung , In Ho Jung ,Jong-Chn Lee , Jin-Hyeok Hwng , Jihwn Kim ,
a Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
b Department of Internal Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea
cDepartment of Internal Medicine, Inje University College of Medicine, Ilsan Paik Hospital, Goyang, Korea
ARTICLE INFO Article history:Received 12 November 2021 Accepted 10 May 2022 Available online 7 June 2022
Keywords:Pancreatic cyst Incidence Prevalence Pancreatectomy Big data
ABSTRACT Background: Pancreatic cysts are common. However, most studies are based on data collected from individual centers. The present study aimed to evaluate the changes of management patterns for pancreatic cystic lesions (PCLs) by analyzing large epidemiologic data.Methods: Between January 2007 and December 2018, information regarding pancreatic cystic lesions was acquired from the nationwide Health Insurance Review and Assessment Service database in Korea.Results: The final number of patients with pancreatic cysts was 165 277 among the total claims for reimbursement of 855 983 associated with PCLs over 12 years. The total number of claims were increased from 19 453 in 2007 to 155 842 in 2018 and the prevalence increased from 0.04% to 0.23%. For 12 years,2874 (1.7%) had pancreatic cancer and 8212 (5.0%) underwent surgery, and 36 had surgery for twice (total 8248 pancreatectomy). After ruling out claims from the first 3 years of washout period, the incidence increased from 9891 to 24 651 and the crude incidence rate of PCLs expanded from 19.96 per 10 0 0 0 0 to 47.77 per 100 000. Compared to specific neoplasm codes (D136 or D377), the use of pancreatic cyst code (K862) has been remarkably increased and the most common since 2010. The annual number of pancreatectomies increased from 518 to 861 between 2007 and 2012, and decreased to 596 until 2018.The percentage of pancreatic cancer in patients who received pancreatectomy increased from 5.6% in 2007 to 11.7% in 2018.Conclusions: The incidence of PCLs is rapidly increasing. Among PCLs, indeterminate cyst is increasing outstandingly. A trend of decreasing in the number of resections and increasing cancer rates among resected cysts may be attributed to the updated international guidelines.
Introduction
Pancreatic cystic lesions (PCLs) are clinically significant due to the potential of malignant transformation. They present with several subtypes and the risks of malignant transformation are different for each subtype [1] . It is difficult to confirm the exact subtype of most PCLs without a biopsy or resection and most PCLs are diagnosed based on their radiological appearance [2] . As a result,life-long surveillance is warranted in most PCLs without resection.
However, the incidentally found PCL is rapidly increasing because of an increase in the aging population and the widespread use of cross-sectional imaging [3] . Moreover, the prevalence was dissimilar in various studies. PCLs were identified in 2.6% outpatient population from a study with computed tomography (CT)scans [4] . They were more commonly detected on magnetic resonance imaging (MRI). The incidence ranged from 13.5% to 19.6%in consecutive patients who had abdominal MRI [ 5 , 6 ]. PCLs were discovered in approximately 24.3% of the autopsies after deaths in elderly people [7] . This large discrepancy between the studies is due to the different sensitivity of the detection modalities for PCLs.
In spite of surveillance strategies for presumed risks of malignant transformation of PCLs, there is no consensus about the surveillance interval and the screening modalities [8-10] . However, a recent study emphasized that the results of the lessintensive strategy were comparable to the more-intensive one and the less-intensive strategy costs much lower if the projected rate of malignant transformation of the pancreatic cysts is low (0.12%annually) [11] . According to this study, the potential rate of malignant transformation is the most critical parameter in deciding the strategy, and the prevalence of PCLs turns out to be an important factor because it functions as a denominator for calculating the rate of malignant transformation. However, large-scale studies are limited although there have been a few cohort studies that analyzed more than 10 0 0 0 patients with PCLs [ 3 , 12 ].
In Korea, there is a single national insurer called the National Health Insurance Service, and most medical cost claims are reviewed by the Health Insurance Review and Assessment (HIRA)Service. As a result, there is an easy access to the claim records of the whole population through the HIRA dataset. Therefore, it is feasible to assess nationwide epidemiological data about PCLs by using the diagnostic codes utilized in the medical claims. Herein,we aimed to assess the changing management patterns for patients with PCLs in recent years using a nationwide medical claim database.
Methods
Dataset
Between January 2007 and December 2018 the public data regarding pancreatic cysts were acquired from the HIRA database.For extraction of data about patients with PCLs, the disease or procedural codes of the Korean Standard Classification of Diseases version 6 (KCD-6) were used. KCD-6 is the Korean version of the International Classification of Diseases version 10 (ICD-10), and all the disease and procedural codes found in the KCD-6 and used in this study are exactly the same as those in the ICD-10. The disease codes of the different pancreatic cysts are presented in Table 1 . All claims that had the KCD codes ( Table 1 ) as the primary diagnosis or the secondary diagnosis were collected to collate all possible cases. Similarly, codes regarding pancreatic surgery were collected,too ( Table 2 ).

Table 1 Disease codes about pancreatic cyst.
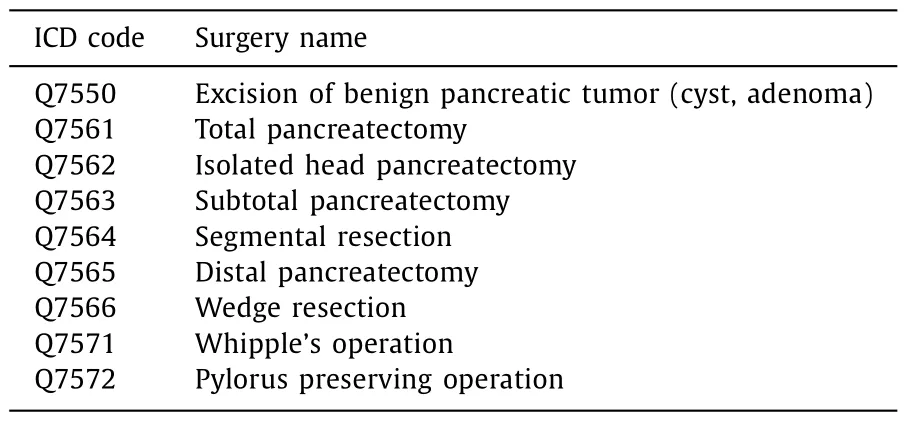
Table 2 Codes of pancreatic surgery.
