Short-term efficacy of unibody single-branched stent in the treatment of lesions involving the left subclavian artery: two-year follow-up outcomes
Bai-Lang CHEN, Xian-Mian ZHUANG, Min-Xin WEI,#
1Department of Cardiovascular Surgery, the Seventh Affiliated Hospital, Sun Yat-sen University, Shenzhen, China
2Department of Cardiovascular Surgery, Fuwai Hospital, Chinese Academy of Medical Sciences, Shenzhen, China
Keywords: Aortic dissection; Left subclavian artery; Single-branched stent graft; Thoracic endovascular aortic repair
The development of thoracic endovascular aortic repair (TEVAR) technology avoids the risk of patients opening the chest and is widely used in Stanford B-type dissection.[1–3]However, because TEVAR technology has clear requirements for vascular anatomy of the lesion, it limits its application to some patients. In the shortcomings of the proximal anchor zone, coverage of the left subclavian artery (LSA) origin without revascularization during TEVAR appears to have increased risk of stroke, upper extremity ischemia and paraplegia.[4]
Currently, there are mainly three endovascular techniques for LSA revascularization in TEVAR. Including chimney technique, fenestrated and branched stent grafts are used to overcome these difficulties.[5,6]For chimney techniques, the incidence of intraoperative endoleak and the risk of cerebral infarction are still being assessed.[7]For fenestrated technique, it is more difficult and risky to align the window and branch opening because of the natural bending structure of the aortic arch.[8]According to recent report, accidental or intentional coverage of arch branches during surgery is not uncommon.[9]So, there is a risk of endoleak or progression of the lesions due to the failure to fully cover the lesions. Therefore, the operation effect of fenestration technology and chimney technology is sometimes not satisfactory. The integrated branch stent has no gap between the branch and the main part, and because of the anchoring effect of the branch part, the risk of stent displacement and endoleak is reduced.
In this study, we reported the feasibility and early results of utilizing this novel single-branched stent graft in the treatment of type B aortic dissections (TBADs) with primary entry tear adjacent to the LSA.
From June 2017 to September 2019, twelve patients with TBADs were treated by endovascular repair with the castor single-branched stent grafts. Table 1 reports the characteristics of these twelve patients. There were ten men and two women with a mean age of 55 ± 14.9 years (range: 35–83 years). All patients had sudden onset of severe chest or back pain lasting from one to three days before hospitalization. All the cases were diagnosed by high-resolution computed tomography (CT) scans (section thickness: 1 mm). 3D reconstruction of the aorta and branch vessels showed that in all cases the primary tears were within 15 mm from the origin of the LSA (Figure 1). All patients underwent TEVAR using castor single-branched stent grafts (Figure 2). They were included if they underwent device implantation.
Before surgery, we select the appropriate stent by measuring the parameters related to the patient’s aortic arch. The diameter of LSA orifice, the distance between LSA and left common carotid artery (LCCA), the aortic diameters of the proximal and distal landing zones were measured by an experienced surgeon using preoperative computed tomography angiography (CTA). Based on these measurements, the single-branched stent graft was customized for each patient. The castor (Shanghai, MicroPort, China) branched aortic stent graft was a unibody branched graft consisting of a self- expandable stent and polyester vascular graft fabric. It consisted of a main stent graft and a side branch for the LSA. The side branch graft was 30 mm long with a diameter of 10–12 mm. The distance between neighboring side branch graft and proximal end of main graft was 5 mm, 10 mm, 15 mm or 20 mm. When the distance between LSA and LCCA is < 10 mm, the former (5 mm) is chosen; if the distance exceeds 10 mm, the latter (10 mm, 15 mm, 20 mm) is selected. All stent grafts were oversized 10%–15% with respect to the proximal aortic diameter. There is no bare stent at the proximal or distal ends of the stent graft. The operation was performed in digital subtraction angiography operation room and general or basic local anesthesia was given according the patient’s condition.
