Atrial fibrillation among Russian men and women aged 55 years and older: prevalence, mortality, and associations with biomarkers in a population-based study
Maria A. Shkolnikova, Dmitri A. Jdanov, Rukizhat A. Ildarova, Natalia V. Shcherbakova,#, Ekaterina B. Polyakova, Evgeny N. Mikhaylov, Svetlana A. Shalnova, Vladimir M. Shkolnikov
1Veltischev Research and Clinical Institute for Pediatrics of the Pirogov Russian National Research Medical University, Moscow, Russian Federation
2Laboratory of Demographic Data, Max Planck Institute for Demographic Research, Rostock, Germany
3International Laboratory for Population and Health, Research University Higher School of Economics, Moscow, Russian Federation
4Arrhythmia Department and Neuromodulation Laboratory, Almazov National Medical Research Centre, Saint-Petersburg, Russian Federation
5National Research Center for Preventive Medicine, Moscow, Russian Federation
Abstract Objective To examine the prevalence of atrial fibrillation (AF), its impacts on cardiovascular disease (CVD) and all-cause mortality, and the associations between AF and inflammatory and serum biomarkers in a population-based sample of Muscovites. Methods The study is a secondary analysis of data from the Stress, Aging and Health in Russia (SAHR) survey that includes information on 1800 individuals with an average age of 68.5 years at baseline, and on their subsequent mortality during 7.4 years on average. AF is detected by 12-lead electrocardiogram (ECG) and 24-hour Holter monitoring. The statistical analysis includes proportional hazard and logistic regression models. Results Of the 1732 participants with relevant Holter data, AF was detected in 100 (74 by ECG and Holter, 26 by Holter only). The prevalence of AF was 5.8% for men and 7.4% for women. The fully adjusted model showed strongly elevated hazard of CVD and all-cause mortality in men and women with long non-self-limiting AF (LAF). LAF was found to be negatively associated with elevated total and low- density lipoprotein cholesterol and to be positively associated with elevated markers of inflammation in women. Conclusions The study assessed for the first time the prevalence and the risks of death related to AF among older Russians. LAF was shown to be a strong and independent predictor of CVD and all-cause mortality. AF is unlikely to contribute to the large excess male mortality in Russia. The finding that one-quarter of AF cases were detected only by Holter monitoring demonstrates the usefulness of diagnostics with prolonged ECG registration.
J Geriatr Cardiol 2020; 17: 74-84. doi:10.11909/j.issn.1671-5411.2020.02.002
Keywords: Aging; Atrial fibrillation; Gender differences; Holter monitoring; Mortality; Prevalence
1 Introduction
Atrial fibrillation (AF) is the most common arrhythmia in aging populations, and given that its presence is associated with increased morbidity and mortality from cardiovascular diseases (CVD) and all causes, AF poses a growing public health challenge.[1-3]AF prevalence increases steeply with age, from less than 1% in individuals under age 50 to over 10% in people aged 80 and older.[3-6]In the European Union, the absolute number of adults aged 55 and older with AF has been estimated at 8.8 million in 2010 and is projected to rise to 17.9 million by 2060.[7]
The vast majority of papers on AF epidemiology have examined cohorts living in high-income countries, while only a few papers have investigated the epidemiology of AF in Eastern Europe.[8,9]In the context of Russia, only one previous study has assessed the prevalence, correlates, and mortality effects of AF in the general population.[10]This study drew on data from cohorts surveyed in the late 1970s and the early 1980s, with a study sample consisting of individuals with an average age of 47 at the baseline, including a few individuals over age 60. However, given the large burden of CVD and all-cause mortality in Russia, population-based studies on AF at old ages in the country are highly relevant.[11,12]Moreover, in light of the unusually large mortality gap between men and women in the general population of Russia,[13]it is important to investigate the relationship between AF and death separately for men and women.
In most population-based studies, AF is registered using electrocardiogram (ECG). However, 24-hour ECG monitoring (Holter monitoring) is a more comprehensive method for diagnosing AF, as it captures short episodes of AF[14]that have the potential to develop into permanent AF over the life course.[15]
Several biomarkers have been previously identified as predictors of stroke and death in subjects with AF.[16,17]Analyses of the association between AF and serum biomarkers have shed additional light on the development, perpetuation, and adverse outcomes of AF.[18]In several studies, AF has also been linked to inf lammatory biomarkers.[18-22]Finally, it has been suggested that there are sex differences in the associations between AF and inflammation and lipid profile markers.[23]This issue has yet to be explored for the Russian case.
This study is a secondary analysis of data from the Stress, Aging and Health in Russia (SAHR) study, which includes information on the baseline characteristics of Moscow residents and on their subsequent mortality.[13,24-26]
The aims of this study are to examine the prevalence of AF and sex differences in the AF prevalence, the effects of AF on CVD and all-cause mortality among men and women, and the associations between AF and inflammatory and serum biomarkers in a population-based sample of older Muscovites. Given the high level of CVD mortality and the large mortality gap between men and women in Russia, we intend to investigate whether some part of these population phenomena can be explained by patterns of AF prevalence and mortality impacts that are characteristic of Russia.