The HIRA dataset consists of five tables. Among these, three tables were acquired in this study: the table with general information (table 20) containing demographic data such as sex, age,and indicators for inpatient and outpatient services; the table with specific information on services provided (table 30); and the table with diagnostic information (table 40). The key codes for each table were unique and connected the tables.
Washout period and census data
The incidence of pancreatic cyst was calculated at the first time of diagnosis. Patients diagnosed during the initial three years (between 2007 and 2009) were excluded as this duration was considered the “washout period”. To estimate the prevalence and agestandardized incidence rates, the annual population and census data in 2010 and 2015 were acquired from the Korean Statistical Information Service. The Department for Population and Housing Census of Korea conducts a survey once every five years. After excluding the three-year washout period, the 2010 and 2015 population censuses were used to calculate the age-standardized incidence rates between 2010 and 2014, and 2015 and 2018, respectively.
Operational definition of pancreatic cancer
Pancreatic cancer was defined using ICD-10 code C25.x. Among them, only patients supported by the national aid program (V193)for critical and rare diseases were considered to be patients with pancreatic cancer. Currently, this special program supports patients with rare incurable diseases or cancer to lessen the burden of medical costs on these patients. Because the C25 code was used to record patients who were suspected to have pancreatic cancer regardless of true malignancy, a combination of codes C25 and V193,which is unique to Korea, was used to define pancreatic cancer.
Finally, patients with pancreatic cancer were defined in this study in the following manner: (1) patients with definite pancreatic cancer - those who had codes C25 as the primary diagnosis and V193, without claims for any other cancer; (2) patients with possible pancreatic cancer - those who had codes C25 as the primary diagnosis and V193, with claims for other cancer.
