Assessment of the differences in the short-term clinical outcomes of superotemporal and inferonasal Baerveldt glaucoma implantation surgeries performed via the pars plana route
Abstract
?KEYWORDS:Baerveldt glaucoma implant; intraocular pressure; superotemporal; inferonasal; pars plana route
INTRODUCTION
The effectiveness of glaucoma drainage implants (GDIs)in reducing intraocular pressure (IOP) have been reported in patients with refractory glaucoma[1-6]. GDIs have the Molteno implant (Molteno Ophthalmic Ltd, Dunedin, New Zealand), the Baerveldt glaucoma implant (BGI) (AMO, Santa Ana, California, USA), and the Ahmed glaucoma valve (New World Medical, Rancho Cucamonga, California, USA). The BGI Plate are larger relative to the Ahmed and the Molteno. Most BGI procedures are performed in the superotemporal quadrant, making the placement of the BGI plate easier as shown in the figures as the rectus muscles are more easily exposed in this location than the other quadrant (Figures 1 and 2).
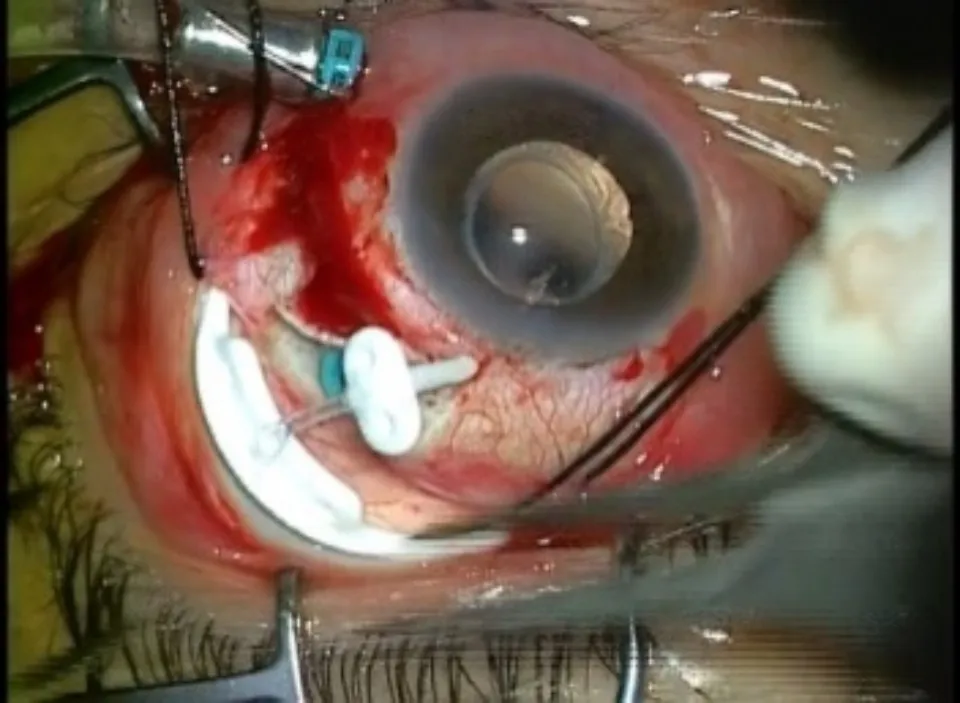
Figure 1 The BGI insertion in the superotemporal quadrant (The insertion space is wider).
