Characteristics of lymph node stations/basins metastasis and construction and validation of a preoperative combination prediction model that accurately excludes lymph node metastasis in early gastric cancer
Mengyu Feng,Jingtao Wei,Ke Ji,Yinan Zhang,Heli Yang,Xiaojiang Wu,Ji Zhang,Zhaode Bu,Jiafu Ji
Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing),Center of Gastrointestinal Cancer,Peking University Cancer Hospital&Institute,Beijing 100142,China
Abstract Objective:To explore the candidate indications for function-preserving curative gastrectomy and sentinel lymph node navigation surgery in early gastric cancer (EGC).Methods:The clinicopathological data of 561 patients with EGC who underwent radical gastrectomy for gastric cancer at Peking University Cancer Hospital from November 2010 to November 2020 with postoperative pathological stage pT1 and complete examination data,were collected.Pearson’s Chi-square test was used and binary logistic regression was employed for univariate and multivariate analyses.Combined analysis of multiple risk and protective factors for lymph node metastasis (LNM) of EGC was performed.A negative predictive value (NPV)combination model was built and validated.Results:LNM occurred in 85 of 561 patients with EGC,and the LNM rate was 15.15%.NPV for LNM reached 100% based on three characteristics,including ulcer-free,moderately well differentiation and patient <65 years old or tumor located at the proximal 1/3 of the stomach.Regarding lymphatic basin metastasis,multivariate analysis showed that the metastatic proportion of the left gastric artery lymphatic basin was significantly higher in male patients compared with female patients (65.96% vs. 38.89%,P<0.05).The proportion of right gastroepiploic artery lymphatic basin metastasis in patients with a maximum tumor diameter >2 cm was significantly greater than that noted in patients with a maximum tumor diameter ≤2 cm (60.78% vs.28.13%,P<0.05).Conclusions:Characteristics of lymph node stations/basins metastasis will facilitate precise lymph node resection.The NPV for LNM reaches 100% based on the following two conditions: young and middle-aged EGC patients,well-differentiated tumors,and without ulcers;or well-differentiated tumors,without ulcers,and tumors located in the proximal stomach.These findings can be used as the recommended indications for functionpreserving curative gastrectomy and sentinel lymph node navigation surgery.
Keywords: Early gastric cancer;lymph node metastasis;lymphatic basin;negative predictive value;functionpreserving curative gastrectomy with lymphatic basin dissection
Introduction
The diagnosis rate of early gastric cancer (EGC) in China has been significantly improved with the popularization of the “early diagnosis and treatment” concept in recent years.According to data from the Chinese Alliance for Gastrointestinal Cancer Surgery in 2020,the proportion of EGC patients in China gradually increased from 19.6% in 2014 to 21.7% in 2019.Regarding the diagnosis and treatment of ECG,approximately 25% of patients undergo endoscopic treatment. The proportion of patients undergoing open surgery has decreased to less than 1/4,and the proportion of patients undergoing laparoscopic surgery has increased significantly,accounting for greater than 50% of patients.Among all patients undergoing radical surgery,the incidence of lymph node metastasis(LNM) was 6.4% for stage T1a and 20.6% for stage T1b.Therefore,the characteristics of LNM in ECG require further exploration.
According to the current research,the existing technical means [including endoscopic ultrasonography (EUS),computed tomography (CT),etc.] are not sufficient to accurately estimate the lymph node status in ECG (1,2).LNM is the most critical factor affecting the prognosis of ECG and is also an important factor determining treatment selection.According to the current diagnosis and treatment guidelines,the treatment of ECG mainly includes endoscopic therapy and radical gastrectomy with lymph node dissection (3-5).However,only a small proportion of EGC patients are suited for endoscopic therapy.For most EGC patients who are not suited for endoscopic surgery,the recommended treatment method is radical gastrectomy and lymph node dissection according to the current guidelines.Because the incidence of LNM in EGC patients is not high,for most EGC patients,radical gastrectomy and lymph node dissection may be regarded as a relatively extended surgery.In recent years,some scholars have begun to explore function-preserving curative gastrectomy with lymphatic basin dissection.In addition,remarkable results have been achieved in a few clinical trials on sentinel lymph node biopsy in EGC,and a large number of related clinical trials are ongoing.
Therefore,the characteristics of LNM in EGC will be explored in this study based on single center data from Peking University Cancer Hospital.In addition,we will accurately analyze the negative predictive value (NPV) for LNM to accurately identify certain EGCs without LNM,potentially providing a basis for the selection of functionpreserving curative gastrectomy and sentinel lymph node navigation surgery.
Materials and methods
Study design and patients
This was a retrospective single-center non-interventional study conducted at Peking University Cancer Hospital in China.We retrospectively analyzed 561 EGC patients who received radical gastrectomy at Peking University Cancer Hospital between November 2010 and November 2020.For the external validation,data from 494 EGC patients without endoscopic ultrasonography reports between November 2010 and November 2020 were retrieved.This study was approved by the Medical Ethics Committee of the Peking University Cancer Hospital,and informed consent was obtained from all individuals.
The inclusion criteria were as follows: 1) patients who were pathologically diagnosed with gastric adenocarcinoma;2) patients undergoing radical gastrectomy and standard D1+/D2 lymph node dissection for the first time;and 3) postoperative pathological stage T1 according to the 8th edition of the American Joint Committee on Cancer(AJCC) TNM staging system.The exclusion criteria were as follows: 1) previous history of neoadjuvant therapy,including chemotherapy,targeted therapy and immunotherapy;2) two or more primary gastric cancer lesions;3) previous history of other cancer or remnant gastric cancer;4) locally advanced gastric cancer or distant metastasis;or 5) incomplete preoperative evaluation,including gastroscopy and biopsy,EUS,abdominal contrast-enhanced CT,etc.
Clinicopathological evaluation
Clinicopathological information,including sex,age,gastroscopic reports,biopsy pathological results,EUS reports,CT reports and postoperative pathological results,was retrospectively collected. Gastroscopic reports recorded tumor location,maximum tumor diameter and presence or absence of ulcer.The tumor location was classified as the esophagogastric junction (EGJ) or upper(U),middle (M),or lower (L) portion of the stomach.Regarding pathological results of the biopsy,the differentiated type included papillary adenocarcinoma and well and moderately differentiated tubular adenocarcinoma,and the undifferentiated type included poorly differentiated adenocarcinoma and signet-ring cell carcinoma,and mucinous adenocarcinoma.EUS/CT reports included enlarged lymph nodes with lengths ≥5 mm.Postoperative pathological results recorded T stage,vascular tumor thrombi,and the stations and number of metastatic and non-metastatic lymph nodes.