In these patients with definite or possible pancreatic cancer, the date of diagnosis of pancreatic cancer was defined as the first date on which the medical claim was made with the code C25. If code C25 was identified only as the secondary diagnosis, and not as the primary diagnosis, they were regarded as not having pancreatic cancer for the purpose of this study, even if they had code V193.
Statistical analysis
Student’st-test and Chi-square test were used for continuous and categorical data, respectively. The prevalence rate is defined as the proportion of the number of patients with a specified PCL code to the population in the same year. The crude incidence is defined as the number of patients with a newly developed PCL code that had not been diagnosed in the preceding three years(considered the “washout period”). The age-standardized incidence rate is defined as the proportion of crude incidence in groups categorized based on 10-year increments of age per 10 0 0 0 0 population of the same age group. All tests were two-sided, andPvalues<0.05 were considered statistically significant. All analyses were performed and plots were drawn using R software version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Number of patients with pancreatic cysts, pancreatic surgery and pancreatic cancer
Between 2007 and 2018, there were 690 657 claims with pancreatic cysts codes as their primary diagnosis and 239 293 claims with the codes as their secondary diagnosis. After removal of duplicated cases that had the pancreatic cyst codes in both the primary and the secondary diagnoses, a total of 855 983 claims in 165 277 patients were eventually identified to be related with pancreatic cysts ( Fig. 1 ). During the first clinic visit, the mean age of patients was 59.7 ± 14.0 years and the ratio of males to females was 0.81 (73 815/91 462) for 12 years.
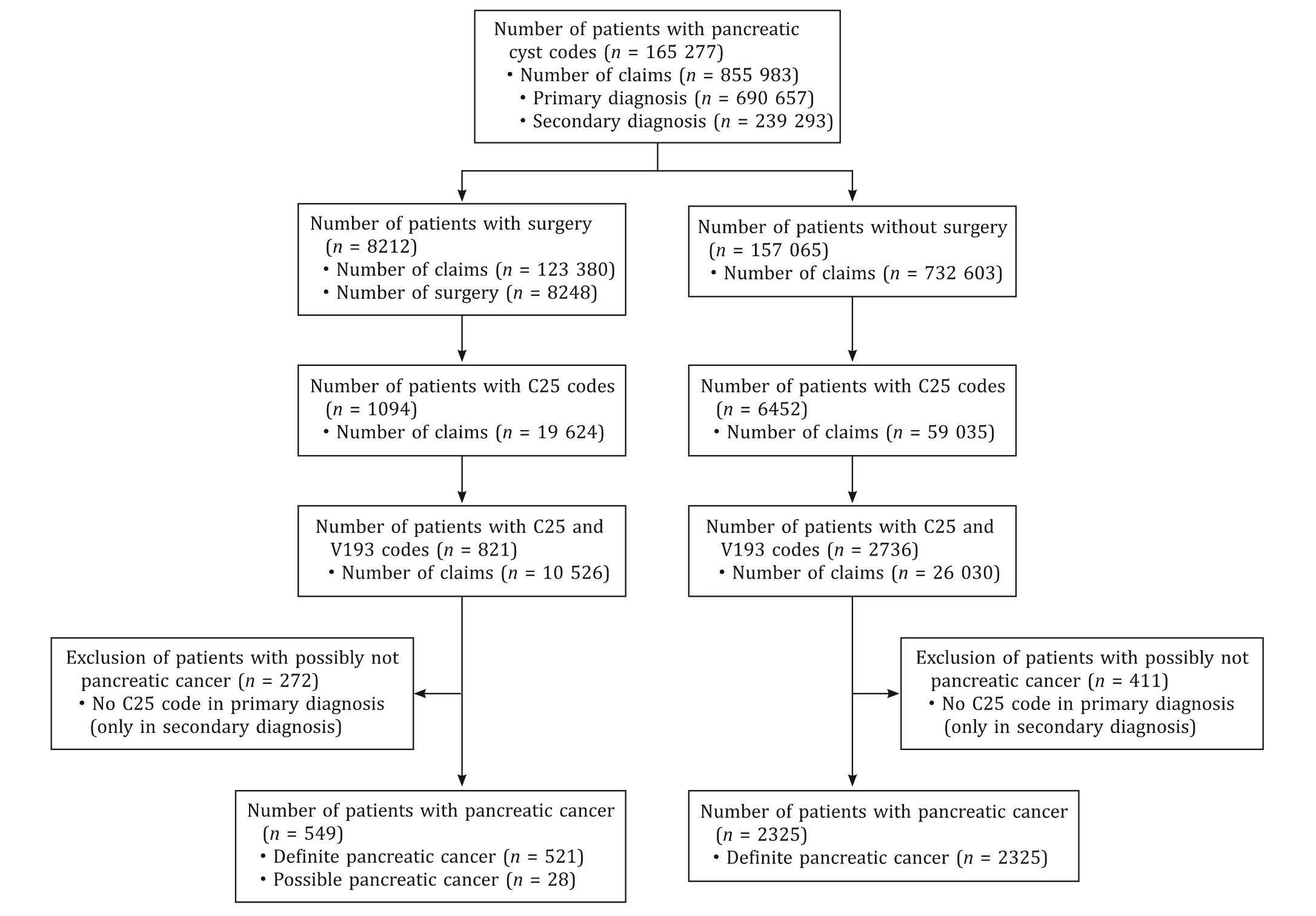
Fig. 1. Flow chart of the study.
Of these, 8212 patients (5.0%) underwent pancreatectomy within the 12-year period, and 36 underwent surgery for twice(total 8248 pancreatectomies). Among 8212 patients who received pancreatic surgery, 1094 had code C25 in their 19 624 claims, and 821 patients had both codes C25 and V193 in their 10 526 claims.There were 521 patients with definite pancreatic cancer, and 28 with possible pancreatic cancer. Therefore, a total of 549 patients(6.7%) were regarded as having pancreatic cancer, and 272 patients were regarded as not having pancreatic cancer because code C25 was identified