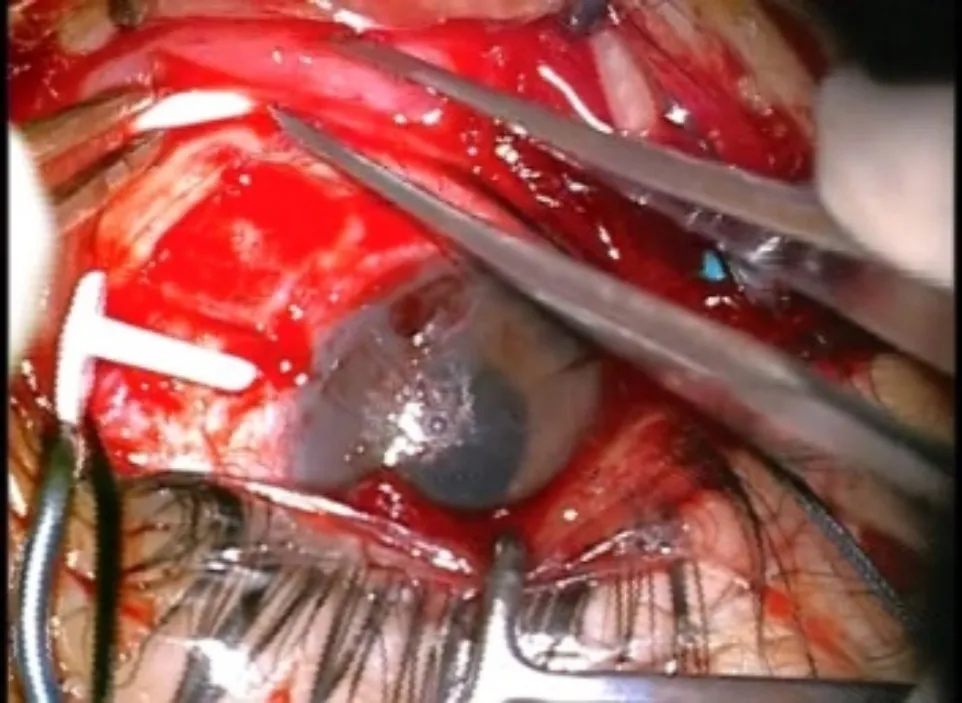
Figure 2 The BGI insertion in the inferonasal quadrant (The insertion space is narrower).
It is unfortunate that the sclera, and/or conjunctiva is often scarred from previous surgeries of the superotemporal quadrant in the eyes with refractory glaucoma. Conversely, the inferior conjunctiva is often kept from incision nevertheless the superior conjunctiva was scarred in the eye. A previous report has demonstrated that IOP reduction was recorded after inferonasal BGI surgery[7]and we considered that the difference in the insertion area of the plate might affect the filtration area around the plate, but there are no reports on whether the BGI insertion area affects IOP reduction. Therefore, the aim of this study was to evaluate the difference between superotemporal and inferonasal BGI surgeries in terms of IOP reduction for patients with neovascular glaucoma (NVG).
SUBJECTS AND METHODS
EthicalApprovalThe study was performed in accordance with the tenets of the Declaration of Helsinki. The ethics committee of Toho University Sakura Medical Center approved the protocol for this retrospective study (approval number S16047). In accordance with the clinical research guidelines of the Japanese Ministry of Health, Labour, and Welfare, the study design was explained to subjects using the hospital’s website.
We reviewed retrospectively the medical records of all patients who underwent BGI surgery for the treatment of NVG at Toho University Sakura Medical Center between June 2015 and April 2018. Because the type of glaucoma affects the IOP reduction of the BGIs, we only included NVG cases in our study to minimize the variations[8-10]. All the patients were followed up for 12mo after surgery. Patients observed during shorter period or undergoing another glaucoma surgery during the follow-up period were excluded. The included cases were divided into two groups as follows: the superotemporal insertion group, which included 18 eyes in 16 subjects (13 males, 3 females; mean age 62.9±14.4 years), and the inferonasal group, which included 17 eyes in 15 subjects (11 males, 4 females; mean age 56.9±10.7 years).
In the current study, the number of anti-glaucoma medications used by the patients was counted using the following criteria: mono-component medication drop equals one medication, double-component medication drop equals two medications, and oral anti-glaucoma agent equals two medications because a previous study reported that the effect of a combination of drugs is equal to that of an oral anti-glaucoma drug[11]. We determined successful cases with BGI surgery that cases when the postoperative IOP was between 6 and 22 mmHg, without the use of oral anti-glaucoma medications, visual acuity at the final visit with light perception or better, and when further glaucoma surgeries were not needed. The IOP (measured with a Goldmann applanation tonometer), visual acuity, and the number of anti-glaucoma medications administered at 12mo visit were compared with the values recorded at the preoperative visit. The IOP was measured 3 times at the same visit and the mean value was recoreded. Visual acuity was measured by decimal visual acuity and then converted the LogMAR visual acuity. The IOP and the number of anti-glaucoma drugs used before and after surgery, and the IOP reduction rate at 12mo after operation relative to preoperative IOP was compared between the superotemporal and inferonasal groups.