Statistical analysis
The statistical analyses were performed by using IBM SPSS Statistics (Version 22.0;IBM Corp.,New York,USA).The Pearson Chi-squared test and Fisher’s exact test (when appropriate) were used for comparisons of categorical variables.Significant factors noted on univariate analysis were subsequently entered into a binary logistic regression model for multivariate analysis.Two-sided P<0.05 was considered statistically significant.
To accurately analyze the characteristics of LNM and clinical treatment,combined analysis of multiple risk factors for LNM was performed.This type of combined analysis was defined as follows: a sample is included in the“YES” group when all the risk factors (two or more) are met simultaneously,if not,the sample is included in the“NO” group.
In addition,the sensitivity,specificity,positive predictive value (PPV) and NPV were calculated.In this study,we focused on NPV and a combined analysis of multiple protective factors for LNM was performed.We sought to confirm which combination of protective factors could be used to achieve an NPV of 100%.
Results
Baseline clinicopathological characteristics and risk factors for LNM
The baseline clinicopathological characteristics,including sex,age,tumor location,maximum tumor diameter,presence or absence of ulcer,enlarged lymph node indicated by CT/EUS,degree of differentiation,presence or absence of vascular tumor thrombi,total number of resected lymph nodes,T stage and N stage,are shown inTable 1.
LNM occurred in 85 of the 561 EGC patients enrolled in this study,with a relatively reasonable LNM rate(15.5%) according to previous studies.Among 85 patients with LNM,there were 50 (58.8%) patients with stage N1,28 (32.9%) with stage N2 and 6 (7.1%) with stage N3a according to the 8th edition of the AJCC staging system.Univariate and multivariate logistic regression analyses revealed that old age (≥65 years old),distal 2/3 of stomach,maximum tumor diameter >2 cm,presence of ulcers,enlarged lymph nodes indicated by CT/EUS,poor differentiation,vascular tumor thrombi and T1b stage were independent risk factors for LNM of EGC (Table 1).Based on the current indications for the endoscopic treatment of EGC,we selected four related risk factors,including the presence of ulcers,poor differentiation,maximum tumor diameter >2 cm and T1b stage,for further combined analysis.The LNM rate increased significantly when EGC patients possessed one or more risk factors,and the LNM rate showed an increasing trend from 20%-30% for one risk factor to 50%-60% for multiple risk factors (Table 2).
