Evaluation of triage strategies for high-risk human papillomavirus-positive women in cervical cancer screening: A multicenter randomized controlled trial in different resource settings in China
Le Dang ,Linghua Kong ,Yuqian Zhao ,Yi Dai ,Li Ma ,Lihui Wei ,Shulan Zhang,Jihong Liu,Mingrong Xi,Long Chen,Xianzhi Duan0,Qing Xiao,Guzhalinuer Abulizi2,Guonan Zhang,Ying Hong,Qi Zhou,Xing Xie,Li Li,Mayinuer Niyazi,Zhifen Zhang,Jiyu Tuo,Yiling Ding2,Youlin Qiao,Jinghe Lang
1Department of Gynecology and Obstetrics,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences/Peking Union Medical College,Beijing 100730,China;2National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China;3Center for Cancer Prevention Research,Sichuan Cancer Hospital and Institute,Sichuan Cancer Center,School of Medicine,University of Electronic Science and Technology of China,Chengdu 610041,China;4Department of Epidemiology,Dalian Medical University,Dalian 116044,China;5 Department Obstetrics and Gynecology,Peking University People’s Hospital,Beijing 100044,China;6Department of Obstetrics and Gynecology,Shengjing Hospital Affiliated to China Medical University,Shenyang 110004,China;7 Department of Gynecology and Obstetrics,Sun Yat-sen University Cancer Center,Guangzhou 510060,China;8Department of Gynecology and Obstetrics,West China Second University Hospital,Sichuan University,Chengdu 610041,China;9Department of Gynecology and Obstetrics,Zhejiang Xiaoshan Hospital Affiliated to Hangzhou Normal University,Chinese Academy of Medical Sciences/Zhejiang Xiaoshan Hospital Affiliated to Hangzhou Normal University,Hangzhou 310000,China;10 Department of Obstetrics and Gynecology,Beijing Tongren Hospital,Capital Medical University,Beijing 100730,China;11Department of Gynecology and Obstetrics,the Eight Affiliated Hospital Sun Yat-sen University,Shenzhen 518000,China;125th Department of Gynecology,the Affiliated Cancer Hospital of Xinjiang Medical University,Urumqi 830011,China;13Department of Gynecologic Oncology,Sichuan Cancer Hospital&Institute,Sichuan Cancer Center,School of Medicine,University of Electronic Science and Technology of China,Chengdu 610041,China;14 Department of Gynecology and Obstetrics,Nanjing Drum Tower Hospital,Affiliated Hospital of Nanjing University Medical School,Nanjing 210008,China;15Department of Gynecological Oncology,Chongqing University Cancer Hospital/Chongqing Cancer Hospital,Chongqing 400030,China;16 Department of Gynecologic Oncology,Women’s Hospital,School of Medicine Zhejiang University,Hangzhou 310006,China;17Department of Gynecology and Obstetrics,Tumor Hospital of Guangxi Zhuang Autonomous Region,Nanning 530021,China;18Department of Gynecology,People’s Hospital of Xinjiang Uygur Autonomous Region,Urumqi 830000,China;19 Department of Gynecology,Hangzhou Women’s Hospital,Hangzhou 310016,China;20 Department of Gynecology and Obstetrics,Hubei Cancer Hospital,Tongji Medical College,Huazhong University of Science and Technology,Wuhan 430079,China;21 Department of Gynecology and Obstetrics,the Second Xiangya Hospital of Central South University,Changsha 410011,China;22School of Population Medicine and Public Health,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100005,China
Abstract Objective:We aimed to evaluate the effectiveness of different triage strategies for high-risk human papillomavirus (hrHPV)-positive women in primary healthcare settings in China.Methods:This study was undertaken in 11 rural and 9 urban sites.Women aged 35-64 years old were enrolled.HrHPV-positive women were randomly allocated to liquid-based cytology (LBC),visual inspection with acetic acid and Lugol’s iodine (VIA/VILI) (rural only) triage,or directly referred to colposcopy (direct COLP).At 24 months,hrHPV testing,LBC and VIA/VILI were conducted for combined screening.Results:In rural sites,1,949 hrHPV-positive women were analyzed.A total of 852,218 and 480 women were randomly assigned to direct COLP,LBC and VIA/VILI.At baseline,colposcopy referral rates of LBC or VIA/VILI triage could be reduced by 70%-80%.LBC (n=3 and n=7) or VIA/VILI (n=8 and n=26) could significantly decrease the number of colposcopies needed to detect one cervical intraepithelial neoplasia (CIN) 2 or worse and CIN3+compared with direct COLP (n=14 and n=23).For the 24-month cumulative detection rate of CIN2+,VIA/VILI triage was 0.50-fold compared with LBC triage and 0.46-fold with the direct COLP.When stratified by age,baseline LBC triage+performed best (P<0.001),peaking among women aged 35-44 years(Ptrend=0.002).In urban sites,1,728 women were hrHPV genotyping test positive.A total of 408,571 and 568 women were randomly assigned to direct COLP for HPV16/18+,direct COLP for other hrHPV subtypes+,and LBC triage for other hrHPV subtypes+.LBC (n=12 and n=31) significantly decreased the number of colposcopies needed to detect one CIN2+and CIN3+compared with direct COLP (n=14 and n=44).HPV16/18+increased the 24-month cumulative detection rate of CIN2+(17.89%,P<0.001).Conclusions:LBC triage for hrHPV-positive women in rural settings and direct COLP for HPV16/18+women and LBC triage for other hrHPV subtype+women in urban settings might be feasible strategies.
Keywords: Cervical cancer screening;hrHPV-positive;LBC;triage strategy;VIA/VILI
Introduction
Cervical cancer is the fourth most common female malignancy.There are approximately 604 thousand new cases of cervical cancer worldwide,with over 341 thousand deaths each year (1).Nearly 90% of cervical cancer cases occur in developing countries (2).The World Health Organization (WHO) announced a global strategy in 2020 encompassing its “90-70-90” targets,which must be met by 2030 for countries to be on the path toward cervical cancer elimination (3).One of the targets is that 70% of women will be screened with a high-performance test by 35 years of age and again by 45 years of age.In China,cervical cancer incidence and mortality rates are both higher in rural than in urban areas (4).With a large population,disparities in economic development,inequality distribution of quality health care,and substantial differences in the disease burden in rural and urban areas have restricted the elimination of cervical cancer in China(5,6).Only 21.4% of women aged ≥21 years had been screened for cervical cancer by 2014,with significant geographical variations (7).Meeting the screening target of 70% will be a massive challenge in China,especially in primary health care settings.Much work toward the comprehensive prevention and control of cervical cancer remains to be done before the disease can be eliminated.
Given its clear etiology,its long preinvasive phase,and the availability of effective prevention channels,the prospects for prevention and elimination of cervical cancer are the most promising of those associated with all types of cancer.As well known,high-risk human papillomavirus(hrHPV) is the leading cause of cervical cancer (8),and thus HPV DNA testing for cervical cancer screening offers a prospective prevention method.It has been demonstrated that HPV-based cervical cancer screening is effective as a primary screening method (9-12) and is significantly superior to traditional methods in primary healthcare settings (13,14).Moreover,a simple,affordable,fast and accurate HPV DNA test (careHPV,Qiagen) especially designed for cervical cancer screening in low-and middleincome countries (LMICs) obtained WHO prequalification in 2018 (15).With this advance,the barriers of high cost and high laboratory and technician requirements for HPV testing in low-resource settings will be well addressed.