only as the secondary diagnosis. Of the 157 065 patients who did not receive pancreatic surgery, 6452 had code C25 in their 59 035 claims and 2736 had both codes C25 and V193 in their 26 030 claims. Of these, a total of 2325 (1.5%) were regarded as having pancreatic cancer, and 411 not having pancreatic cancer,as code C25 was identified only as the secondary diagnosis. Therefore, a total of 2874 patients (1.7%) were defined as having pancreatic cancer, and there was a significant difference in the frequency of pancreatic cancer between patients with and without resection(6.7% vs. 1.5%,P<0.001).
The number of medical claims
The total number of claims for any of the 5 pancreatic cyst codes were increased from 19 453 in 2007 to 155 842 in 2018. A total of 138 092 patients were newly diagnosed to have pancreatic cysts in 9 years (2010-2018) and the incidence of pancreatic cyst increased from 9891 to 24 651 ( Fig. 2 ). The prevalence of PCLs was risen from 0.04% in 2007 to 0.23% in 2018 and the crude incidence from 19.96 per 100 000 to 47.77 per 100 000 population between 2010 and 2018 ( Table 3 ).
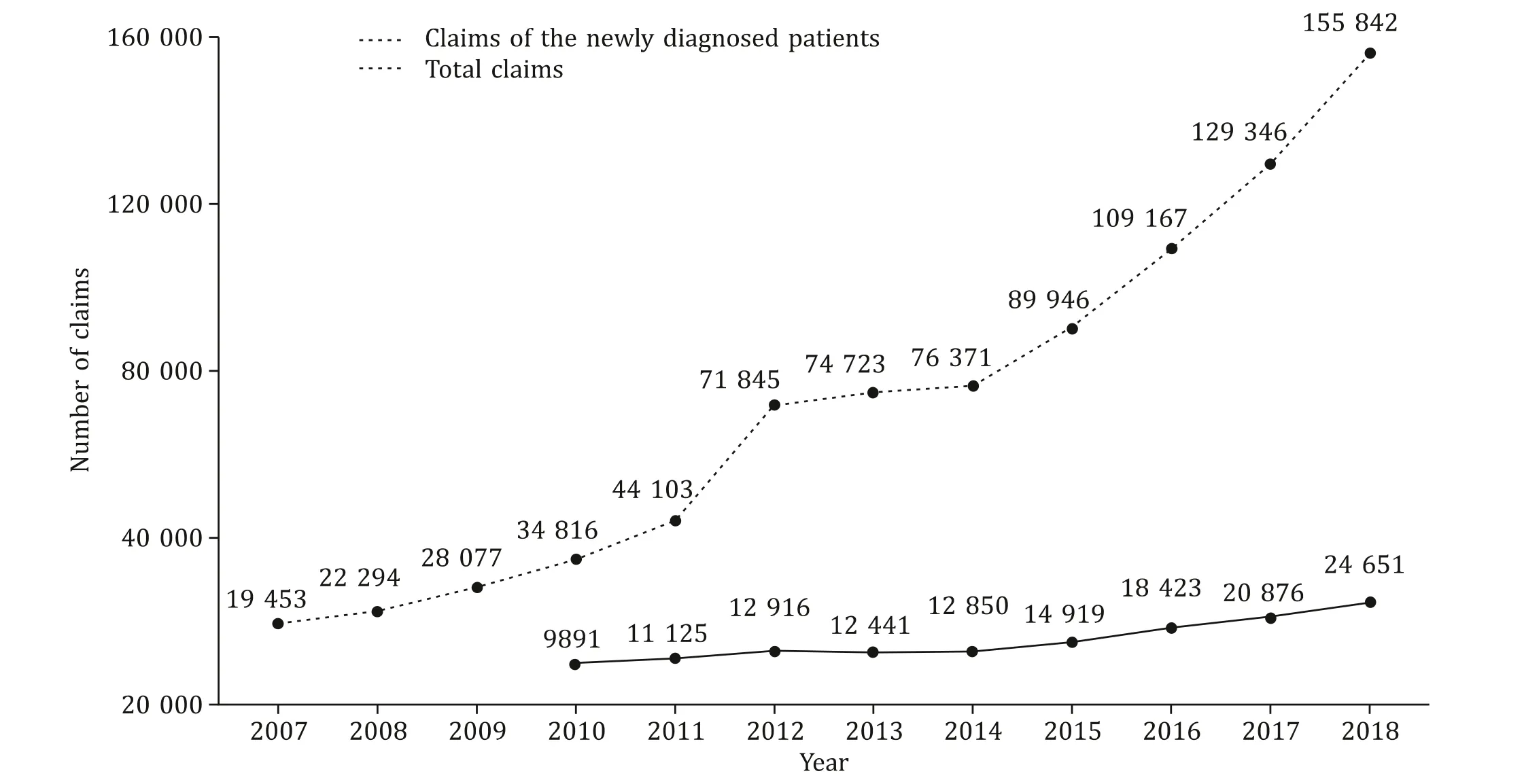
Fig. 2. The total number of claims including those in newly diagnosed patients during the study period. The total claims for five pancreatic cyst codes were rapidly increased from 19 453 to 155 842 between 2007 and 2018. After a washout period for three years, the incidence of newly diagnosed pancreatic cysts also increased from 9891 to 24 651 between 2010 and 2018.
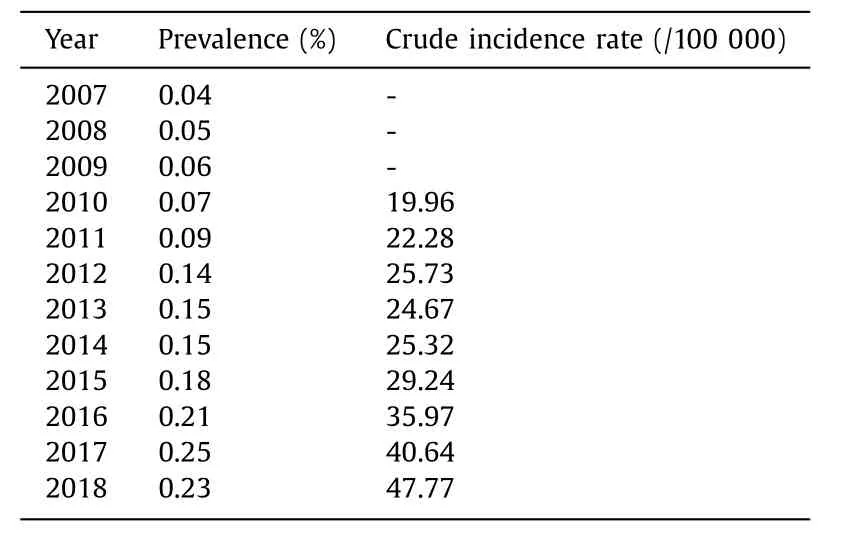
Table 3 Population adjusted prevalence and incidence of pancreatic cysts.
Among the number of claims with cystic codes in the primary diagnosis, the claims with D136 (benign neoplasm of pancreas),D377 [neoplasm of uncertain or unknown behavior of other digestive organs (anus not otherwise specified, intestine not otherwise specified, esophagus, pancreas)], and K862 (cyst of pancreas) revealed a rapid increase ( Fig. 3 ). Among these, K862 was the second most common in 2007. However, it ranked to the most common code since 2010. D136 ranked from the most common in 2007 to the second most common code since 2010. The claims with K863(pseudocyst of pancreas) displayed a slight increase from 1541 to 3053. However, those with the code D017 (carcinomainsituof pancreas) were negligible.