Protective factors of LNM
Based on the above risk factors for LNM in EGC,the inverse can be regarded as a protective factor: young and middle-aged (<65 years old),proximal 1/3 of the stomach,maximum tumor diameter ≤ 2 cm,absence of ulcers,no enlarged lymph nodes indicated by CT/EUS,well differentiated tumor,no vascular tumor thrombi and T1a stage.To make a more accurate preoperative negative prediction,preoperative protective factors were used for further analysis.The NPVs of the above 7 preoperative protective factors (young and middle-aged,proximal 1/3 of the stomach,maximum tumor diameter ≤2 cm,absence of ulcers,no enlarged lymph nodes indicated by CT,no enlarged lymph nodes indicated by EUS,and well differentiated tumor) for LNM were 86.21%,92.86%,90.09%,95.08%,87.63%,89.84% and 94.15%,respectively (Table 3).Therefore,absence of ulcers might be the optimal single factor to exclude LNM in EGC and it should be included in the next combination analyses.Then we calculated the NPVs of two factors combination and found that the NPV for LNM reached 99.21% when the EGC patients possessed the above two factors (absence of ulcers and well differentiated tumor) simultaneously,indicating that less than 1% of EGC patients would progress to LNM.Next,we performed combination analyses of three factors in order to find 100% NPV.Fortunately,we found that the NPV for LNM reached 100% when the EGC patients possessed three protectivefactors simultaneously,including absence of ulcers,well differentiated tumor,and young and middle-aged or tumor located at the proximal 1/3 of stomach (Table 4).
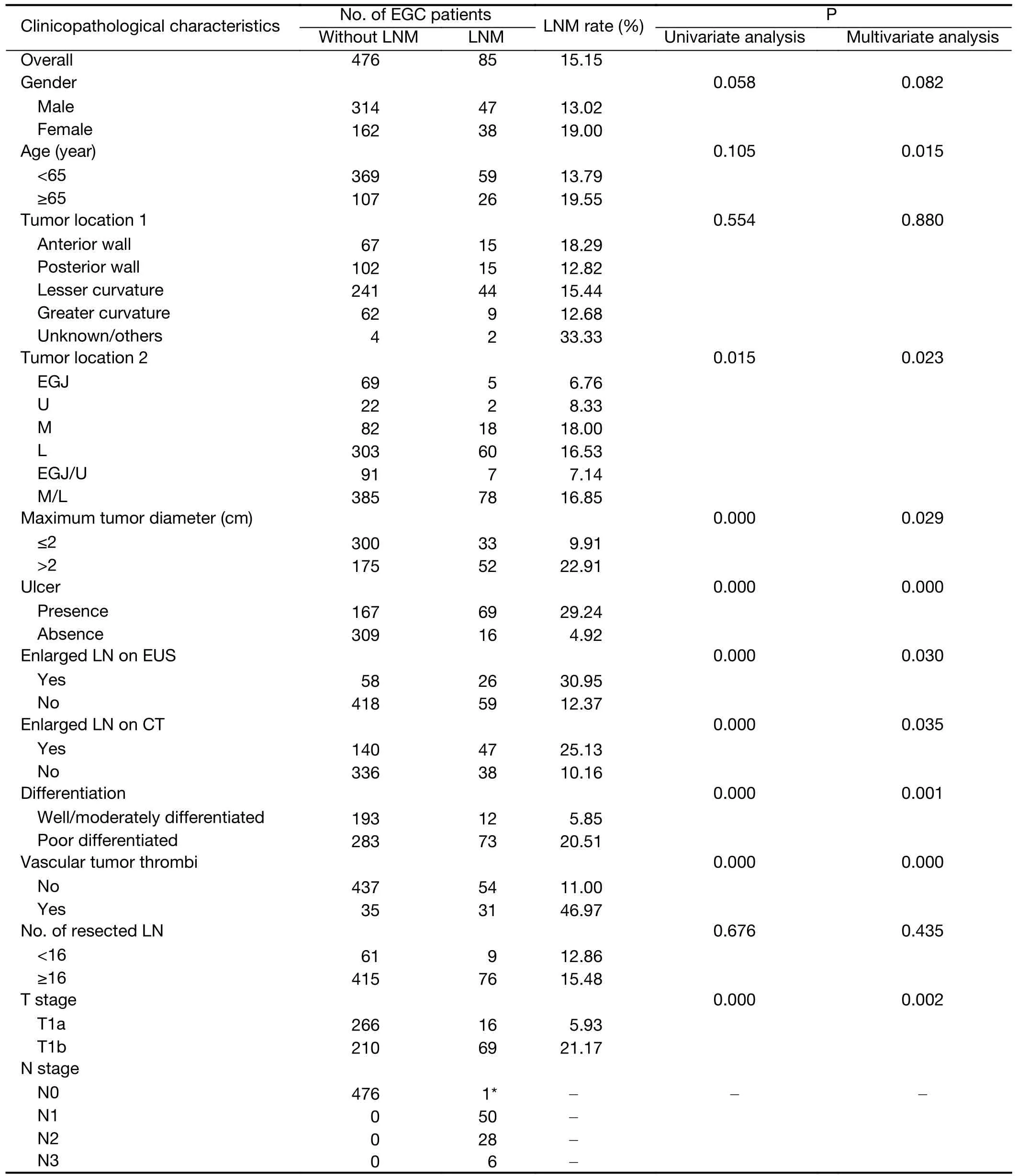
Table 1 Baseline clinicopathological characteristics of EGC and risk factors for LNM (N=561)
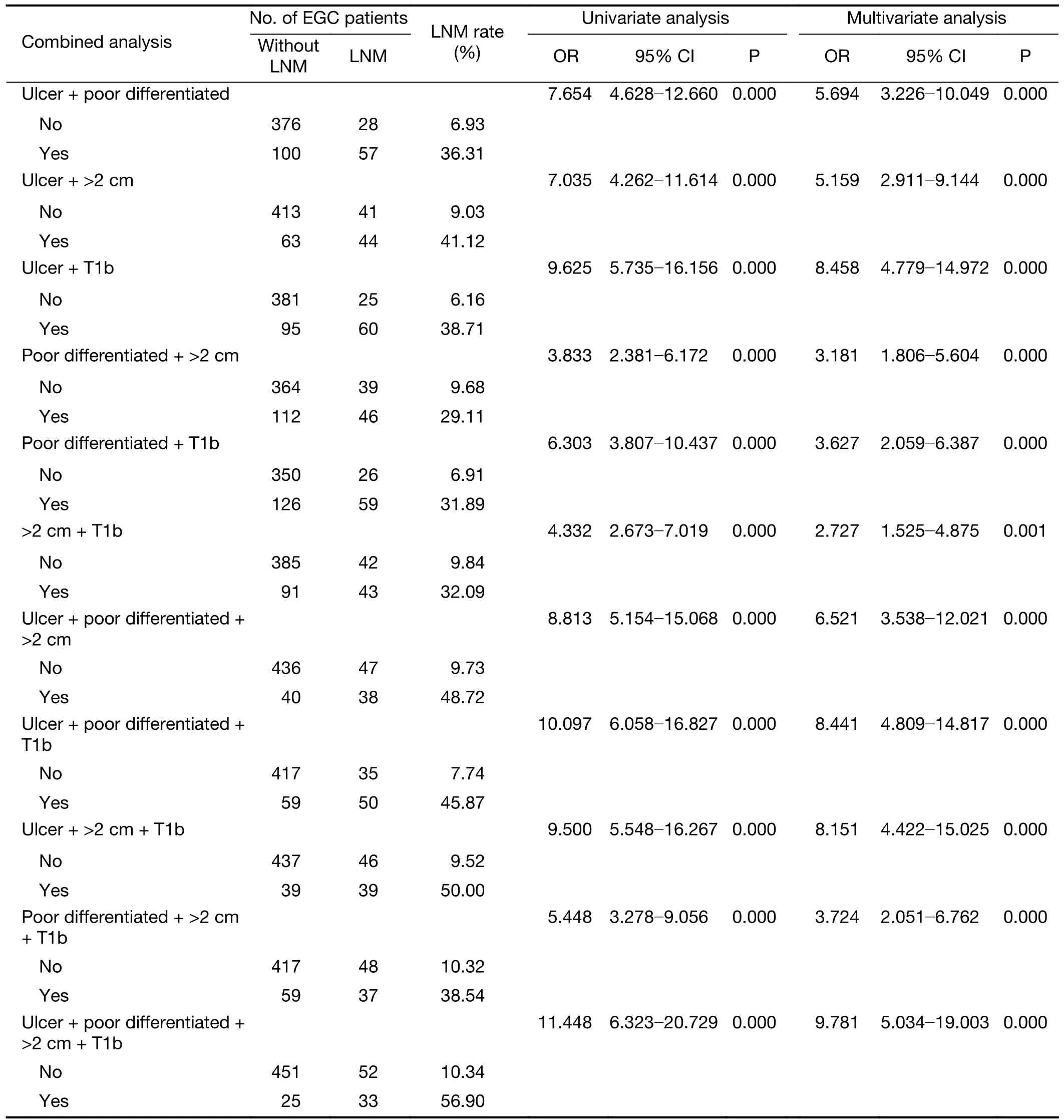
Table 2 Multiple risk factors combined analysis of LNM in EGC (N=561)
External validation for NPV combination analysis
To validate the accuracy of NPV combination test,clinicopathological information from 494 EGC patientswas retrospectively collected and the NPV was calculated based on the combination analysis.Among 494 patients,67(13.6%) patients had LNM.The NPV for LNM reached 100% when the EGC patients possessed two protective factors simultaneously,including absence of ulcers and well differentiated tumor. The NPV combination system showed good predictive accuracy and LNM exclusion ability (Table 5).