BaerveldtGlaucomaImplantSurgeryWe performed BGI surgery similar to the method mentioned before[12]. The incision was designed along the corneal limbus of conjunctiva exposed, either the superior and lateral recti muscles or the inferior and medial recti muscle, depending on the chosen point of insertion of the plate following the administration of Sub-Tenon’s anesthesia. The insertion area was decided at the operator’s discretion depending on the condition of the conjunctiva in each case. Following the creation of A 6×6-mm fornix-based lamellar scleral flap in the superotemporal quadrant or inferonasal quadrant, an infusion cannula was placed in the inferotemporal quadrant to prevent the collapse of eye ball during the BGI surgery. The other two ports were created under the scleral flap on the same side if the scleral flap was made in the superotemporal quadrant and on the conjunctiva of the other side if the flap was made in the inferonasal quadrant. Pars plana vitrectomy was performed if the vitreous was present. Additional endophotocoagulation was performed in all cases. The BGI tube was knotted using an 8-0 polyglactin suture thread to prevent excessive outflow until plate encapsulation and insertion beneath the lateral and superior recti muscles in the superotemporal quadrant or beneath the medial and inferior recti muscles in the inferonasal quadrant were completed. Following anchoring the anterior edge of the plate to the sclera, a sclerotomy was made at 3.5 mm from the limbus under the lamellar scleral flap with a 20-gauge V-lance. The Hoffmann elbow and tube were inserted through the sclerotomy port and fixed in place with an 8-0 nylon thread. The Hoffmann elbow was then covered with the scleral flap, which was sutured closed with a 10-0 nylon thread. To avoid early postoperative elevation of IOP, a Sherwood slit was made using a microblade. Finally, the infusion cannula was removed, and the sclera was covered with the conjunctiva again with a continuous suture (Figure 3).
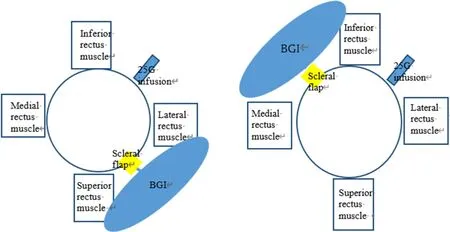