However,HPV testing has high sensitivity but low specificity (11,16).As a growing number of countries prepare to adopt the HPV testing as a primary screening method,effective triage is crucial to ensure that unnecessary colposcopy referral and overtreatment will be avoided.A growing number of algorithms are currently being evaluated as possible triage approaches worldwide(16-19).However,many novel techniques are currently not feasible due to their requirements to adequate healthcare infrastructure in terms of laboratories,rigorous training of personnel,and quality control measures.In addition,they are not widely affordable due to high costs.Therefore,how best to manage hrHPV-positive women in cervical cancer screening remains a topic of debate.Screening programs,including management strategies,should be based on local needs in terms of financial and human resources,infrastructure and capacities,societal norms and patient acceptability,and the level of cancer risk reduction desired,as no single screening program or triage strategy fits all situations (16).Healthcare decision-makers in developing countries must take into consideration these priorities when selecting among alternative methods for managing hrHPV-positive women in different economic areas.
It is vital to select accurate and reliable triage strategies for hrHPV-positive women that are appropriate to different economic areas by means of large scale,population-based,realistic studies in the real world.In line with this,the study aimed to evaluate the clinical performance and accumulative risks of high-grade cervical intraepithelial neoplasia (CIN) or worse associated with different triage strategies for hrHPV-positive women in rural and urban areas in China.
Materials and methods
Study design and population
Based on China’s nationwide screening program,20 sites were selected from China’s seven geographical regions in total,including 11 rural sites and 9 urban sites.All screening procedures were conducted at local hospitals,and each site was supervised by a provincial-level comprehensive hospital.The study was approved by the Ethics Committees of Peking Union Medical College Hospital and all participating hospitals (No.S-705).The protocol is available online at www.chictr.org.cn.This trial is registered in the Chinese Clinical Trial Registry (No.ChiCTR1900022530).The details of this study have been well described previously (9,14).Briefly,a multicenter,unblinded randomized trial was carried out from 2015 to 2018,and eligible women aged 35-64 years were randomized into screening by liquid-based cytology (LBC),hrHPV testing [In urban sites,the polymerase chain reaction-based Cobas 4800 test (Roche Diagnostics) or Liferiver hrHPV genotyping kit (ZJ Bio-Tech) was applied.In rural sites,the hybrid capture-based careHPV(QIAGEN) assay was used (9)],or visual inspection with acetic acid and Lugol iodine (VIA/VILI,rural only).Eligible women were those who had no history of cervical cancer or hysterectomy and no clinical symptoms of pregnancy and who could understand the study procedures,voluntarily participated and were sexually active.All enrolled women provided written informed consent and received a questionnaire regarding to their sociodemographic and reproductive behavioral information.In this paper,we focus mainly on hrHPV-positive women in the hrHPV primary screening arm.Women with incomplete screening results were excluded from the analysis.Triage strategies designed for hrHPV-positive women in rural sites and urban sites are illustrated inFigure 1.
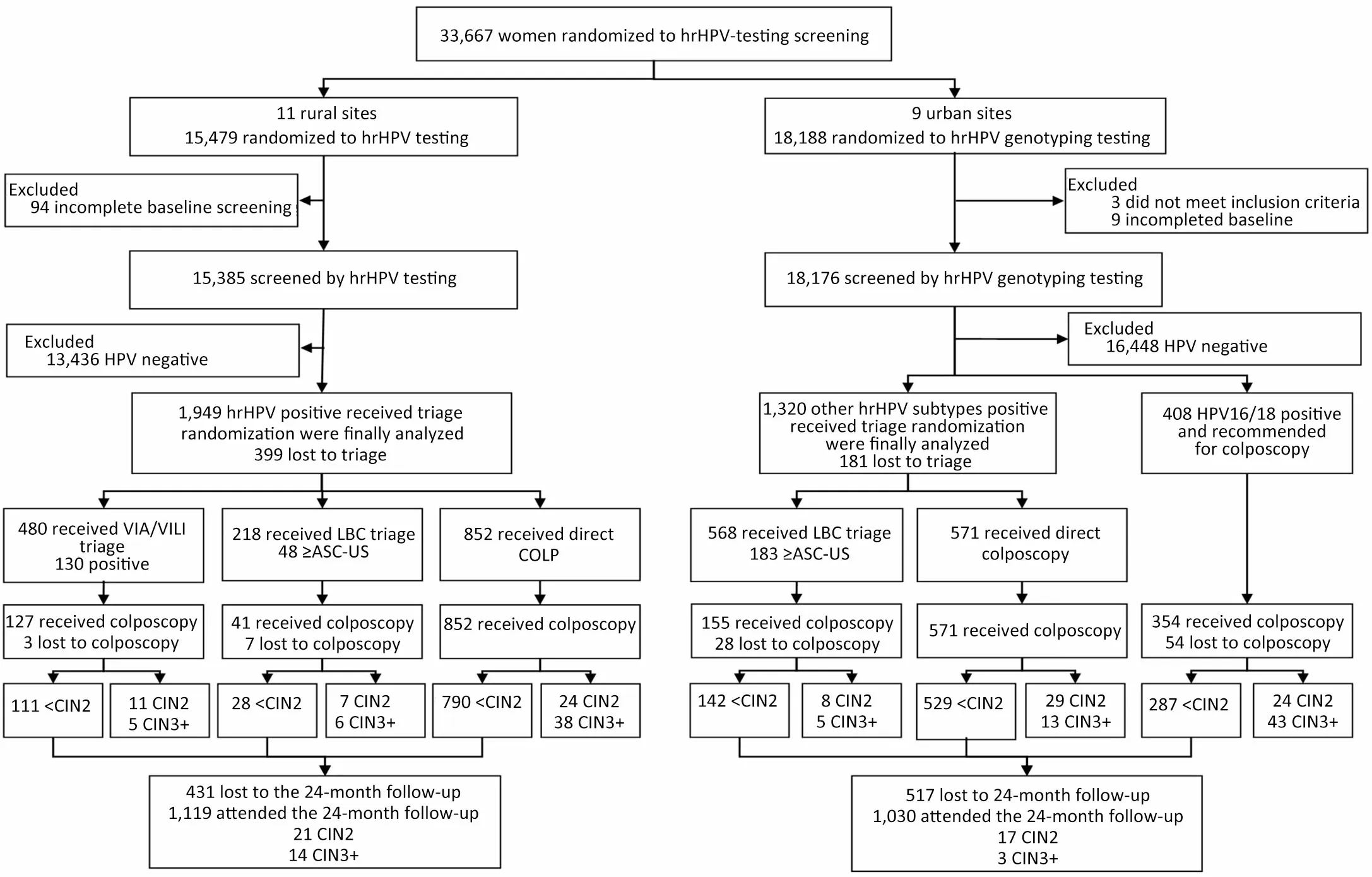
Figure 1 Study profile.In four rural sites where no cytology system was available,hrHPV+women were randomly assigned at a 1:1:1 ratio to VIA/VILI triaging,LBC triaging,or direct COLP.One urban site withdrew from the trial before the 24-month follow-up and was excluded from the analysis.Other hrHPV-subtypes+women were randomly assigned at a 1:1 ratio to LBC triaging or direct referral to colposcopy without triaging.VIA/VILI,visual inspection with acetic acid and Lugol’s iodine;hrHPV,high-risk human papillomavirus;LBC,liquid-based cytology;ASC-US,atypical squamous cells of undetermined significance;NILM,negative for intraepithelial lesion or malignancy;CIN,cervical intraepithelial neoplasia;COLP,referral to colposcopy without triage.