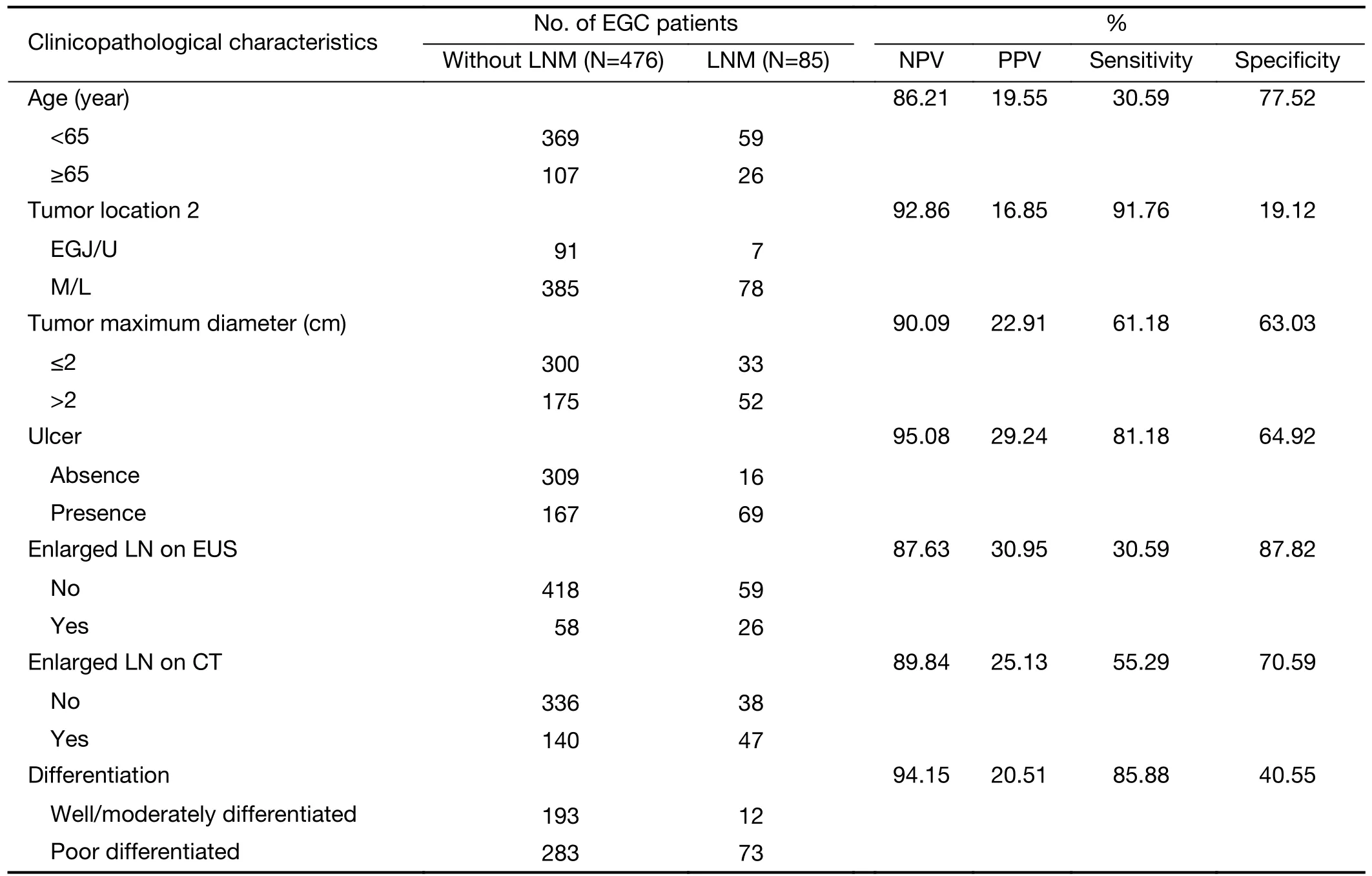
Table 3 Preoperative protective factors for LNM in EGC and negative predictive value analysis
Different regional lymph nodes
The LNM frequency of different stations varied based on tumor location,size,differentiation,etc.The LNM frequency was described according to the order from high to low as follows: No.3 (48.19%),No.6 (32.53%),No.4d(19.28%),No.7 (12.05%),No.5 (10.84%),No.9(10.84%),No.8a (9.64%),No.4sb (3.61%),No.1(2.41%),No.2 (1.20%),No.12a (1.20%),No.4sa (0).LNM occurred at the first level of the station in 63 of 83 EGC patients (75.90%),at both the first and second levels of the station in 17 (20.48%) of 83 EGC patients,and at only the second level of the station in 3 (3.61%) of 83 EGC patients (Table 6).
Then we analyzed the potential factors influencing the second level of the station metastasis.Univariate analysis revealed that no factors were related to the incidence of metastasis to the second level of the station;however,multivariate logistic regression analysis revealed that the incidence of metastasis to the second level of the station in the group with a maximum tumor diameter ≤2 cm was significantly greater than that in the >2 cm group (34.38%vs.17.65%,P<0.05),and the incidence of metastasis to the second level of the station in the group with vascular tumor thrombi was significantly greater than that in the group without vascular tumor thrombi (29.03%vs.21.15%,P<0.05).A maximum tumor diameter ≤2 cm and vascular tumor thrombi were independent risk factors for LNM atthe second level of the station,and the differences were statistically significant (Table 7).
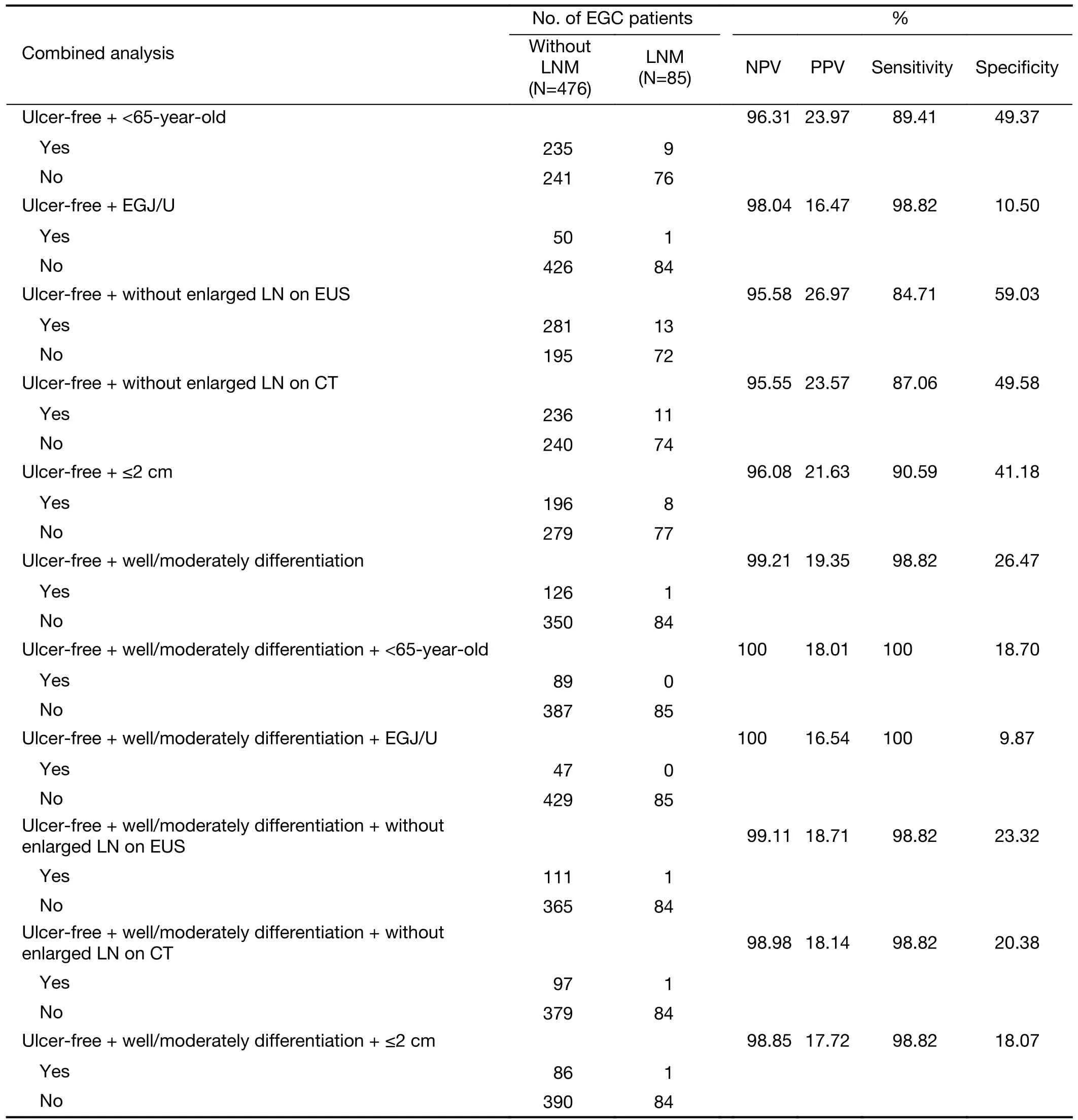
Table 4 Multiple preoperative protective factors combined analysis of LNM in EGC and NPV analysis
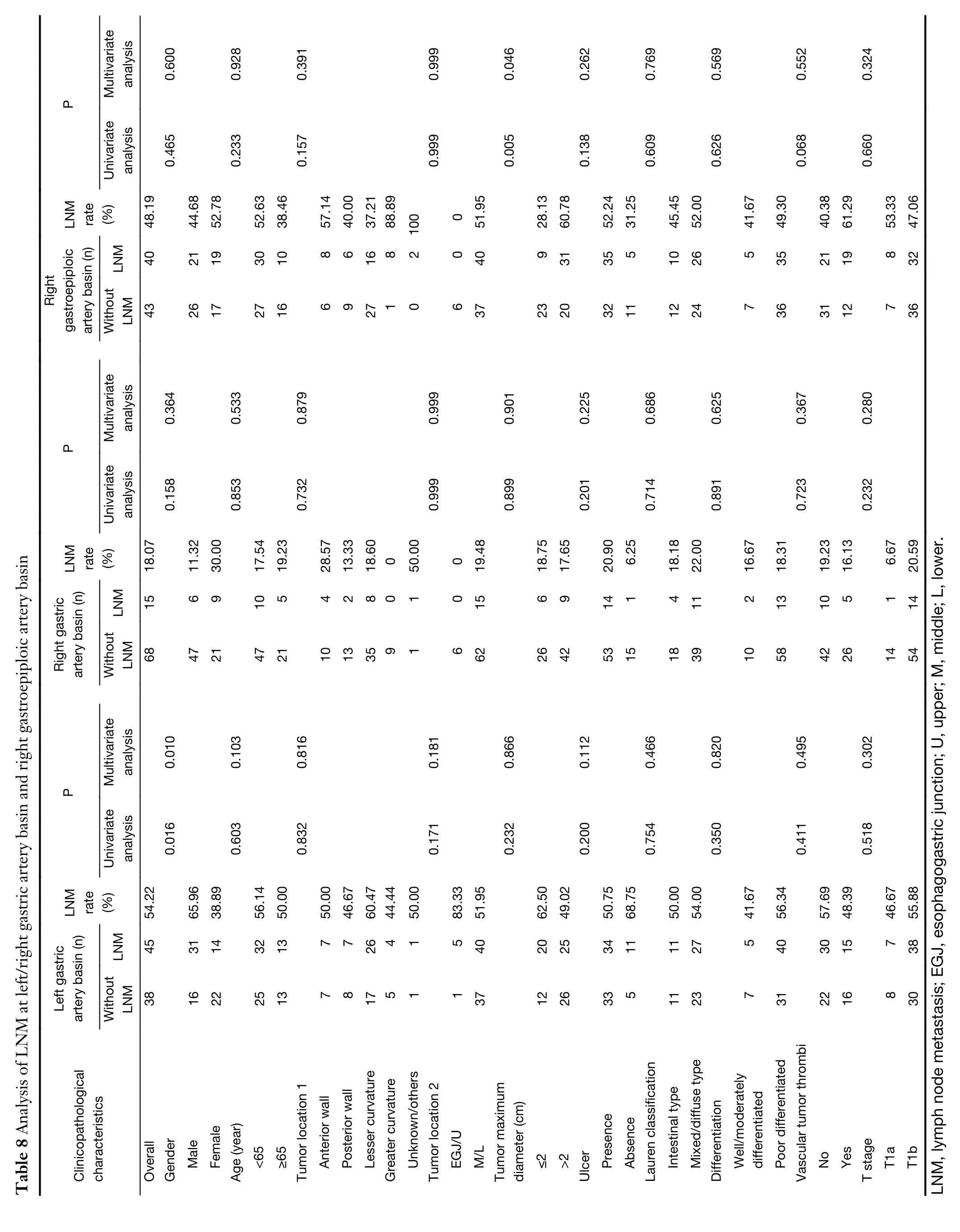