Figure 3 The plate was placed between the inferiorl rectus muscle and the medial rectus muscle A: the insertion of BGI in the superotemporal quadrant. The plate was placed between the lateral rectus muscle and the superior rectus muscle; B: the insertion of BGI in the inferotemporal quadrant.
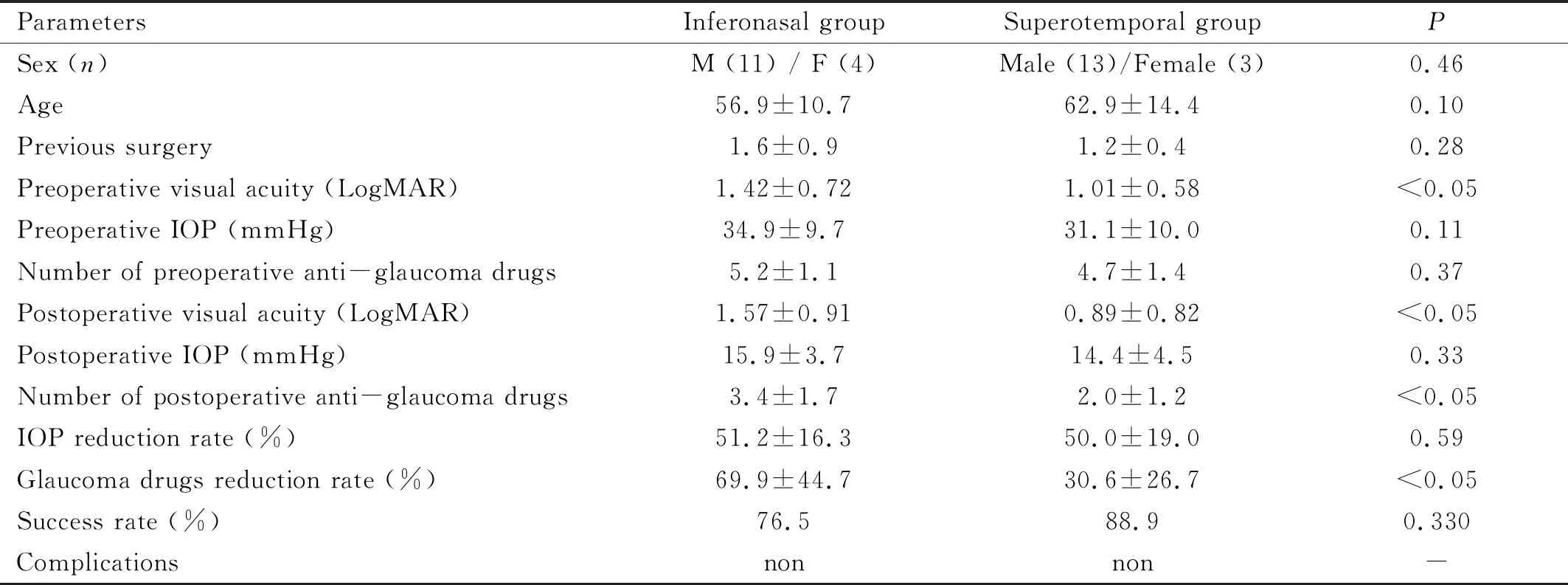
Table 1 Demographic and clinical characteristics
StatisticalAnalysisAll statistical analyses were performed using Statcel software (OMS, Saitama, Japan). AP<0.05 was considered statistically significant. Fisher’s exact test was used to compare sex-related differences. Mann-Whitney U-test was used to assess the difference in the IOP values, the number of previous surgery and the number of anti-glaucoma medications used between the superotemporal group and the inferonasal group. A pairedt-test was used to assess the difference in the LogMAR visual acuity, the IOP values, and the number of anti-glaucoma medications used before and after surgery. The student’st-test was used to assess the difference in the IOP reduction rate.χ2test was used to assess the difference in the success rate.
RESULTS
The number of previous surgeries was 1.2±0.4 times in the superotemporal group and 1.6±0.9 times in the inferonasal groups (Mann-WhitneyU-test,P=0.28) (Table 1). The type of previous surgery was simple vitrectomy, cataract surgery, phacovitrectomy, and trabeculectomy. One case in the superotemporal group underwent a combined vitrectomy/BGI procedure on both eyes. The remaining eyes underwent BGI alone because they were vitrectomized eyes. The mean visual acuity in the superotemporal group was 1.08±0.58 at the first visit and 0.89±0.82 at 12mo follow-up (Pairedt-test,P=0.18) (Table 2). The mean visual acuity in the inferonasal group was 1.42±0.72 at the first visit and 1.57±0.91 at the 12mo follow-up visit (pairedt-test,P=0.95) (Table 2). The mean IOP in the superotemporal group was 31.1±10.0 mmHg at the preoperative visit and 14.4±4.5 mmHg at the 12mo follow-up (Pairedt-test,P<0.05) (Figure 4, Table 2).
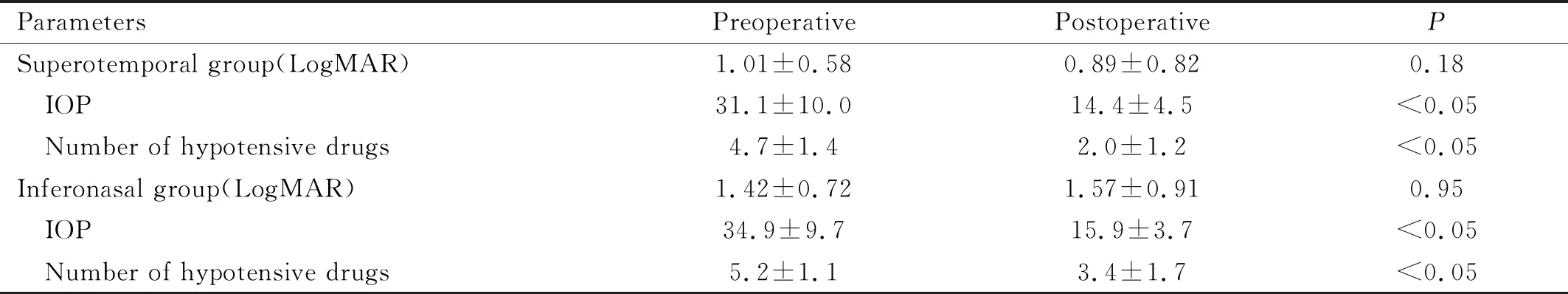
Table 2 LogMAR, IOP, and the number of hypotensive drugs between preoperative and postoperative
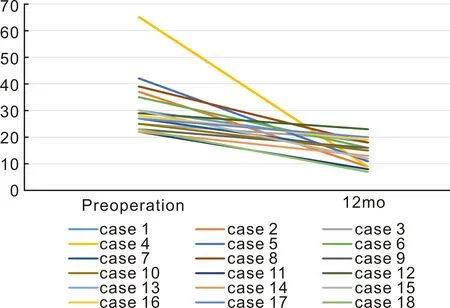
Figure 4 IOP values of the superotemporal group.