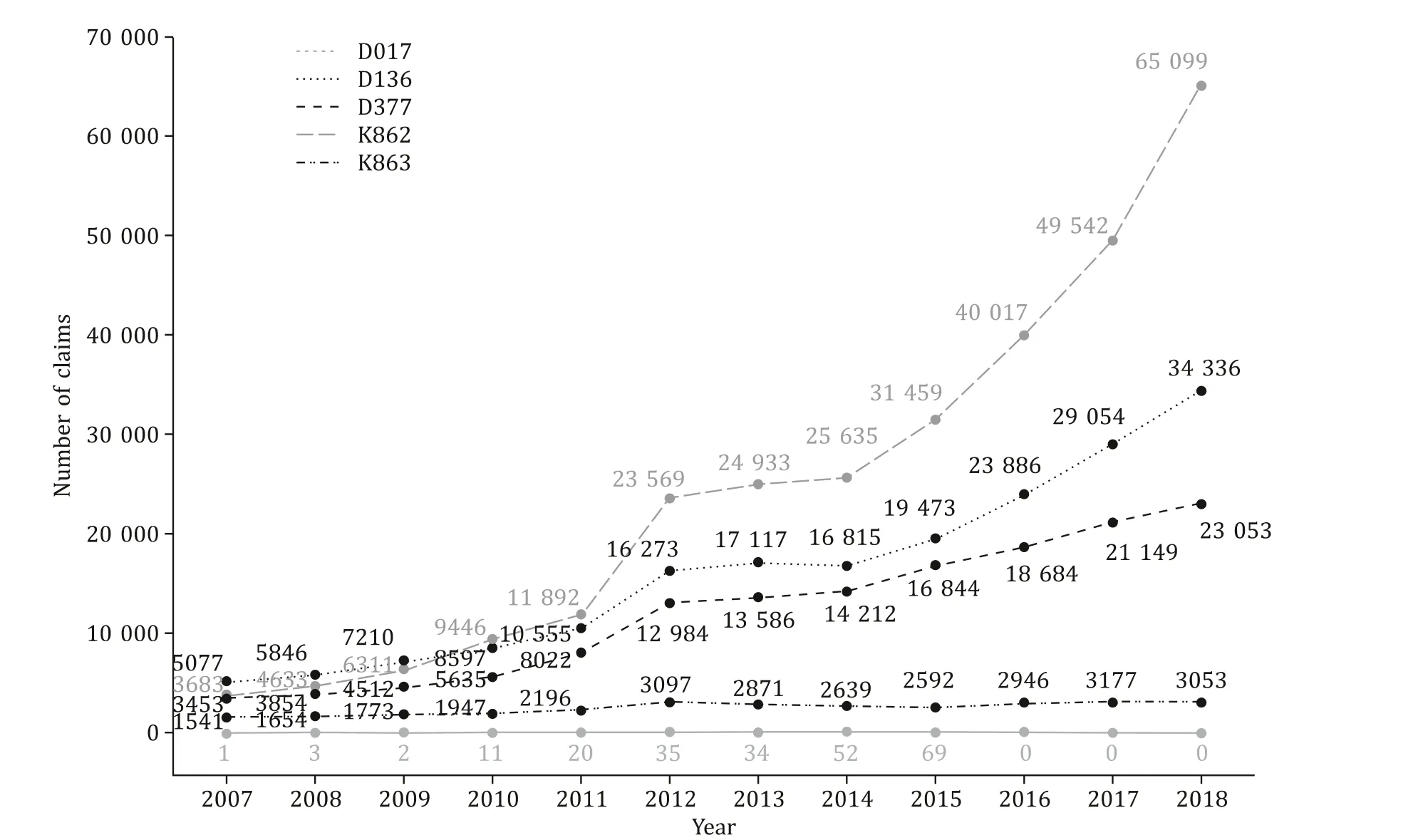
Fig. 3. The incidence of pancreatic cysts categorized based on the disease code.Among five different codes for pancreatic cyst, K862 (cyst of pancreas) was the most common code followed by D136 (benign neoplasms of pancreas) and D377 (neoplasms of uncertain or unknown behavior of other digestive organs).
Newly diagnosed patients with pancreatic cysts
Among the 138 092 patients with newly diagnosed pancreatic cysts, the mean age was 60.3 ± 13.8 years. The incidence of PCLs was more common in females than in males (77 334/60 758), and the annual sex ratio of males to females exhibited a continuous decrease from 0.86 to 0.69 ( Fig. 4 ).
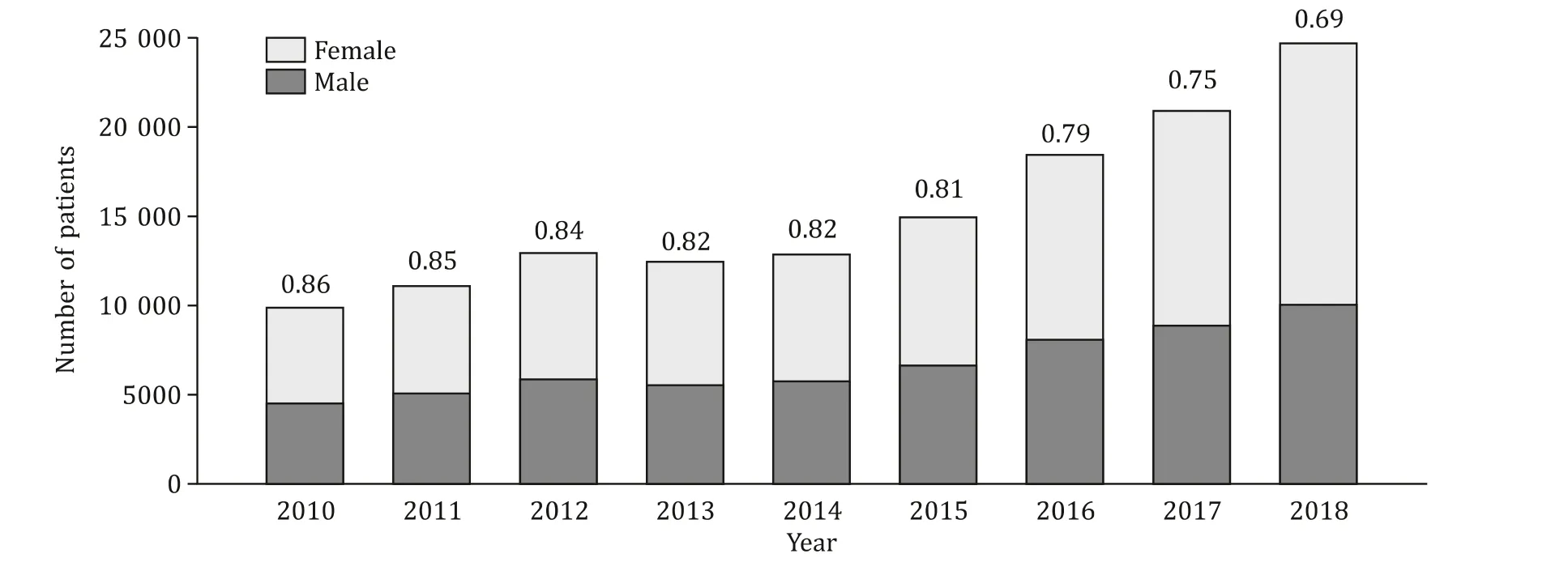
Fig. 4. Incidence of pancreatic cysts when classified based on the sex. The incidence of pancreatic cysts was more common in females and a decrease from 0.86 to 0.69 was noted in the ratio of males to females between 2010 and 2018.