The lymphatic basin concept was used for sentinel lymph node biopsy in EGC.In this study,we tried to analyze the lymphatic basin metastasis of EGC based on the location of LNM.Due to the small number of metastatic cases of the left gastroepiploic artery basin,posterior gastric artery basin and other lymphatic basins,the left/right gastricartery basin and the right gastroepiploic artery basin were mainly analyzed in this study.Among 83 patients with LNM,there were 45 cases of left gastric artery basin (No.1/No.3/No.7) metastasis,15 cases of right gastric artery basin (No.5/No.8) metastasis,and 40 cases of right gastroepiploic artery basin (No.4d/No.6) metastasis.Univariate and multivariate logistic regression analyses revealed that the incidence of left gastric artery basin metastasis was significantly higher in male EGC patients compared with female patients (65.96%vs.38.89%,P<0.05),and male sex was an independent risk factor for left gastric artery basin metastasis.Univariate and multivariate logistic regression analyses revealed no independent risk factor for right gastric artery basin metastasis.However,the characteristics of right gastric artery basin metastasis were described as follows: There were 9 cases with tumors located at the greater curvature,none of which had LNM in the right gastric artery basin;there were 6 cases with tumors located in the proximal 1/3 stomach,none of which had LNM in the right gastric artery basin.Univariate and multivariate logistic regression analysis revealed that the incidence of right gastroepiploic artery basin metastasis in EGC patients with a maximum tumor diameter >2 cm was significantly greater than that of patients with a maximum tumor diameter ≤2 cm (60.78%vs.28.13%,P<0.05),and maximum tumor diameter >2 cm was an independent risk factor for right gastroepiploic artery basin metastasis.Otherwise,there were 6 cases with tumors located in the proximal 1/3 stomach,none of which experienced LNM in the right gastroepiploic artery basin(Table 8).