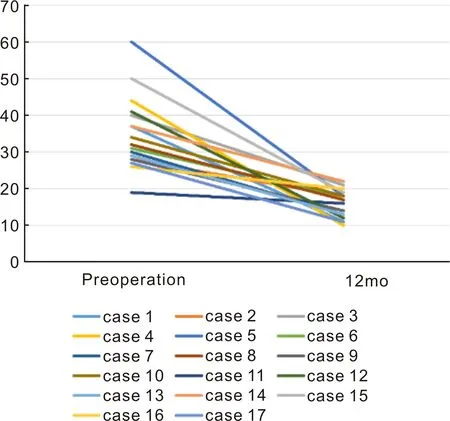
Figure 5 IOP values of the inferonasal group.
The mean IOP for the inferonasal group was 34.9±9.7 mmHg at the preoperative visit and 15.9±3.7 mmHg at the 12mo follow-up (Pairedt-test,P<0.05) (Figure 5).
Surgery significantly reduced the number of anti-glaucoma medications used in the superotemporal group, from 4.7±1.4 medications before surgery to 2.0±1.1 medications after surgery (Pairedt-test,P<0.05) (Figure 6).
Surgery significantly reduced the number of anti-glaucoma medications used in the inferonasal group as well, from 5.2±1.1 medications before surgery to 3.4±1.7 medications after surgery (Pairedt-test,P<0.05) (Figure 7).
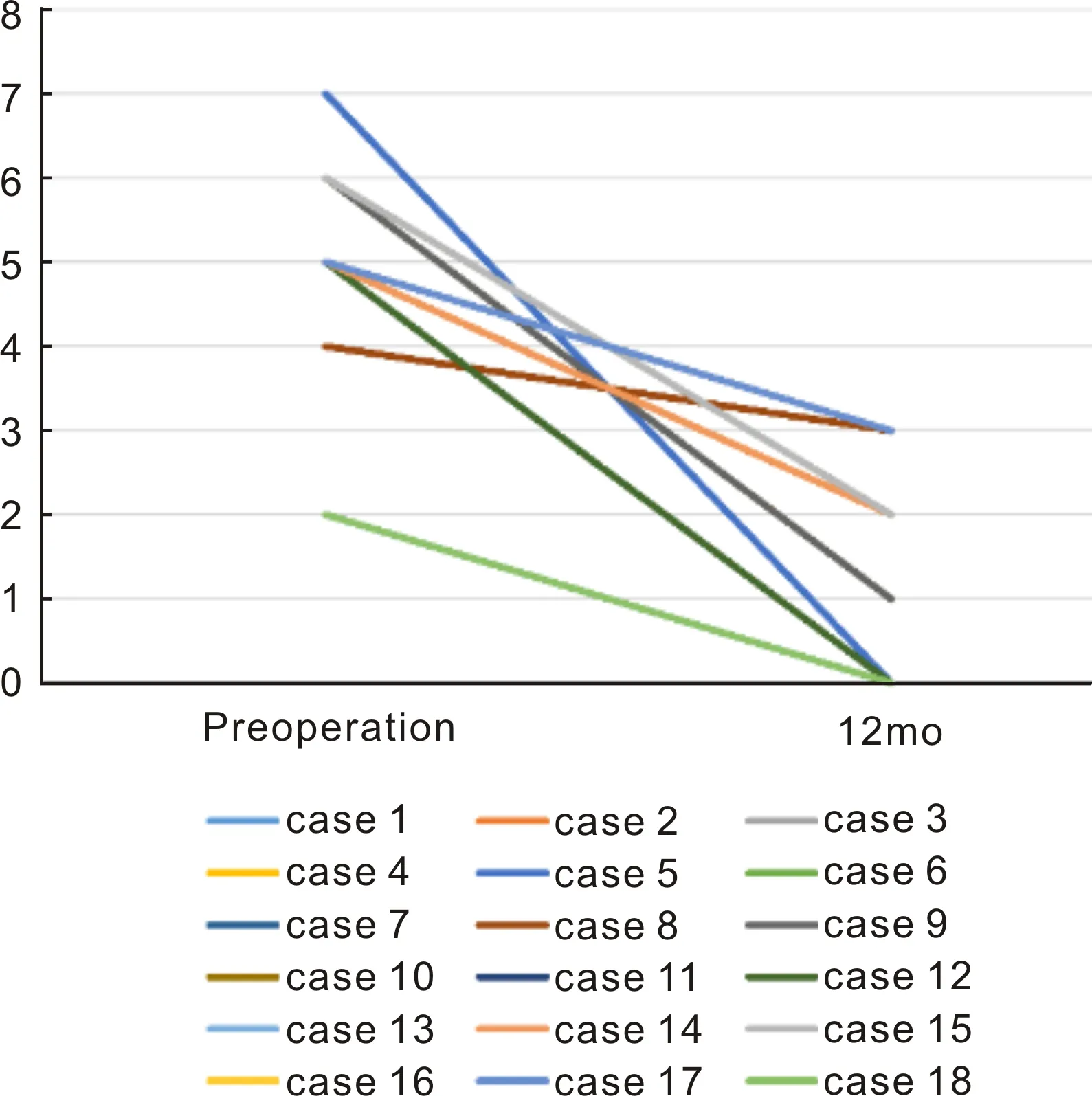
Figure 6 Number of anti-glaucoma drugs used by the patients in the superotemporal group.
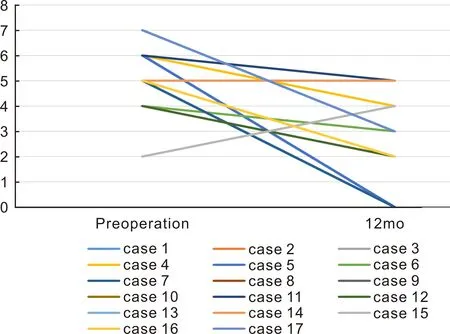
Figure 7 Number of anti-glaucoma drugs used by the patients in the inferonasal group.
The IOP reduction rate of the superotemporal group was (50.0±19.0)% and that of the inferonasal group was (51.2±16.3)%. There was no significant correlation between the two groups (Student’s-ttest,P=0.590) (Table 1). The glaucoma drugs reduction rate of the superotemporal group was (30.6±26.7)% and that of the inferonasal group was (69.9±44.7)%. There was a significant correlation between the two groups (Student’s-ttest,P<0.05). We classified BGI surgery as successful in 16 out of 18 (88.9%) cases in the superotemporal group and 13 out of 17 (76.5%) cases in the inferonasal group. There was no significant correlation between the two groups (χ2-test,P=0.330). There were no surgery-related complications, such as exposure of the tube and plate or endophthalmitis, in all cases by slit-lamp examination.