The patients aged>60 years had the highest incidence followed by those in their 50s ( Fig. 5 A). Patients in their 70s had the highest age-standardized incidence rate (182.6 per 100 000) followed by those in their 60s and 80s (148.0 per 100 000 and 141.8 per 100 000) in 2018 ( Fig. 5 B).
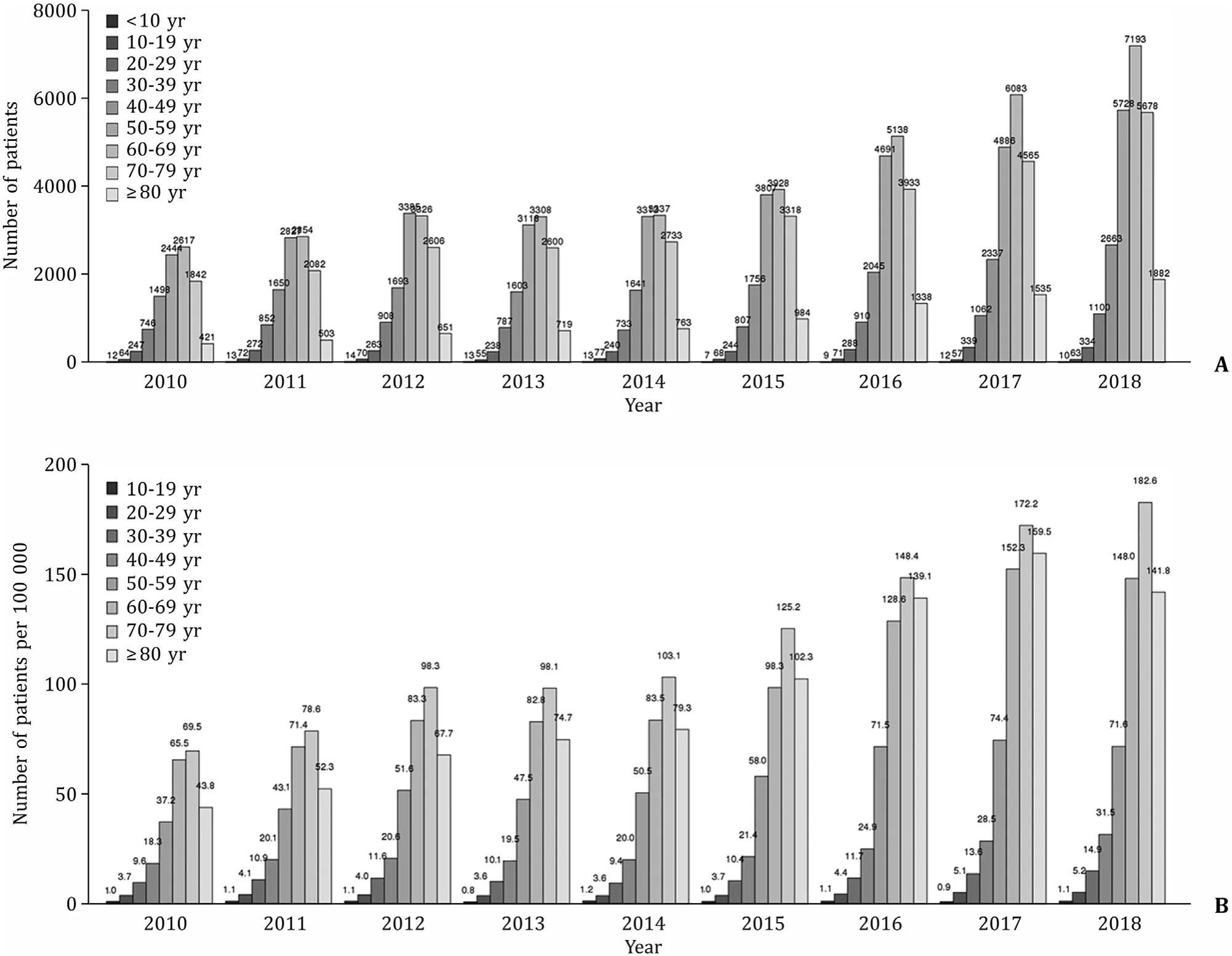
Fig. 5. Incidence of pancreatic cysts when classified based on the age. A: The crude incidence of pancreatic cysts was highest among patients in their 60s, when participants were classified according to 10-year increments in age. B: Age-standardized incidence rates were highest among those in their 70s followed by those in their 60s and 80s.
Number of surgery and percentage of pancreatic cancer over pancreatectomy
Of the 8248 cases of resection, the number of pancreatectomies increased from 518 to 861 between 2007 and 2012, and decreased to 596 until 2018 ( Fig. 6 A). The percentage of pancreatectomy compared with the total medical claims continually decreased from 2.7% to 0.4%. The percentage of pancreatic cancer over pancreatectomy increased from 5.6% in 2007 to 11.7% in 2018( Fig. 6 B).