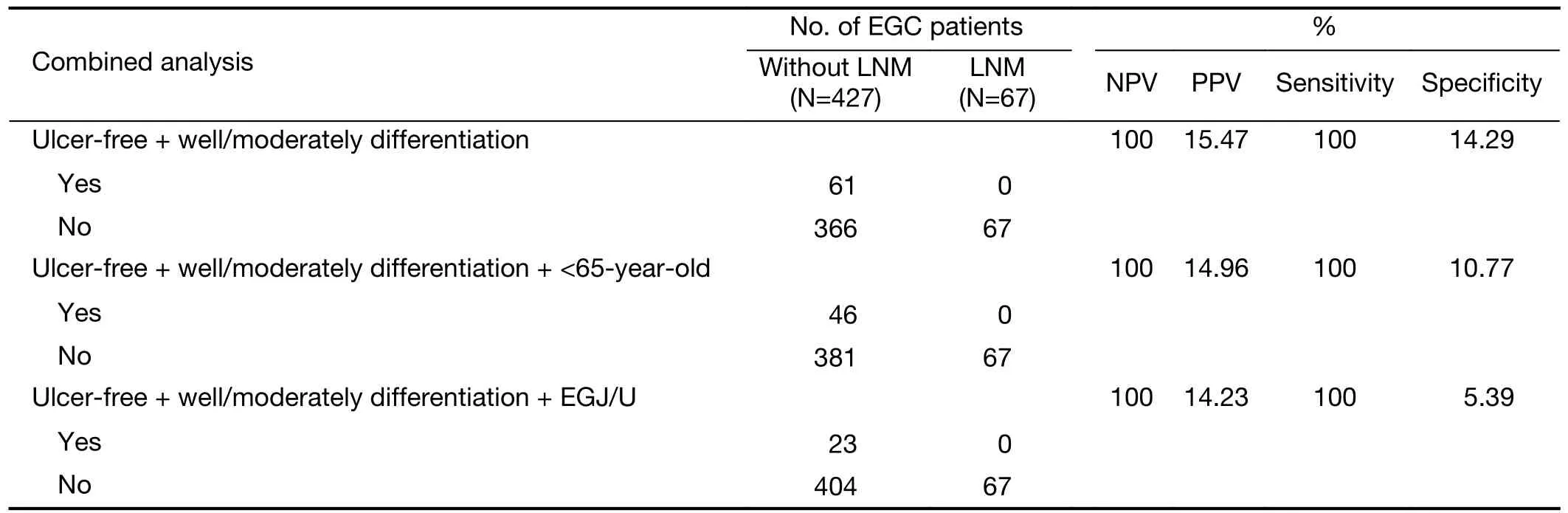
Table 5 External validation for negative predictive value analysis in EGC
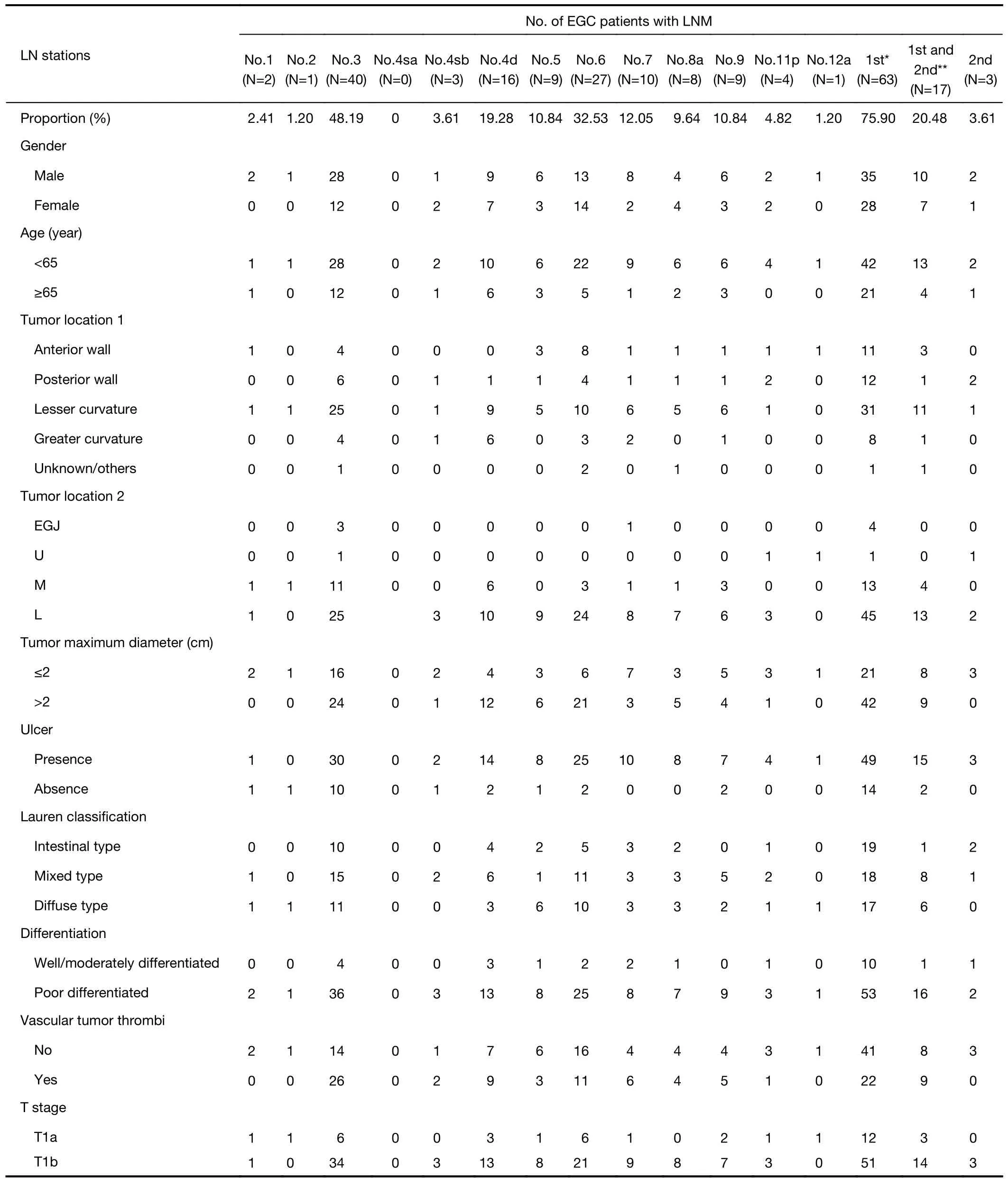
Table 6 Analysis of different metastatic LN stations
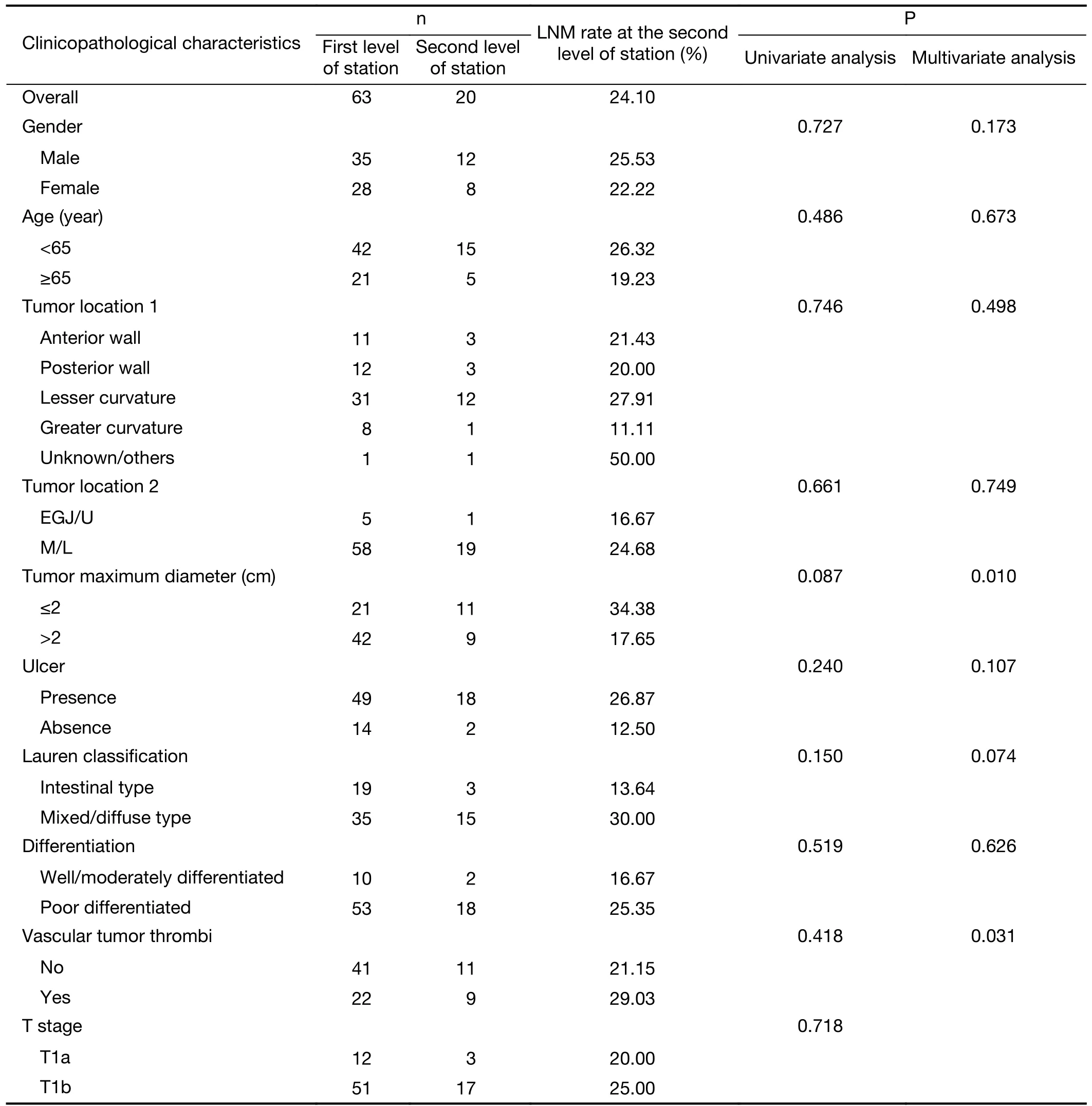
Table 7 Analysis of LNM at the second level of stations
Discussion
The evaluation of lymph node status is very important for the selection of treatment for EGC.The LNM rate of EGC reported in this study was 15.15%,which was similar to the data reported in previous studies (6-10).EUS and CT are the most commonly used methods to evaluate the lymph node status of EGC (11).Studies have shown that the sensitivity and specificity of EUS in determining LNM in EGC are 0.83 and 0.67,respectively.Due to poor penetration of ultrasound,lymph nodes located far away from perigastric areas cannot be obtained (2).The results of this study suggested that the NPV,PPV,sensitivity and specificity of EUS in diagnosing LNM were 87.63%,30.95%,30.59% and 87.82%,respectively.In addition,the results of this study suggested that the NPV,PPV,sensitivity and specificity of CT in diagnosing LNM were 89.84%,25.13%,55.29% and 70.59%,respectively.Therefore,the method is insufficient to diagnose LNM of EGC by using EUS and CT,and it is important to accurately analyze the risk and protective factors of EGC.