Procedures
All screening and diagnostic procedures were performed by well-trained local health providers.hrHPV-positive women were registered when they were called back,and the triage procedures were explained by a local health worker.The randomization scheme was performed in an ACCESS participant registration database.The trained local health workers immediately obtained the triage allocation from the computer after inputting the national identification number of each participant.Informed consent and a questionnaire for sociodemographic and reproductive behavioral information were obtained during the primary procedure by local health workers.Then,women received their triage test or direct colposcopy without triage in the gynecologic examination room according to their random allocations.
In rural sites,participants who tested hrHPV-positive were randomly assigned to VIA/VILI triage,LBC triage,or direct referral to colposcopy without triage (direct COLP) with a 1:1:1 ratio in the call-back examination.In four rural sites without cytological capacity,hrHPVpositive women were triaged by VIA/VILI or direct COLP at a 1:1 ratio.In urban sites,enrolled women with HPV 16/18+were referred for colposcopy,and women with other hrHPV subtypes+were randomly assigned to LBC triage (other hrHPV subtypes+with LBC triage) or direct COLP (other hrHPV subtypes+without triage) at a 1:1 ratio.The women assigned to the direct COLP arm without triage immediately received colposcopy examinations,and the women allocated to the LBC or VIA/VILI (in rural areas only) triage arm were rescreened following the aforementioned procedures;triage abnormal women were referred to colposcopy.The necessary biopsy specimens were obtained under colposcopy guidance.Four-quadrant random biopsies at the squamous column junction and endocervical curettage (ECC) were performed if there were high-grade cytology abnormalities but a normal colposcopy impression.
At 24 months after the baseline screening,all participants except the women who were histologically diagnosed as CIN 2 or worse were called back for follow-up screening.In rural sites,women were simultaneously screened by hrHPV testing,LBC and VIA/VILI.In urban sites,women were screened by hrHPV genotyping tests and LBC.Women with any positive results were referred to colposcopy directly.
Outcome verification
The result of LBC was graded according to the Bethesda System,and atypical squamous cells of undetermined significance or worse (ASC-US+) were deemed positive.The CIN classification systems were used for histology.The pathology processing and readings were performed at local sites.Ten percent of random samples of negative cytology,20% of negative histopathology samples,and all positive cytology and histopathology specimens by local pathologists would be reviewed by an external pathologist from the provincial hospitals (9).The final diagnosis was based on the worst findings across all histology findings.Biopsy confirmed that CIN2+and CIN3+were used as clinical outcome endpoints.The primary outcomes were the baseline detection rate,the 24-month detection rate,and the 24-month cumulative detection rates of CIN2+and CIN3+lesions.The secondary outcome was the number of colposcopies for one case of CIN2+or CIN3+.
Statistical analysis
Statistical analyses were performed on the intention-toscreen population.We present the number of hrHPVpositive women and the proportion of triage-positive and high-grade CIN detection for women in the different triage strategy groups.Screening efficiency was evaluated by the number of colposcopies required to detect one case of CIN2+or CIN3+.We estimated the 24-month cumulative detection rates for CIN2+and CIN3+in different triage strategies and stratified by age group.Continuous variables are presented as the median and interquartile range (IQR).Counts and percentages are presented for categorical data,and the Chi-squared test was performed for comparison.The Wilson score method was used to calculate 95% confidence intervals (95% CIs).We adjusted the rates by the direct methods of standardization(20).Rates ratio (RR) with 95% CIs were used to compare the 24-month cumulative detection rates for CIN2+and CIN3+of different triage strategies.All statistical tests were performed with SAS 9.4 (SAS Institute Inc,Cary,NC,USA).Two-sided P values less than 0.05 were considered statistically significant.
Results
Baseline characteristics of participants
A total of 33,667 participants were randomly located in the hrHPV arm. In rural sites,15,385 eligible women completed the hrHPV baseline screening,and 1,949 women had hrHPV-positive results (12.7%).A total of 480,218,and 852 women were randomly referred for VIA/VILI triage,LBC triage and direct COLP,respectively.A total of 1,119 hrHPV-positive women completed the follow-up screening at 24 months (Figure 1).In urban sites,18,176 participants were screened by hrHPV genotyping,and 1,728 (9.5%) hrHPV-positive results were finally analyzed.A total of 408 women tested HPV16/18+and were referred to colposcopy directly,and 1,320 other hrHPV-subtypes+women were randomly triaged by LBC (N=568) or direct COLP (N=571).At 24 months,1,030 hrHPV-positive women attended the follow-up screening (Figure 1).A total of 399 (20.5%) and 181 (10.5%) women were lost to triage in rural and urban sites,respectively. The sociodemographic and reproductive characteristics of the hrHPV+women in the 11 rural sites and 9 urban sites are shown inTable 1.The triage arms were comparable on demographic information across rural and urban sites(Table 1).The demographics were compared between the women who were lost to triage and received triage(Supplementary Table S1).
The Palestinian worker was eventually released after the mistake came to light?abut not before he underwent hours of questioning. Facebook apologized for the mistake and said it took steps to correct it.
We also compared the baseline information between women who were followed-up and lost to follow-up(Supplementary Table S2) and discovered that except smoking status in urban sites,there were no significant differences between the two groups.The smoking rate of Chinese women is low,and one case more or less would cause large vibration of the outcome.
Performance of different triage arms for HPV-positive women
Table 2demonstrates the outcomes at baseline,the 24-month and the 24-month cumulative follow-up screening in different triage arms.In the rural sites,18.81% (41/218)of the women in the LBC triage arm and 26.46% (127/480)in the VIA/VILI triage arm were referred to colposcopy at baseline screening.To identify one CIN2+or CIN3+lesions,fourteen or twenty-three colposcopies were needed in the direct COLP arm,while three or seven were needed for the LBC triage arm and eight or twenty-six were needed for the VIA/VILI triage arm.In the urban sites,86.76% (354/408) of women in the direct COLP for other hrHPV subtypes+arm and 27.29% (155/568) in the LBC triage for other hrHPV subtypes+arm was referred to colposcopy.To identify one CIN2+or CIN3+lesion,fourteen or forty-four colposcopies were needed in the direct COLP for other hrHPV subtypes+arm,while twelve or thirty-one were needed for the LBC triage for the other hrHPV subtypes+arm.These results were standardized by the direct methods of standardization,and no significant changes were found before and after standardization(Supplementary Table S3).