DISCUSSION
The benefit of insertion of GDIs in the inferonasal quadrant has been reported in several reports[7,13]. Readetal[14]evaluated a cohort of patients who received a Molteno implant (previously reported by Millsetal[15]) and found no difference in clinical outcomes based on plate location. Kara et al. reported that inferonasal BGI placement appeared to be safe and they suggested this as an alternative method in certain clinical situations[7]. Different from the Ahmed valve, the BGI plate is generally inserted under the extraocular recti muscles because the size of the plate is 350 mm2, which is bigger than the plate used for Ahmed glaucoma valve surgery. Moreover, the procedure of inserting the BGI plate into the inferonasal quadrants is difficult than that of the superotemporal depending on the extraocular muscle of the adhesion area. The adhesion areas of the extraocular muscles are 5 mm from the limbus for the superior rectus muscle, 7 mm from the limbus for the inferior rectus muscle, 6 mm from the limbus for the medial rectus muscle, and 9 mm from the limbus for the lateral rectus muscle. Therefore, BGI placement locations, in order of preference, are as follows: superotemporal quadrant, inferotemporal quadrant, inferonasal quadrant, and superonasal quadrant. Because the insertion area is wide and easily exposed in this location, making the placement of the BGI plate easier, BGI procedures are usually performed in the superotemporal quadrant[16-17].