Several risk factors for LNM in EGC,including maximum tumor diameter >2 cm,invasion of submucosa,poor differentiation,presence of ulcer,and vascular tumor thrombi (8,10),have been reported in previous studies.These results were similar to the results of this study.Endoscopic therapy for EGC was also based on these related researches,and the current absolute indications for endoscopic resection were defined as follows: a differentiated-type adenocarcinoma without ulcerative findings (UL0),in which the depth of invasion was clinically diagnosed as T1a and the diameter was ≤2 cm(4,5).Therefore,the following four risk factors were used for combined risk factor analysis: presence of ulcers,poor differentiation,maximum tumor diameter >2 cm and T1b stage.We found that the LNM rate increased significantly when the EGC patients possessed at least one risk factor,and it showed an increasing trend from 20%-30% for one risk factor to 50%-60% for four risk factors.When two risk factors were present,the LNM rate in the group with the presence of ulcers and maximum tumor diameter >2 cm(41.12%) was the highest.When three risk factors were present,the LNM rate was 50% in the group with the presence of ulcers,maximum tumor diameter >2 cm and T1b.When four risk factors were present simultaneously,the LNM rate reached 56.9%.Therefore,EGC patients with risk factors should receive radical gastrectomy and D1+/D2 lymphadenectomy.EGC patients with risk factors might not be suited for exploratory function-preserving curative gastrectomy with lymphatic basin dissection.