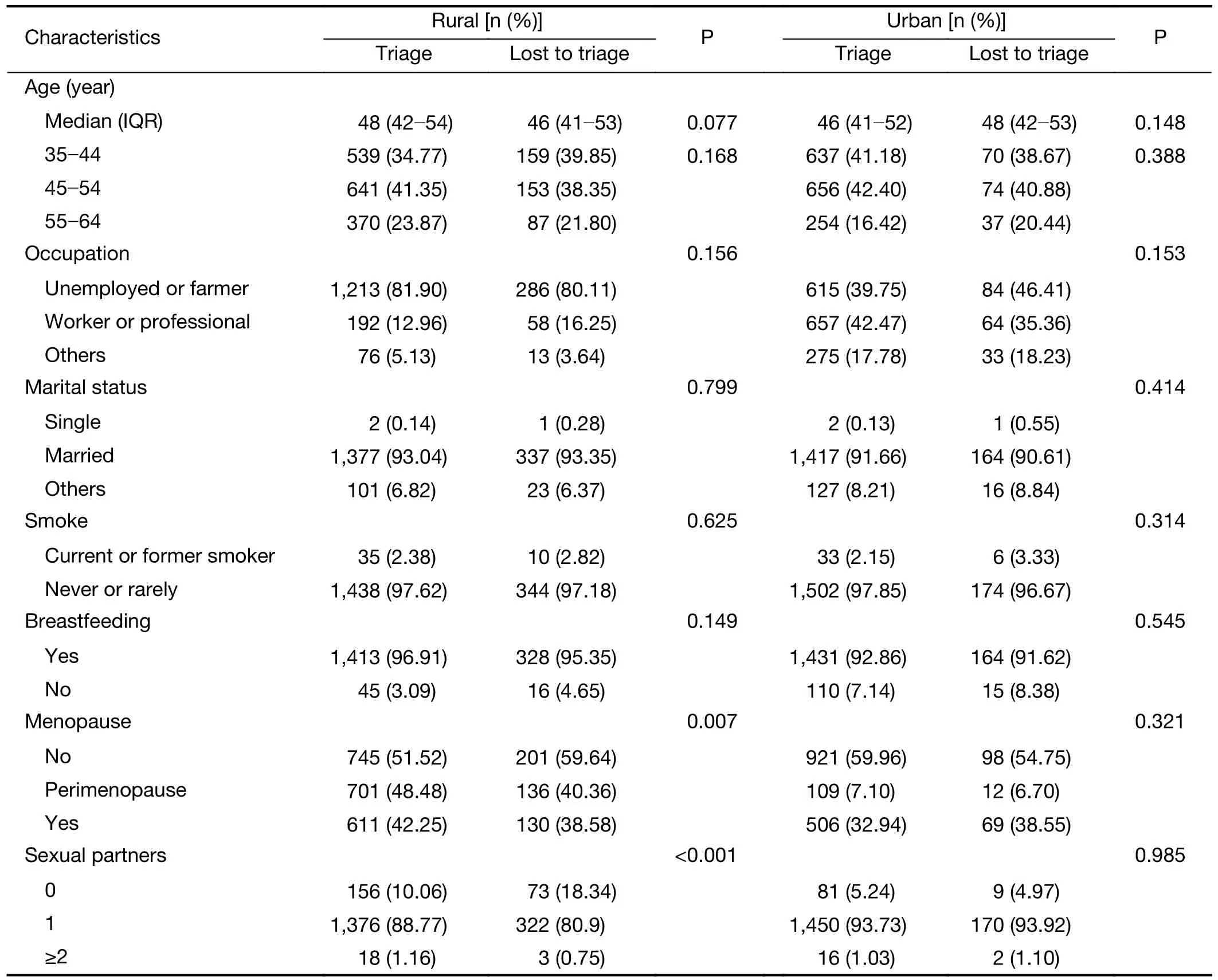
Table S1 Comparison of baseline information between hrHPV-positive women who were triaged and lost to triage
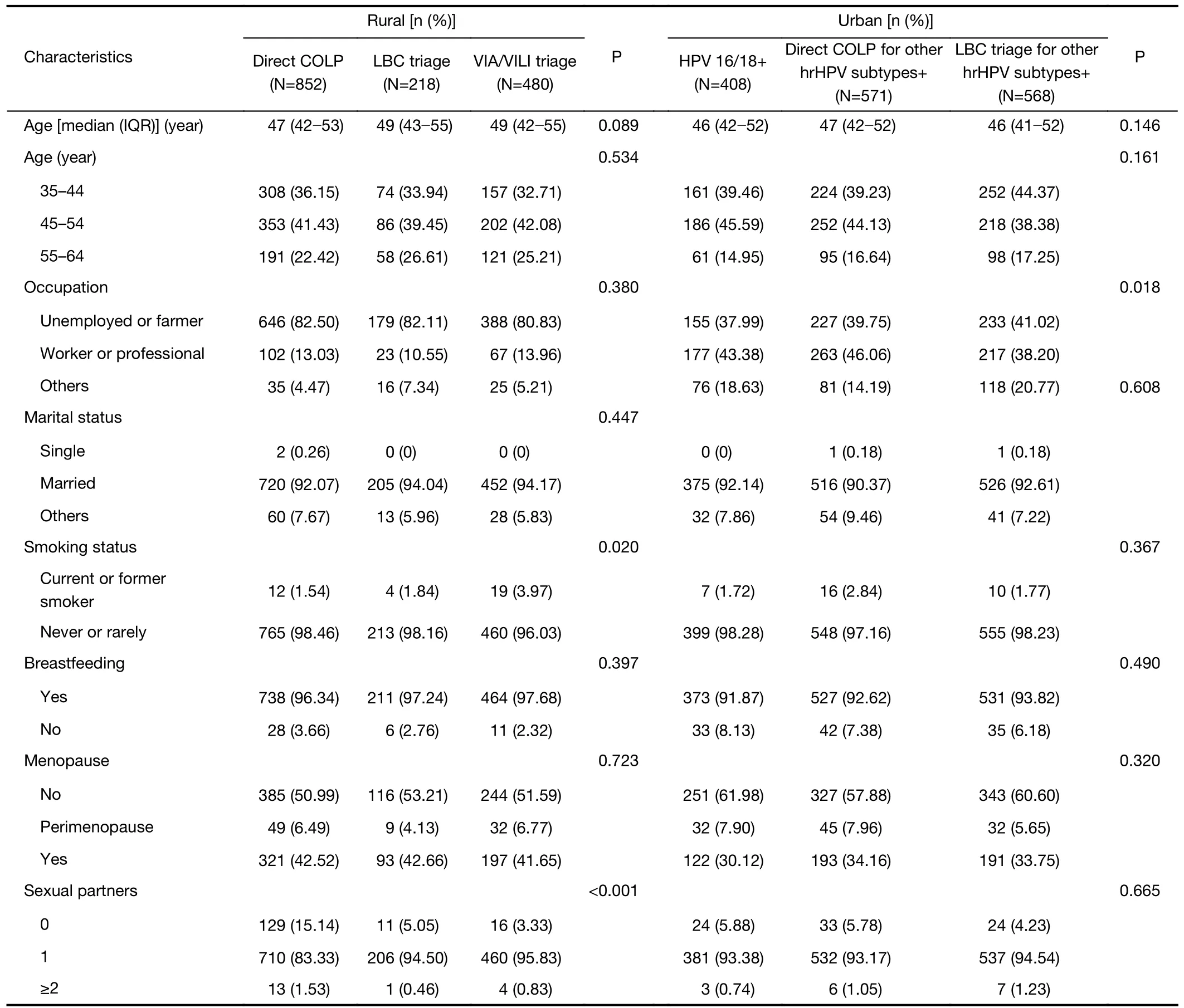
Table 1 Sociodemographic characteristics of hrHPV-positive women included in the analysis

Table 2 Outcomes for different triage arms of hrHPV testing positive in rural sites and urban sites
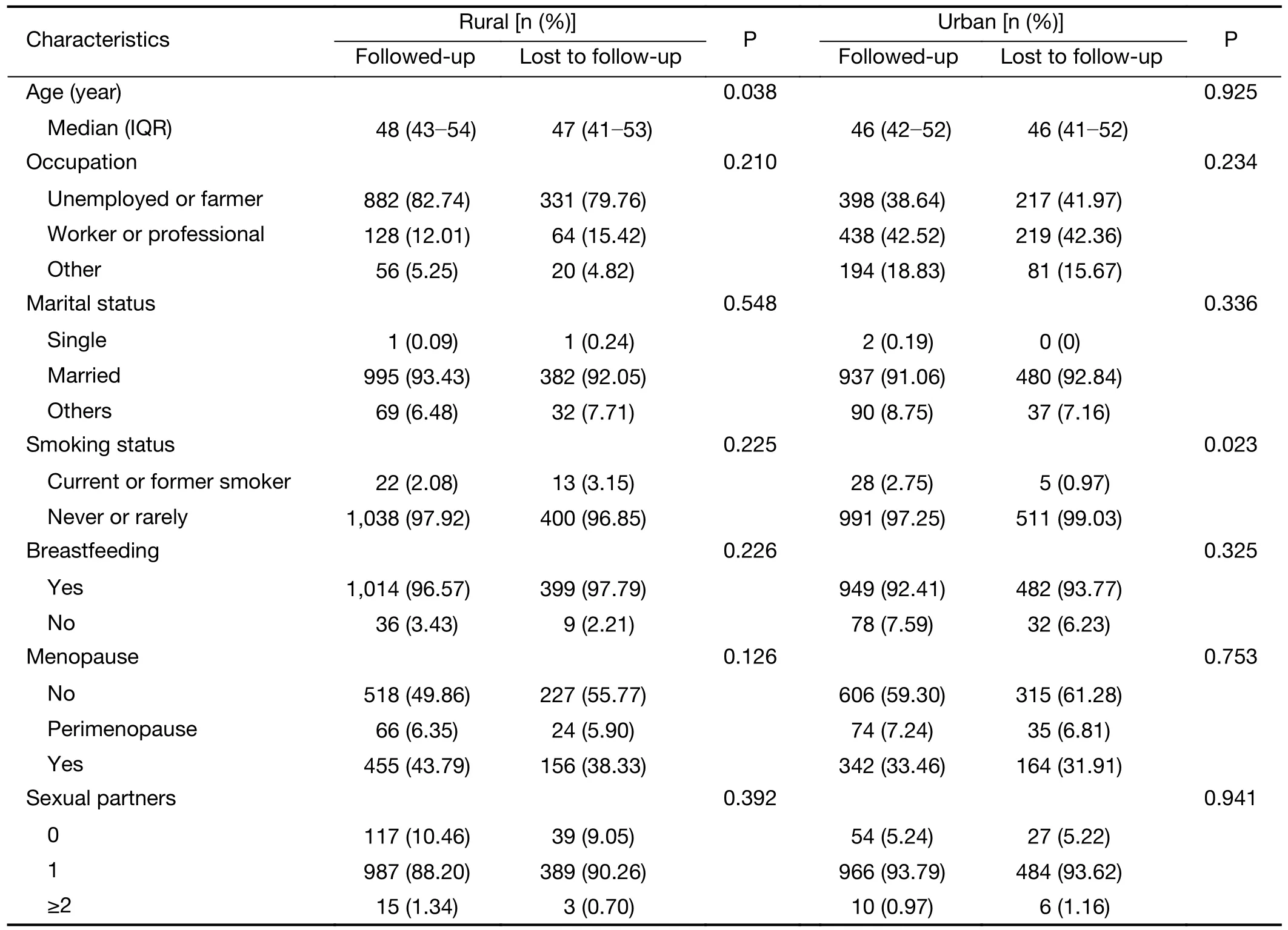
Table S2 Comparison of baseline information between hrHPV-positive women who were followed-up and lost to follow-up
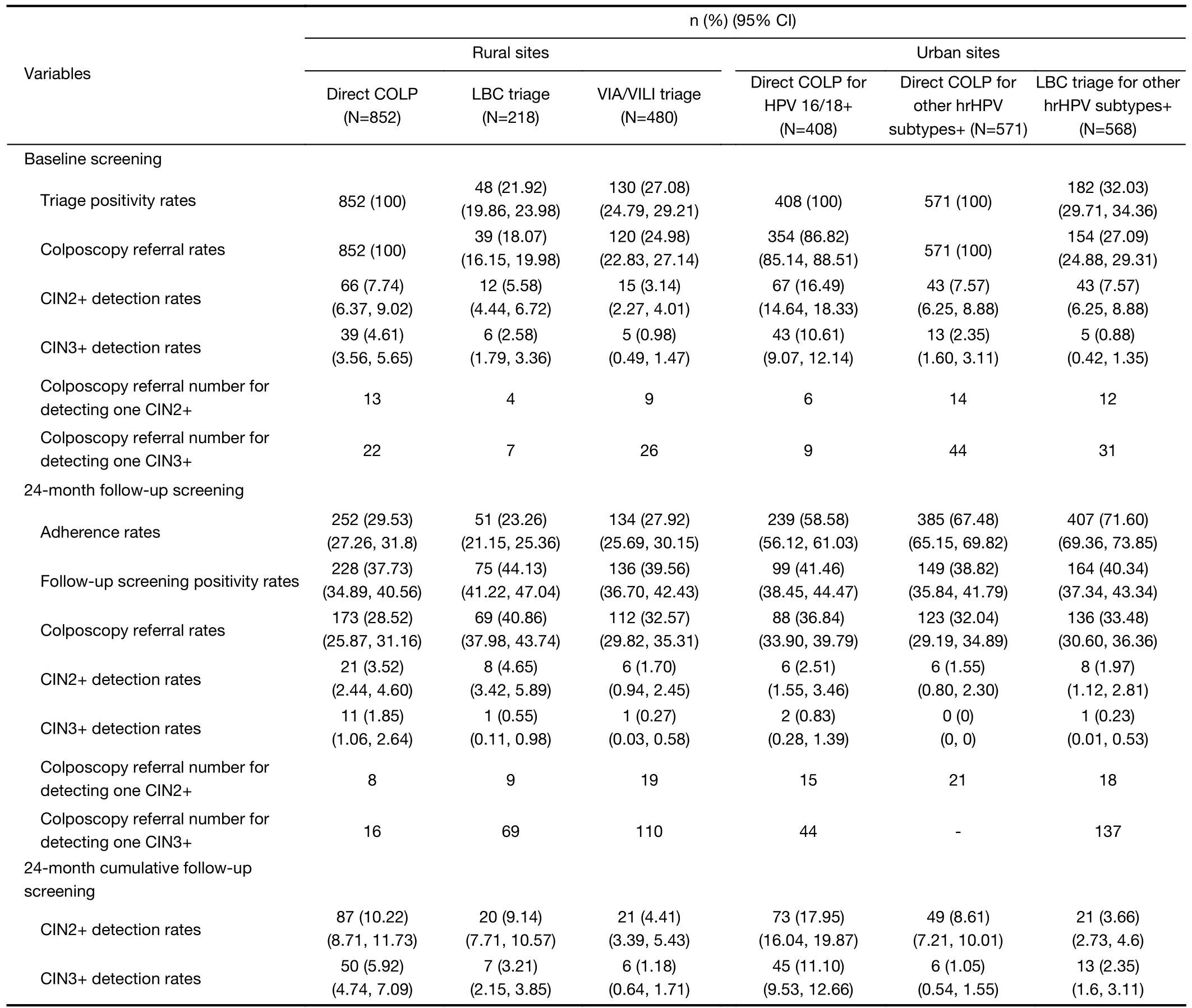
Table S3 Adjusted outcomes for different triage arms of hrHPV testing positive in rural sites and urban sites by direct methods of standardization
Figure 2shows the rates ratio of high-grade CIN detection rates among different triage arms.First,we compared the RR (95% CI) in the baseline and 24-month follow-up screening.In rural site,the VIA/VILI triage arm detected CIN2+significantly less frequently than the direct COPL arm [RR (95% CI),0.46 (0.26,0.81)] at baseline.The disparities disappeared at the 24-month follow-up screening.No distinction was found when we compared the LBC arm and direct COLP arm,or VIA/VILI arm and LBC arm both at baseline and 24-month follow-up.Then,we discovered that the cumulative detection rates for CIN2+were higher in the direct COLP arm and LBC triage arm than in the VIA/VILI triage arm [VIA/VILIvs.direct COLP,RR (95% CI),0.46 (0.28,0.75);VIA/VILIvs.LBC,RR (95% CI),0.50 (0.27,0.94)],but no significant difference was observed between the LBC triage arm and the direct COLP arm [RR (95% CI),0.93 (0.56,1.55)](Figure 2A).Finally,similar results were discovered for CIN3+,except that there were no differences between the LBC triage arm and the VIA/VILI triage arm [RR (95%CI),0.39 (0.13,1.17)] at the 24-month cumulative screening (Figure 2B).
In urban sites,we compared the CIN2+and CIN3+detection rates of the two triage strategies,namely,1)direct COLP for HPV16/18+and LBC triage for other hrHPV subtypes+and 2) direct COLP for HPV16/18+and other hrHPV subtypes+.The detection rates for CIN2+in the LBC triage arm were 0.74 times lower than those in the direct COLP arm [RR (95% CI),0.74 (0.55,1.00)] at baseline screening,but no differences were observed in results for these two strategies at the 24-month follow-up screening [RR (95% CI),1.13 (0.52,2.46)] and 24-month cumulative screening [RR (95% CI),0.78 (0.66,1.17)](Figure 2C).No differences were observed for CIN3+(Figure 2D).
Cumulative detection rate of different triage arms by ages
The results of the 24-month cumulative detection rate for different triage strategies by different age groups are displayed inFigure 3.In rural areas,the 24-month cumulative detection rate for CIN2+was highest in thebaseline LBC triage+arm (31.25%),followed by VIA/VILI triage+(13.85%),direct COLP (9.86%),LBC triage-(2.94%) and VIA/VILI triage-(1.14%) (P<0.001).Among the baseline LBC triage+women,the 24-month cumulative detection rate peaked at 35-44 years and significantly declined for women aged 55-64 years (Ptrend=0.002).In addition,hrHPV+in direct COLP was slightly higher in the 35-44 years old group and 45-54 years old group but declined in the 55-64 years old group (Ptrend=0.057) (Figure 3A).A comparable pattern was observed for CIN3+,but the trend was not statistically significant (Figure 3B).