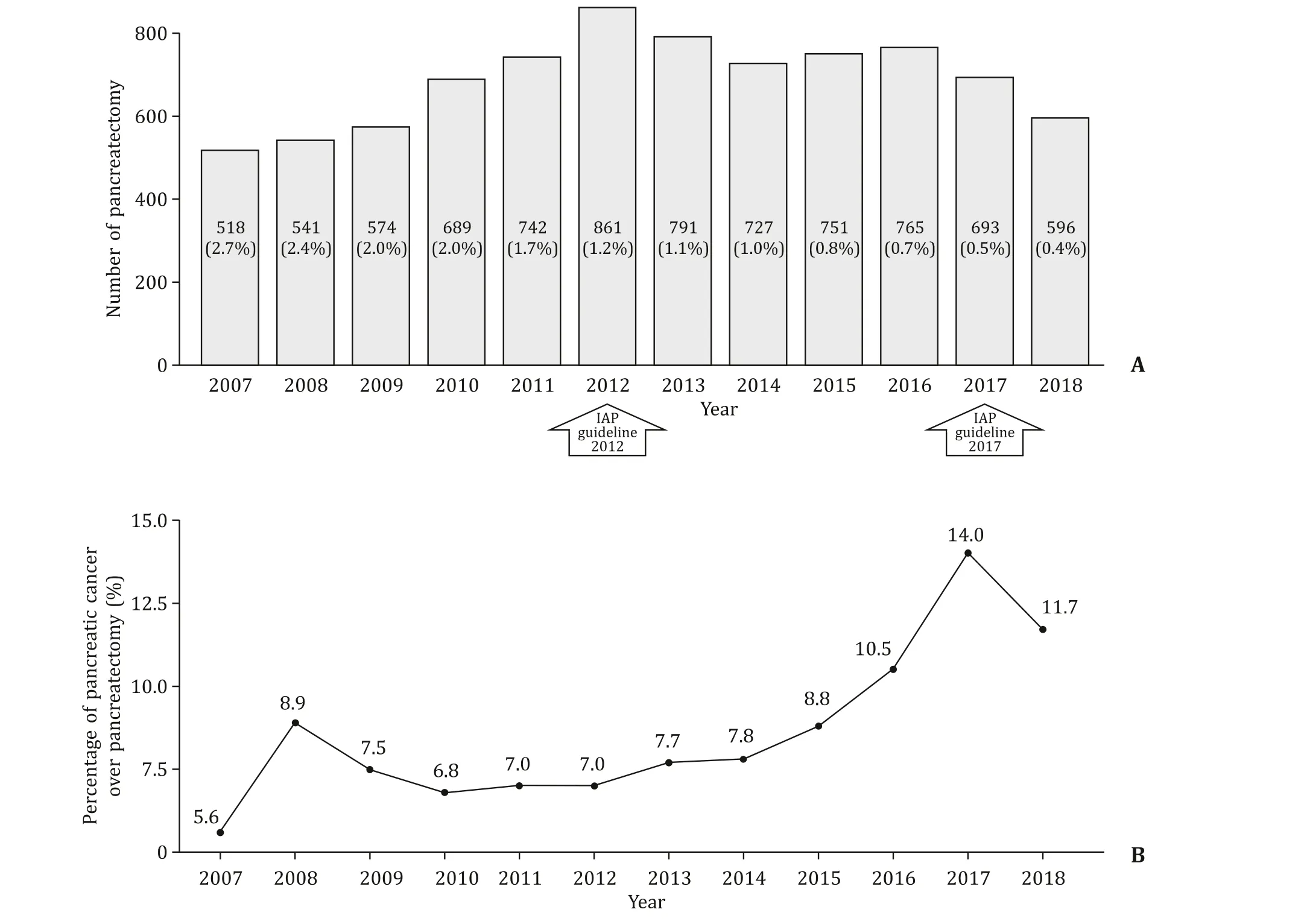
Fig. 6. Number of pancreatectomies and percentage of pancreatic cancer over pancreatectomy. A: The number of surgical resections increased from 518 to 861 between 2007 and 2012, then decreased to 596 between 2012 and 2018. Compared to the number of resections, the rate of resection continuously decreased from 2.7% to 0.4% of the patients with PCLs. International Association of Pancreatology (IAP) Consensus Guidelines 2012 and 2017 were marked as arrows. B: The rate of pancreatic cancer in those who received resection increased from 5.6% to 11.7%. PCL: pancreatic cystic lesion.
Discussion
PCLs are relatively common and comprise a heterogenous group of pancreatic diseases. Although they have a potential risk of malignant transformation according to the subtype, about 70% of PCLs are discovered incidentally [13] . In Korea, a study was conducted for the purpose of health screening using CT scans, which reported a crude prevalence rate of 2.1% [3] . In a prospective populationbased study using MRI in Germany, the baseline prevalence was 49.1% which was comparable to the findings obtained in an autopsy study [14] and the weighted incidence of newly detected pancreatic cysts was 12.9% [15] . The higher prevalence when diagnosed using MRI could be due to its excellent tissue contrast using T2-weighted sequence for evaluating cystic contents when compared to CT [16] .
In the current study, the prevalence and incidence were much lower than those in other studies. The crude prevalence was much higher (2.1%) among a population in a previous large-scale Korean study that underwent health screening using abdominal CT [3] ,than in the current study (0.23% in 2018). This difference can be explained by the omission of axial imaging and the inclusion of younger patients who have lesser PCLs than the elderly [17] . However, it is important to note that in our study the incidence increased by 2.5 times in 9 years and the prevalence increased by 6 times in 12 years. Considering the rise of the aging population and the more widespread use of axial imaging, the incidence of PCLs tends to increase in the near future. Consequently, the risk of malignant transformation might be lower than the current estimation because of an increase in the diagnosis of low-risk small PCLs and a slow evolution of small benign cysts [ 3 , 18 ].