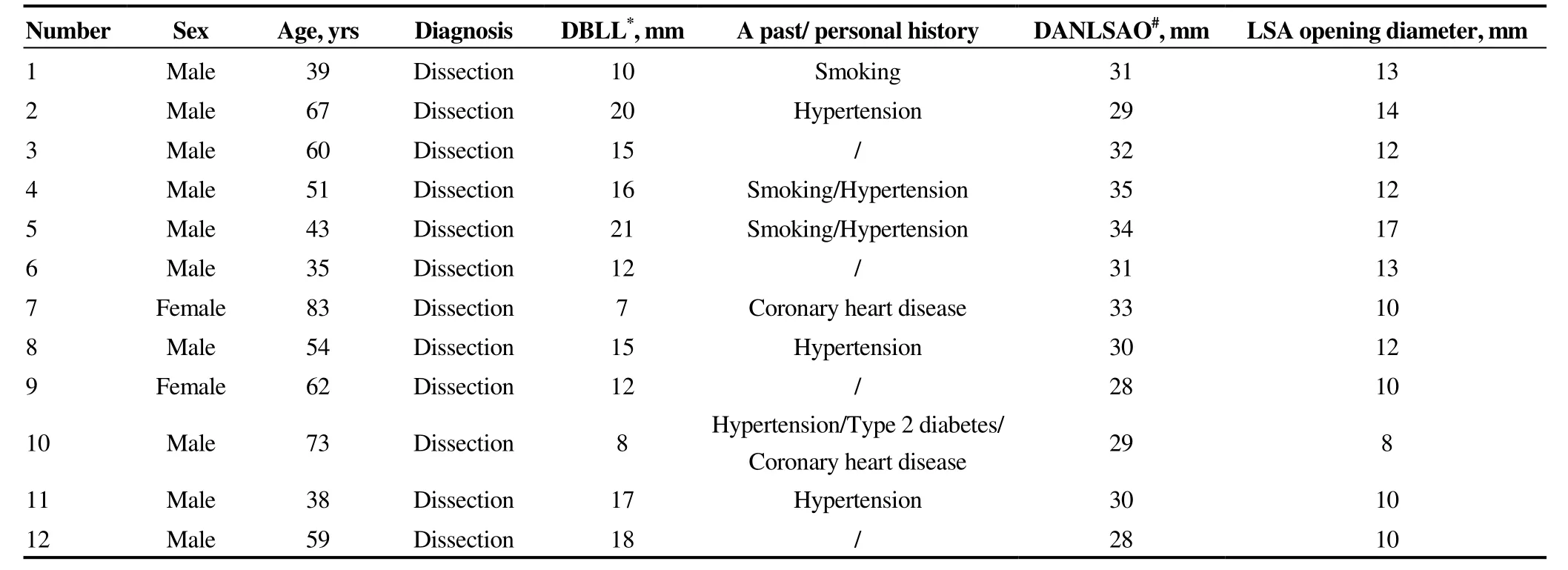
Table 1. Clinical data of twelve patients treated with TEVAR.

Figure 1. Preoperative radiography. Preoperative radiography suggests dissection rupture is involved LSA. LSA: left subclavian artery.
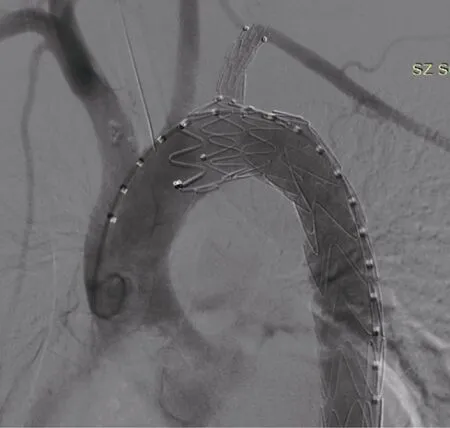
Figure 2. Postoperative radiography. After the release of the stent, it was suggested that the three branches were unobstructed and the rapture was closed well, and no endoleak was found.
After operation, patients were monitored for procedure related complications. A period of follow-up was two years. Follow-up included whether the patient died, the cause of death, complications, current symptoms, blood pressure in both upper limbs. CT scans were conducted at six months, twelve months and annually thereafter. The side branch patency, false lumen thrombosis, endoleak events and patient survival were recorded.