In urban areas,the 24-month cumulative detection rate for CIN2+was highest in the direct COLP for HPV 16/18+arm (17.89%),followed by direct COLP for other hrHPV+(8.41%),direct COLP for HPV 16/18+and other hrHPV subtypes+with LBC triage+(7.65%),direct COLP for HPV 16/18+and other hrHPV subtypes+with LBC triage-(1.82%) (P<0.001).Among the different triage arms,relatively steady trends were found in the 35-44 years old group and 45-54 years old group,whereas an upward trend was found in the 55+age group,an inverted V-shape was found except in the LBC triage-arm (Figure 3C).The results showed similar patterns for CIN3+(Figure 3D).

Figure 2 Rates ratio of high-grade CIN detection rates (95% CI) among different triage arms at baseline,at 24-month follow-up screening and the 24-month cumulative screening.(A) CIN2+detection rates (95% CI) in rural sites;(B) CIN3+detection rates (95% CI) in rural sites;(C) CIN2+detection rates (95% CI) in urban sites;(D) CIN3+detection rates (95% CI) in urban sites.For Figures 2C and 2D,we compared the CIN2+and CIN3+detection rates of the two triage strategies,namely 1) direct COLP for HPV16/18+and LBC triage for other hrHPV subtypes+and 2) direct COLP for HPV16/18+and other hrHPV subtypes+.95% CI,95% confidence interval;CIN,cervical intraepithelial neoplasia;LBC,liquid-based cytology;COLP,referral to colposcopy without triage;VIA/VILI,visual inspection with acetic acid and Lugol’s iodine.