A recent model-based cohort study proposed the clinical implications of the American Gastroenterological Association (AGA)guidelines in 2015 [ 8 , 11 ]. According to their model, a moreintensive surveillance strategy would be offset by a greater number of surgical deaths and higher cost due to the estimated low rate of malignant transformation (0.12% per year). In this nationwide study, pancreatic cancer was diagnosed in 1.74% of pancreatic cyst during the 12-year study period. Considering the possibility of incidental PCLs when pancreatic cancer was diagnosed, the actual risk of pancreatic cancer originating from PCLs in the general population might be much lower, which is very similar to the estimated rate in a model-based cohort study [11] . Consequently, the current study supports this recent systematic model-based study,which suggested a less-intensive surveillance strategy.
In this study, the most common disease code in the medical claims was K862 (cyst of pancreas), which was two times more prevalent than the second common disease code D136 (benign neoplasm of pancreas). Considering that codes D136 and D377 correspond to specific subtypes of PCLs, we believe that most clinicians prefer to use the general disease code instead of the specific designation. It may also reflect the difficulty in diagnosing PCLs accurately, especially when they are very small.
It is also well-known that PCLs are far more common in the elderly [ 3 , 5 , 7 , 15 , 17 ]. In our study, the age-standardized incidence rates were highest in those aged>70 years (around 182.6 per 10 0 0 0 0). The incidence rates among those in their 60s, 70s, and>80s were more than two, four, and eight times of the rates among those in their 50s, 40s, and 30s, respectively in 2018. The incidence rates of those in their 10s and 20s were 1.1 per 100 000 and 5.2 per 100 000 population, respectively.
The data from previous studies were inconsistent with regard to the difference in prevalence rates between males and females. Although some studies reported no differences between the two sexes [ 4 , 17 ], other studies reported a female predominance[12-14] . Our study also showed that PCLs were more common in females than in males and the ratio of males to females revealed a decreasing trend. The cause for female predominance is not clear. However, female predominance in other cystic lesions such as serous cystic neoplasms, solid pseudopapillary neoplasms,and mucinous cystic neoplasms [19] and the longer life expectancy among females in Korea (86.3 years in females vs. 80.3 years in males in 2019) could explain this variance [20] .
In this study, the number of pancreatectomies increased until 2012 and decreased thereafter. However, the rate of pancreatectomies among patients with PCLs continuously decreased. The decreasing trend in the number of resections may be attributed to the 2012 updated international guidelines [ 9 , 21 ]. Another recent multicenter study also reported a decreasing rate of surgery based on the international guidelines [22] . However, the present study showed an improvement in the prediction of cancer, from 5.6%to 14.0%, contrary to the previous study that showed a decreasing rate of high-risk disease [22] . Although it is assumed that the more conservative approach based on improved imaging test and knowledge about PCLs have influenced the improved outcomes in this study, more studies are necessary to validate this hypothesis.
There were several limitations. First, we did not classify the subtypes of PCLs because we did not access patient-level medical data. It is possible that the radiological diagnosis of PCLs could be inconsistent with the pathological diagnosis. Furthermore, this study demonstrated that indeterminate pancreas cyst has become a tremendous proportion of the entire disease population of PCLs.Therefore, the implication of our study is that future guidelines should be better established considering the indeterminate entity of PCLs, which has been reflected at a certain point by AGA guidelines [8] . Second, this study could not discriminate the pancreatectomy for pancreatic cancer derived PCLs from that for pancreatic cancer concomitant PCLs. Therefore, there is the possibility of incidental PCLs at diagnosis of pancreatic cancer. Finally, the crude incidence and prevalence rates are much lower than those in other studies. Since most PCLs are incidentally found on axial imaging(CT) that was performed for unrelated causes, there is a possibility that their incidence was underestimated without performing tests in the population in this study. However, the current study has the strength of nationwide ascertainment of the rapidly increasing trend of PCLs and provides a glimpse of the epidemiological trends about PCLs in Korea. In addition, National Health Insurance Service had expanded insurance coverage to include pancreas MRI for pancreas cystic lesions since November, 2019 in need of further nationwide epidemiologic study in near future to compare with the current study.
In conclusion, we observed a rapid increase in the crude incidence and prevalence rates of PCLs. In addition, indeterminate cyst, but not neoplastic cyst, is tremendously increasing according to the nationwide dataset. The updated 2012 international guidelines may attribute to decreasing trend in the number of resections and increasing cancer rates among resected cysts. It is necessary to investigate with a less-intensive surveillance strategy and a more precise preoperative diagnosis.
Acknowledgments
This study used HIRA research data (M20190807904) made by Health Insurance Review & Assessment Service(HIRA). The views expressed are those of the author(s) and not necessarily those of the HIRA and the MOHW.
CRediTauthorshipcontributionstatement
JaewooPark:Conceptualization, Data curation, Formal analysis, Writing - original draft, Writing - review & editing.Jinkyeong Park:Conceptualization, Data curation, Formal analysis, Writing -original draft, Writing - review & editing.YoonSukLee:Data curation, Formal analysis, Writing - review & editing.KwangrokJung:Writing - review & editing.InHoJung:Writing - review & editing.Jong-ChanLee:Writing - review & editing.Jin-HyeokHwang:Writing - review & editing.JaihwanKim:Conceptualization, Data curation, Formal analysis, Investigation, Supervision, Writing - original draft, Writing - review & editing.
Funding
None.
Ethicalapproval
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital. Written informed consent was obtained from all participants.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年3期
Hepatobiliary & Pancreatic Diseases International2023年3期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Narrative medicine principles and organ donation communications
- Hepatobiliary&Pancreatic Diseases International
- Laparoscopic extended right hepatectomy for posterior and completely caudate massive liver tumor (with videos)
- Etiology and classification of acute pancreatitis in children admitted to ICU using the Pediatric Sequential Organ Failure Assessment (pSOFA)score
- Endoscopic ultrasound-guided drainage of peripancreatic fluid collections: What impacts treatment duration?
- Percutaneous ultrasound and endoscopic ultrasound-guided biopsy of solid pancreatic lesions: An analysis of 1074 lesions