Immediate postoperative aortogram demonstrated successful exclusion of the lesion and good perfusion of LSA in all cases. All patients successfully completed the implanta- tion of the branch stent, and the lesion was completed closed. The intraoperative radiography showed that the stent was unobstructed and no endoleak occurred. Perioperative mortality was 0, and there were no serious complications such as stroke, acute myocardial infarction, renal failure or left arm ischemia. The seventh patient was placed with LCCA branch stent during operation. Because the lesion area is adjacent to the LSA, and the lesion is large. Single-branched stent was used to block LSA opening. Intraoperative angiography showed retrograde blood flow to the left vertebral artery. All the patients were followed up regularly after operation. There was no death, no special discomfort, and no complication of cerebral ischemia and left upper limb ischemia during the follow-up period. Hypertensive patients take the medicine on time, blood pressure is well controlled, and the blood pressure of the upper limbs is not much different. No re-operation was performed and no stent displacement was found. One month after the operation, however, a small type I endoleak was noticed in the third patient at the starting part of the stent. Endoleak was less, so untreated. This patient was no symptomatic after the operation, so did not undergo any further intervention. Late follow-up found that endoleak disappeared. There were no adverse clinical events in the outpatient follow-up of twelve patients. Aortic CTA showed that the stent was in place, the aorta and LSA stent were unobstructed, the rupture was completely occluded, there was no thromboembolism occurred in the false lumen of dissection.
Our experience shows that unibody single-branched stent graft design was a very promising proposal. Theoretically, the unibody design could natively avoid the gutter endoleak appeared in chimney technique and avoid loss of alignment due to the anchoring effect of the branch section, which made a contribution to stabilize the entire device. This stent can not only reconstruct some branches of aortic arch, but also ensure the blood flow of LSA, and there is no need for vascular bypass surgery. Moreover, compared with thoracotomy, integrated stent has made great progress in reducing surgical trauma, reducing operation time and so on. The main disadvantage is that the branch graft distortion may occur, and the branch stent need to be customized temporarily before operation and is not suitable for emergency patients.
All patients in this study had lesions involving LSA. Considering the risk of internal endoleak in fenestration technology, for such patients, the use of integrated single- branched aortic covered stent can avoid the injury caused by thoracotomy. At present, there is little research on the treatment of arch of disease with integrated stent. Huang, et al.[10]studied twenty-one cases of Stanford B dissection treated with single-branched stent. The successful rate of operation was 100% and perioperative mortality was 0. Intraoperative endoleak occurred in one case, blocking endoleak with stent again. During the follow-up period (one year), there were no complications such as paraplegia, cerebral infarction, left upper limb ischemia, dissection rupture and so on. Reexamination of CTA showed that the stent was unobstructed on displacement and endoleak occurred. In this study, all patients underwent successful surgery and stents were successfully release. No stent displacement and endoleak were found in intraoperative angiography. After follow-up, it was found that the thrombus of dissection was good and the branches of blood vessels were unobstructed.
At present, the standard length of the front end of the stent branch is 5 mm, 10 mm, 15 mm or 20 mm. In theory, the greater the distance between the LSA and the LCCA, the longer the length of the front end stent can have a longer anchoring zone, thereby reducing the leakage and displacement of the stent. The distance between LSA and LCCA in this study is more than 5 mm. Whether there is a risk of endoleak caused by insufficient anchoring area in patients than 5 mm remains to be observed in the future. When the short-distance stent is withdrawn from the LSA sheath, if the resistance is too large, there is a risk of pulling the front end of the body into the LSA opening. This situation did not occur in this study. At present, for patients with LSA and LCCA distance greater than 5 mm, this technique works well. For patients with shorter distances, the effect needs to be further clarified in the future.
Our limited experience showed that the castor branched aortic stent graft system was safe and feasible to obtain an adequate proximal landing zone while maintaining sufficient LSA perfusion during two-year follow-up. This product provided an attractive alternative to the endovascular treatment of TBADs. However, more experience and studies with longer follow-up are required before this product can be recommended for widespread use.
Acknowledgments
All authors had no conflicts of interest to disclose. The study was approved by the Seventh Affiliated Hospital, Sun Yat-sen University Institutional Review Board following the principles outlined in the Declaration of Helsink.
 Journal of Geriatric Cardiology2020年2期
Journal of Geriatric Cardiology2020年2期
- Journal of Geriatric Cardiology的其它文章
- Diagnostic chest X-ray in atrial septal defects
- Is it better to choose immediate dialysis treatment for renal transplant patients after PCI?
- A novel treatment of refractory coronary embolism: thrombus aspiration catheter-assisted twisting wire technique
- MicroRNA-29a attenuates angiotensin-II induced-left ventricular remodeling by inhibiting collagen, TGF-β and SMAD2/3 expression
- Beneficial effects of moderate to vigorous physical activity on cardiovascular disease among Chinese adults
- Atrial fibrillation among Russian men and women aged 55 years and older: prevalence, mortality, and associations with biomarkers in a population-based study