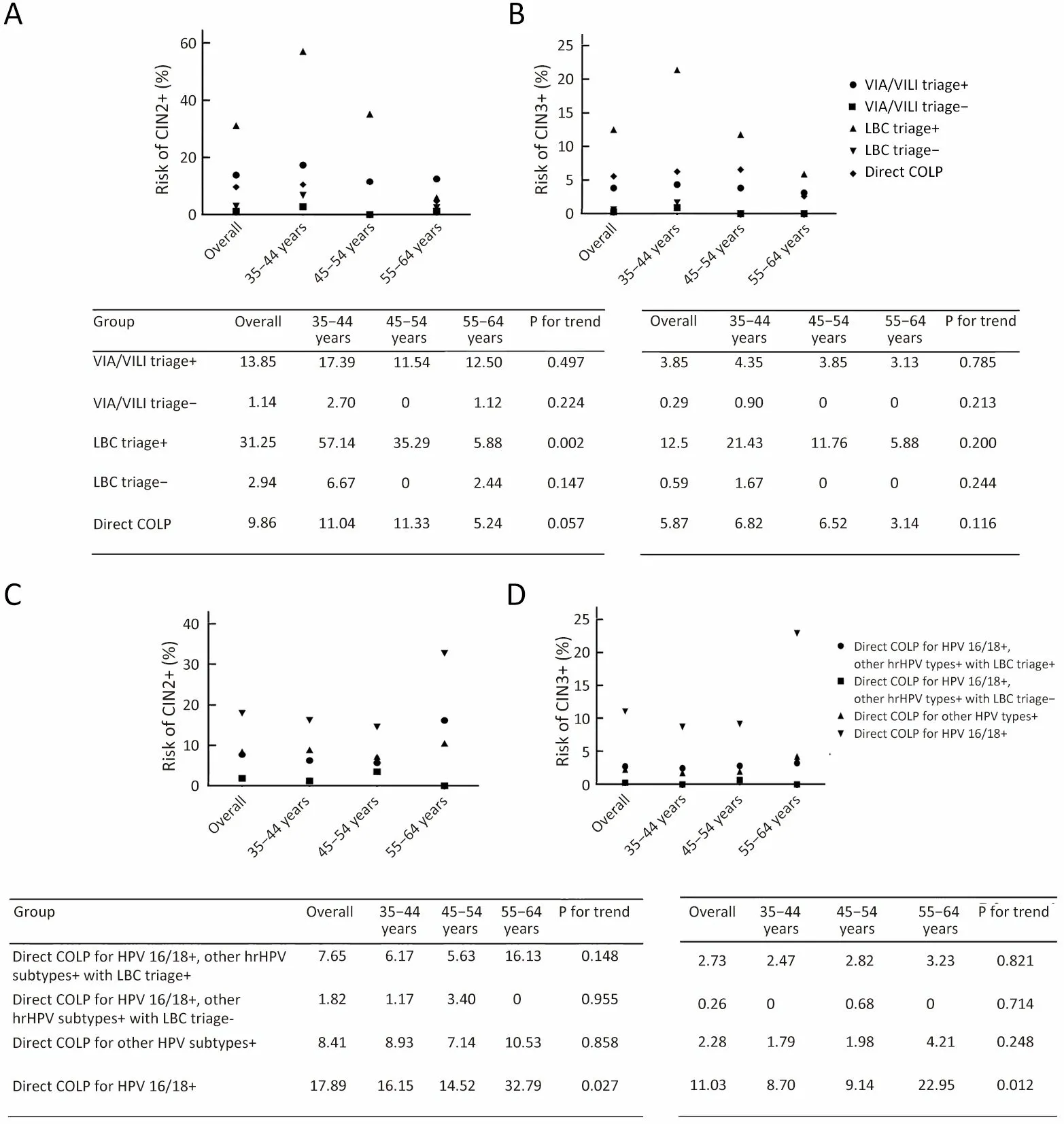
Figure 3 24-month cumulative detection rates of CIN2+or CIN3+among hrHPV-positive women with different triage strategies.(A) 24-month cumulative detection rates of CIN2+in rural sites;(B) 24-month cumulative detection rates of CIN3+in rural sites;(C) 24-month cumulative detection rates of CIN2+in urban sites;(D) 24-month detection rates of CIN3+in urban sites.CIN,cervical intraepithelial neoplasia;VIA/VILI,visual inspection with acetic acid and Lugol’s iodine;LBC,liquid-based cytology;Direct COLP,all hrHPV-positive women were referred to colposcopy directly;hrHPV,high-risk human papillomavirus.
Discussion
The WHO and other guidelines have recommended HPV screening followed by HPV16/18,cytology or VIA as a standard procedure in cervical cancer screening (22-24).Where available,women testing positive for HPV16 or HPV18 genotyping are referred to immediate colposcopy,while the remaining HPV-positive women are recommended to have cytology triage (25,26).For developing countries,two cross-sectional studies and one randomized trial in India and one study in Mexican that evaluated the impact of using cytology or VIA as triage tools for HPV-positive women discovered that while the choice of triage test depends on test availability and affordability in a particular setting,VIA and cytology are currently widely available options for triage of hrHPVpositive women (27,28).Different triage tools have also been evaluated among Chinese women in previous studies(16,18).However,the screening evidence based on a multicenter and prospective study in the real world is still insufficient.
In this study,we applied different triage methods in rural and urban areas to identify the optimal triage strategies based on different economic development and health resource situations.Triage strategies that maximize the detection of high-grade lesions while minimizing colposcopy referral are increasingly viewed as optimal in guideline discussions (18).Rural sites have different needs for triage strategies because their health provider and clinical resource capacity is limited and calling the women,especially elderly women,back for triage tests is challenging.Besides,hrHPV primary screening would inevitably increase the burden of colposcopy service if no appropriate triage strategy were applied.Therefore,it is necessary to adequately and accurately distinguish hrHPVpositive women who are truly in need of colposcopy referral to distribute the limited resources reasonably and efficiently (18,21).At baseline screening in rural sites,triage by LBC or VIA/VILI significantly reduced the number of colposcopies.It has also been generally observed that the LBC triage strategy was almost 2-3 times higher detection rates of CIN2+and CIN3+than VIA/VILI triage strategy but did not show a significant reduction in comparison with those the direct COLP strategy.Compared to all other triage strategies,LBC triage showed the highest colposcopy efficiency with the significantly less number of colposcopies to identify per CIN2+and CIN3+case.Likewise,to identify one CIN3+lesion,7 and 23 colposcopies were needed in the LBC triage strategy and direct COLP strategy,respectively.In addition,there are currently limited data on optimal triage strategies that can distinguish hrHPV-positive women who are at high risk of developing high grade cervical lesions from those who are at lower risk that ensuring them safely return to routine screening (17).Our results revealed that when LBC triage positive,women had remarkably increased risks of developing CIN2+and CIN3+than the risks provided by VIA/VILI triage or direct COLP without triage.The 24-month cumulative detection rate results were consistent with those of a pooled study from a large Chinese population,indicating that cytology was superior to VIA/VILI for triage among HPV-positive women (18).However,the 24-month cumulative detection rate of CIN3+among HPV-positive women triaged by cytology or VIA/VILI in mentioned pooled study was higher than those of in our study.One possible reason is that the cohort population in previous study was co-tested by LBC,VIA and HPV test.Moreover,it is known that the performance of cytology is varies between countries and settings and depends on the medical infrastructure of a particular region as well as the cytologist’s diagnosis experience.Intensive quality control in cytological diagnosis by experienced cytologists might be the explanation for the high proportion of abnormalities detected through cytology triage in the pooled study.While the fact that all screening procedures were conducted by local health providers resulted the relatively lower detection rates,representing the average level of cytology quality nationwide.Therefore,there is also a practical consideration regarding the LBC triage strategy is that although the national program developed and facilitated local healthcare ability by improving infrastructure and personnel training,the numbers of qualified cytologists and gynecologists still need to be increased (29).
Previous studies have demonstrated that the clinical performance of VIA/VILI as a primary method maybe not satisfactory for cervical cancer (18,30).In the latest WHO recommendation,it has been also recommended to use VIA as a triage tool rather than a primary screening method(22).In our study,although VIA/VILI triage for hrHPVpositive women reduced the referrals for colposcopies,the cumulative detection rates of CIN2+and CIN3+were declined remarkably,indicating the considerable number omission diagnosis.In addition,the cumulative detection rates of CIN2+and CIN3+when VIA/VILI+triage were almost 10 times higher (13.85%,1.14%) than those of hrHPV-positive women with negative VIA/VILI.However,VIA/VILI as a triage method had a higher detection rate of CIN2+and positive predictive value in comparison with cytology triage in high-incidence sites in Shanxi Province,where health providers had enriched experience with VIA/VILI for cervical cancer screening(31).Subjectivity is one of the main disadvantages of the VIA-based screening method,but these can probably be alleviated through well-defined VIA criteria or by welltrained health providers to assure the quality of the method.Therefore,VIA/VILI might be inferior to more sensitive methods but could be applied in areas with limited health resources;however,further improvements are still needed.