The previous report has demonstrated that the aqueous humor is absorbed by the fibrous capsule around GDI plates[18]. GDIs sometimes fail to control IOP, and after a period of time, may have their IOP-lowering effect decreased due to further scarring and thickening of the fibrous capsule around the plate[17,19-22]. We considered that the area of the BGI plate covered under the muscle in the inferonasal quadrant is larger than that in the superotemporal quadrant; this affects the formation of the fibrous capsule and can influence IOP reduction depending on the insertion area.
In the present study, we examined the difference in the effectiveness of IOP reduction between inferonasal and superotemporal BGI. Previous studies that examined GDI implants in eyes with NVG reported successful proportion as 60%[8-9]. In contrast, the IOP remained sufficiently reduced in 84.6% of patients one year following GDI placement in the superotemporal quadrant[10]. Since the type of glaucoma affects the result of IOP reduction, we assessed only NVG cases in the present study. The results of the present study showed that there was no significant difference in IOP reduction for NVG between the inferonasal and superotemporal groups. This might lead to considering that the formation of the filtration bleb of BGI was not easily affected by the extraocular muscle. Fluid collections and endoplate characteristics are easily visualized with MRI[18]. Further studies involving the use of MRI for the measurement of the fibrous capsule around the BGI plate are needed.
The rapeutic management of NVG includes panretinal photocoagulation and vitrectomy; however, NVG occurrence after vitrectomy for proliferative diabetic retinopathy has been reported[23-24]. Making a scleral flap for BGI in the superotemporal quadrants is often difficult because a three-port vitrectomy causes scleral and/or conjunctival damage in these quadrants during the vitrectomy. Additionally, glaucoma filtration surgery is generally performed in the superior side to prevent possible endophthalmitis. The superotemporal quadrant could not be used for BGI surgery in eyes which previously underwent vitrectomy or glaucoma surgery.
This study has several limitations. First, the current study has a small number of cases in both groups. A study with a large sample size is needed in the future. Second, the visual acuity in the inferonasal group was worse than that in the superotemporal group. This indicates that the preoperative state might have differed between the two groups. Further studies with the two groups in the same preoperative state are needed. The third is the interpretation of the difference in the anti-glaucoma drug reduction after the operation. The drug reduction rate of the superotemporal groups was significantly higher than that of the inferonasal groups in the current study. It is difficult to assess how one medication to concrete degree of IOP reduction. However, the difference in the reduction of the anti-glaucoma drugs did affect the IOP after the operation. Considering this, the IOP reduction of the superotemporal groups might be higher than that of the inferonasal groups. In a future study, assessment of the IOP reduction considering the number of hypotensive drugs is needed. Finally, the follow-up period was only one year in the present study. The surgical outcomes of the inferonasal and superotemporal BGI procedures were not different; however, complications such as exposure of the silicone tube may occur during the late postoperative period. Tube exposure can lead to ocular inflammation, hypotony, poor vision, and phthisis bulbi and represents a major risk factor for the development of late endophthalmitis, with the exposed tube providing a pathway for organisms to enter the eye through the ocular surface. Pakravanetal[25]found more significant complications, including tube exposure, with Ahmed glaucoma valve implants placed inferiorly (25%) as compared to those placed superiorly (5.2%) in their study of 106 eyes assessed for an average follow-up period of 10.58±6.75mo. Levinsonetal[26]also found that implants placed inferiorly were more frequently exposed (15.6%) as compared to implants placed superiorly (6.3%). Therefore, studies with longer follow-up periods are needed to assess long-term risks for plate exposure and elevated IOP following inferonasal BGI placement.
In conclusion, the results of the present study suggest that there is no difference in the short-term clinical outcomes between superotemporal and inferonasal BGI surgeries performedviathe pars plana route. Therefore, the first choice of the BGI insertion is the superotemporal quadrant because of the ease of the insertion, however, the inferonasal BGI surgeries might be considered a good option depending on the condition of the conjunctiva.