Conversely,the opposite risk factors are regarded as protective factors.In this study,the protective factors for LNM in EGC included young and middle-aged (<65 years old),proximal 1/3 of stomach,tumor maximum diameter ≤2 cm,absence of ulcers,no enlarged lymph nodes indicated by CT/EUS,well differentiated tumor,no vascular tumor thrombi and T1a stage.The roles of absence of ulcers and well differentiated tumor in excluding LNM were noteworthy among the above protective factors.When EGC patients have no ulcers or tumors are well differentiated,the probability of LNM is very low.This information can be used to exclude LNM for EGC.The NPV for LNM reached 99.21% when the EGC patients possessed the above two protective factors simultaneously,indicating that less than 1% of EGC patients would progress to LNM.On this basis,the ability to exclude LNM will be further improved as the number of protective factors increases.The NPV for LNM reached 100% when EGC patients possess three protective factors simultaneously,including the absence of ulcers,well differentiated tumor,and young and middle-aged or tumors located at the proximal 1/3 of the stomach.This predictive model was validated by external data and its prediction accuracy was 100%.Therefore,EGC patients with the above 3 protective factors should be recommended to receive endoscopic resection or function-preserving curative gastrectomy.
Radical gastrectomy is currently the recommended standard operation for EGC tumors that do not meet the absolute indication for endoscopic therapy.Although lymph node dissection for EGC is clearly defined in the current diagnosis and treatment guidelines,the scope of lymph node dissection remains controversial due to inaccurate evaluation of lymph node status before and during surgery.In this study,we tried to provide guidance for the prediction of LNM by analyzing the location of LNM and its characteristics.The frequency of LNM occurring at No.3 and No.6 was the highest among all the lymph node stations;the frequency of LNM occurring at the second level of the station was close to 25%.Therefore,D2 lymphadenectomy was recommended for EGC patients with high LNM risk,and D1/D1+lymphadenectomy was recommended for EGC patients with lower LNM risk.
Given the increase in research on EGC,functionpreserving curative gastrectomy has gradually been taken seriously in recent years due to the continuous improvement of patients’ requirements for postoperative quality of life.Function-preserving curative gastrectomy is defined relative to standard radical gastrectomy,including proximal gastrectomy,pylorus-preserving gastrectomy,segmental gastrectomy,local resection,D1/D1+lymphadenectomy and sentinel node navigation surgery (4,12).Therefore,accurate evaluation of lymph node status is required for function-preserving curative gastrectomy.In recent years,a number of clinical trials in Japan and South Korea have shown that the safety and therapeutic effect of sentinel lymph node navigation surgery in EGC have reached expectations (13-19).A multicenter study in Japan showed that the detection rate of sentinel lymph nodes in EGC could reach 97.5%,with 93% sensitivity and 99%accuracy (20).A recent multicenter RCT study(SENORITA) conducted in South Korea in 2013 was completed,and its research output was published in the Journal of Clinical Oncology.A total of 580 EGC patients were enrolled,including 292 patients in the sentinel lymph node biopsy group and 288 patients in the traditional radical gastrectomy group.The results showed that the sentinel lymph node biopsy group did not show noninferiority to radical gastrectomy group for 3-year DFS,with a 5% margin.However,the 3-year DSS and 3-year OS values did not differ after rescue surgery in cases of recurrence/metachronous gastric cancer,and the sentinel lymph node biopsy group had better long-term quality of life and nutrition than the radical gastrectomy group(14,15).The lymphatic basin is an important concept in sentinel lymph node navigation surgery.In this study,the results showed that the proportions of patients with LNM occurring in the left gastric artery basin,right gastroepiploic artery basin and right gastric artery basin were 54.22%,48.19% and 18.07%,respectively.Male sex was an independent risk factor for LNM in the left gastric artery basin,and maximum tumor diameter >2 cm was an independent risk factor for LNM in the right gastroepiploic artery basin.LNM was not observed in the right gastric artery basin in any patient with EGC with tumors located at the greater curvature.LNM was not observed in the right gastric artery basin or right gastroepiploic artery basin in all patients with EGC with tumors located at the proximal 1/3 of the stomach.Therefore,when function-preserving curative gastrectomy and sentinel lymph node navigation surgery are performed,we can refer to the above data to individually select sentinel lymph node biopsy and lymph node resection range according to sex,tumor location and tumor size.In addition,based on the aforementioned negative predictive analysis results,EGC patients with a low risk of LNM(NPV=100%) are suited to undergoing function-preserving curative gastrectomy and sentinel lymph node navigation surgery.
This study still has several limitations.First,many EGC patients were excluded due to a lack of EUS reports,which might result in selection bias.Second,this study was a retrospective study.Third,the LNM incidence in EGC was low and there were only 83 EGC patients with LNM,which might lead to analysis bias on LNM stations and basins.More studies should be performed before clinical application.Although NPV is more important in this study,PPV also needs attention,and NPV may have greater variability in different centers.
Conclusions
The risk of LNM increases as the number of risk factors increases.The NPV for LNM reaches 100% in the context of the following two conditions: young and middle-aged EGC patients,well differentiated tumors,and without ulcers;or well differentiated tumors,without ulcers,and tumors located in the proximal stomach.These findings can be used as the recommended indications for functionpreserving curative gastrectomy and sentinel lymph node navigation surgery.
Acknowledgements
This work was supported by Beijing Hospitals Authority Clinical Medicine Development of Special Funding (No.XMLX202119) and Open Project funded by Key Laboratory of Carcinogenesis and Translational Research,Ministry of Education/Beijing (No.2022 Open Project-6).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2022年5期
Chinese Journal of Cancer Research2022年5期
- Chinese Journal of Cancer Research的其它文章
- Correlation between imaging features on computed tomography and combined positive score of PD-L1 expression in patients with gastric cancer
- Evaluation of triage strategies for high-risk human papillomavirus-positive women in cervical cancer screening: A multicenter randomized controlled trial in different resource settings in China
- Colorectal cancer burden,trends and risk factors in China:A review and comparison with the United States
- Myeloid checkpoints for cancer immunotherapy
- National guidelines for diagnosis and treatment of malignant lymphoma 2022 in China (English version)
- Beyond images: Emerging role of Raman spectroscopy-based artificial intelligence in diagnosis of gastric neoplasia