In China,women who live in urban regions have more access to opportunistic screening for cervical cancer,which currently includes cytology or HPV genotyping test (5).Genotyping for HPV16,HPV18,or both has been proposed as a triage tool because these two HPV genotypes are associated with approximately 70% of all invasive cervical carcinomas (32),and this proportion was almost 85% in China (33).In this study,the 24-month cumulative detection rates of CIN2+with HPV16/18+were highest in urban areas,surpassing hrHPV subtypes+with LBC triage+(17.89%vs.7.65%),which is also consistent with the findings of the ATHENA study in America (26).HPV16/18+referred to colposcopy and LBC triage for other subtypes-positive has been judged useful and has been recommended for the management of hrHPVpositive women in high-income countries (26,34).In our study,we also found that the 24-month cumulative detection rates of CIN2+and CIN3+from direct COLP for HPV 16/18+and other hrHPV subtypes+with LBC triage+were much greater than those from the direct COLP strategy for hrHPV-positive women without triage.Also,direct COLP strategy increasing colposcopy will lead to overdiagnosis and waste of limited resources.Moreover,a previous study with ten screening strategies determined that HPV testing with immediate referral to colposcopy gave the highest sensitivity of 89% but also the highest false-positive rate of 38% (35).In this context,regarding the management of women with hrHPV genotypingpositive,our study further found that direct COLP for HPV 16/18+and other hrHPV subtypes+with LBC triage may be promising in urban sites in China with the appropriate conditions.These findings are also in line with the present understanding and recognition that triaging of HPV-positive women with HPV16/18 genotyping and cytology provides a good balance between maximizing sensitivity and specificity by limiting the number of colposcopies (19,35).
We also note that age of screened women has considerable influence on the screening performance.For rural sites,the 24-month cumulative detection rate of CIN2+for LBC triage+and VIA/VILI triage+women was higher in 35-44 years old women than in the other two age groups,and the performance characteristics for CIN3+were similar.It is reasonable to speculate that sexually active women aged 35-44 years old are at high risk of HPV infection and cervical lesions.In addition,LBC triage+and VIA/VILI triage+women had relatively lower cumulative detection rates among those over 45 years old,especially LBC triage-positive women aged over 55 years old.These results are consistent with a randomized study in India and a pooled analysis in China that showed VIA-based screening may be less effective for women older than 40-50 years or postmenopausal women due to natural changes in the anatomy of the cervix,which limits visual diagnosis(27,36).Elderly women,especially postmenopausal women whose transformation zone cannot be fully seen and who have epithelial atrophy,may have an increased risk of outcome misclassification in LBC (37).Some studies have also suggested that lesions in elder women may not be recognized by cytology due to the disappearance of the transformation zone (38).Another possible explanation for the high cumulative detection rates might be common cervicitis and vaginitis among rural women,which could lead to low-quality cytological slides and affect the exposed cervix (18).However,in urban sites,all triage strategies had significantly increased cumulative detection rates of CIN2+and CIN3+in the 55-64 years old age group,which mainly associated with different immune responses and sexual behavior.There is a study which proved that many newly diagnosed cervical cancers are found among women over 60-65 years of age (39).One possible factor contributing to the difference in relative effectiveness of HPV testing and cytology is the second peak of HPV infection in women over 50 years old,which has been observed in China and Western Africa (40,41),and urban areas has relatively much qualified cytologists.Nonetheless,all these triage strategies may have limitations for elderly women.Hence,agespecific effectiveness must be carefully considered.
Limitations and advantages
Our study has several advantages as follows: First,because all procedures were conducted by local health providers,our study reflects real-world clinical practice in rural and urban areas,thus providing important guidance on optimal triage strategies for different settings.Furthermore,to our knowledge,this study is the only multicenter,randomized trial with a large population to evaluate the triage performance of the VIA/VILI,LBC and direct COLP screening tests as hrHPV-positive management methods that are currently available and accessible for the Chinese population.
Some limitations are also worth noting.First,the triage strategies increased the risk of sample attrition in follow-up steps.The triage test was the second screening step,which means that hrHPV-positive women had to be recalled for triage tests after receiving the primary result,except for serious lesions observed at the first step.Second,although we planned to set the triage arms by 1:1:1,but four sites did not have the ability of LBC diagnose.These women were allocated to VIA/VILI or direct COLP arm by 1:1.Therefore,there were only 218 women included in the LBC arm.Besides,women who were allocated to VIA/VILI or LBC arm would have to be transferred to coloscopy if positive,the women would be called back again.As a result,the adherence rate of the VIA/VILI and LBC arm would be lower than that of the direct coloscopy arm.Even so,our study provided the evidence of the real situation and efficacy of LBC and VIA/VILI triage for hrHPV positive women.Thirdly,the first HPV vaccine was marketed in 2017 in China,and participants in this study were unlikely to be vaccinated,which restricts the extrapolation of the results interpretation among vaccinated population.Consequently,immunization status and longitudinal data with multiple rounds of follow-up screening are warranted in the future.
Conclusions
Different settings should select feasible triage strategies based on local capability,and benefits and harms should be considered when HPV testing program was introduced optimally into national cervical cancer screening.Our study demonstrated that LBC triage for hrHPV-positive women in rural settings and direct COLP for HPV16/18+women and LBC triage for other hrHPV-subtypes+women in urban settings are promising and feasible choice in China.Therefore,well-trained cytologists and significant investment in quality assurance by a national screening program are urgently needed.VIA/VILI still might be an option in low healthcare resource settings with limited cytologists and facilities,but the quality of VIA is still challenging.Meanwhile,faster,more accurate,effective,and affordable triage tests,such as biomarker-based and artificial intelligence-based methods,should be developed for more precise management of hrHPV-positive women in different resource settings.
Acknowledgements
This study was funded by National Health Commission(formerly Health and Family Planning Commission) of China (No.201502004);CAMS Innovation Fund for Medical Sciences (CIFMS) (No.2021-I2M-1-004) and the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No.2019PT320010 and No.2018PT32025).
Footnote
Conflicts of Interest: YL Qiao and JH Lang have received speakers’ fees and non-financial support from QIAGEN,China,from Roche,Diagnostics (Shanghai) Ltd,and from Hologic Inc.USA,outside the submitted work.They have NOT received any royalties,nor have Intellectual Property/Patent/Stock holdings with these companies.All other authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2022年5期
Chinese Journal of Cancer Research2022年5期
- Chinese Journal of Cancer Research的其它文章
- Characteristics of lymph node stations/basins metastasis and construction and validation of a preoperative combination prediction model that accurately excludes lymph node metastasis in early gastric cancer
- Correlation between imaging features on computed tomography and combined positive score of PD-L1 expression in patients with gastric cancer
- Colorectal cancer burden,trends and risk factors in China:A review and comparison with the United States
- Myeloid checkpoints for cancer immunotherapy
- National guidelines for diagnosis and treatment of malignant lymphoma 2022 in China (English version)
- Beyond images: Emerging role of Raman spectroscopy-based artificial intelligence in diagnosis of gastric neoplasia