2 Methods
2.1 Study cohort
SAHR is a population-based cross-sectional study involving 1800 Moscow residents aged 55 and older (839 men and 961 women). The study participants were randomly selected from seven previous epidemiological cohorts from the Lipid Research Clinics (LRC) and the multinational MONItoring of trends and determinants in CArdiovascular disease (MONICA) studies conducted between the 1970s and the 1990s. Since these cohorts were restricted to individuals who were residents of Moscow before the mid- 1980s, a small number of additional participants who had moved to Moscow after 1985 were identif ied from the Moscow Outpatient Clinics’ registry.[26]
The baseline SAHR survey was fielded between December 2006 and June 2009. The fieldwork and data processing were conducted jointly by the National Research Center for Preventive Medicine (NRCPM, Moscow, Russia), the Max Planck Institute for Demographic Research (Rostock, Germany), and the Duke University in Durham (USA). The study’s design, sampling and recruitment, in-person interviews, and biomedical measures have been described in detail elsewhere.[26]
The SAHR survey produced a wide range of reported social and demographic parameters and biomedical data, which have been previously described.[26]These data include information on anthropometry; handgrip strength; office and home blood pressure; markers based on routine blood tests; blood biochemistry, including the lipid profile; glucose metabolism; markers of inflammation; neuroendocrine markers based on urine samples; 12-lead ECG; and 24-hour ambulatory Holter ECG monitoring.
The 12-lead ECG at rest was performed with the patient in the supine position and was coded using the Minnesota Code (MC) by two trained physicians. The Holter ECG monitoring was performed using a three-channel digital device (Schiller MICROVIT MT-101/200, Schiller, Switzerland). The Holter recordings were examined by two trained cardiologists in semi-manual mode and were checked again by another cardiologist.[26]
Subjects with missing ECG or Holter data or with Holter recordings of less than 17 hours were excluded from the analysis. Analyzable data series were available for 1732 individuals (96.2% of the total sample). Table 1 presents the statistics describing the study data.
2.2 Atrial fibrillation detection and classification
Atrial fibrillation was determined by the presence of AF on 12-lead ECG (MC 8-3) or on Holter recordings. At the time each subject was included, there was no information on the type of AF the individual had based on the current clinical guidelines. Therefore, we used the following definitions: (a) short self-limiting AF episodes (SSLAF): i.e., spontaneously terminating episodes of AF registered during Holter monitoring; and (b) long non-self-limiting AF episodes (LAF): i.e., continuous AF registered on both resting ECG and Holter recordings without sinus rhythm episodes. In the absence of clinical histories, (a) and (b) are assumed to be corresponding to paroxysmal AF and non-paroxysmal (persistent) AF, respectively.
When analyzing the data, we used three dichotomous variables for the presence of AF and its two forms: LAF; SSLAF; and the total AF (TAF), either LAF or SSLAF.

Table 1. Socio-demographic and biomedical characteristics of the sample under study by sex.
2.3 Other variables
The other variables we studied included: (1) classic cardiovascular risk factors: smoking, obesity, hypertension, lipid profile [total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglycerides (TG)]; (2) markers of inflammation: high-sensitivity C-reactive protein (CRP) and interleukin-6 (IL-6); and (3) self-reported adverse health conditions: myocardial infarction (MI) and stroke.
To define high-risk levels of the biomarkers, we used established cut-off points whenever possible (Table 1). Due to the high prevalence of mild hypertension and overweight in the SAHR sample, we chose the higher of the available established cut-off points that determine whether an individual has grade II hypertension [blood pressure (BP) ≥ 160/100 mmHg] or obesity [body mass index (BMI) ≥ 30 kg/m2].
Following earlier SAHR studies, we used the sex-specific upper quintiles of the IL-6 distribution with the same cut-off values as those established in our previous publications.[26]
Major CVD events were identified by the respondents’ self-reported history of MI and stroke provided in the questionnaire.
2.4 Mortality follow-up
Our study linked atrial fibrillation to the subjects’ subsequent mortality with and without adjustment for other covariates. The mean length of the follow-up period was 7.4 years (SD = 2.2 years), with a minimum of 10 days and a maximum of 9.6 years. The total exposure time was 12833 person-years (5555 for males and 7278 years for females). During the follow-up period, 416 deaths occurred (271 men and 145 women). Of these deaths, 248 were CVD (166 men and 82 women).
2.5 Statistical analysis
In all Tables 1-4, the characteristics of the sample and the prevalence of AF were weighted with post-stratification weights to adjust for differences in education (within each sex) between the SAHR sample and the general population of Moscow (based on the 2002 census). The significance of the differences between averages and proportions was checked with a Chi-square test.
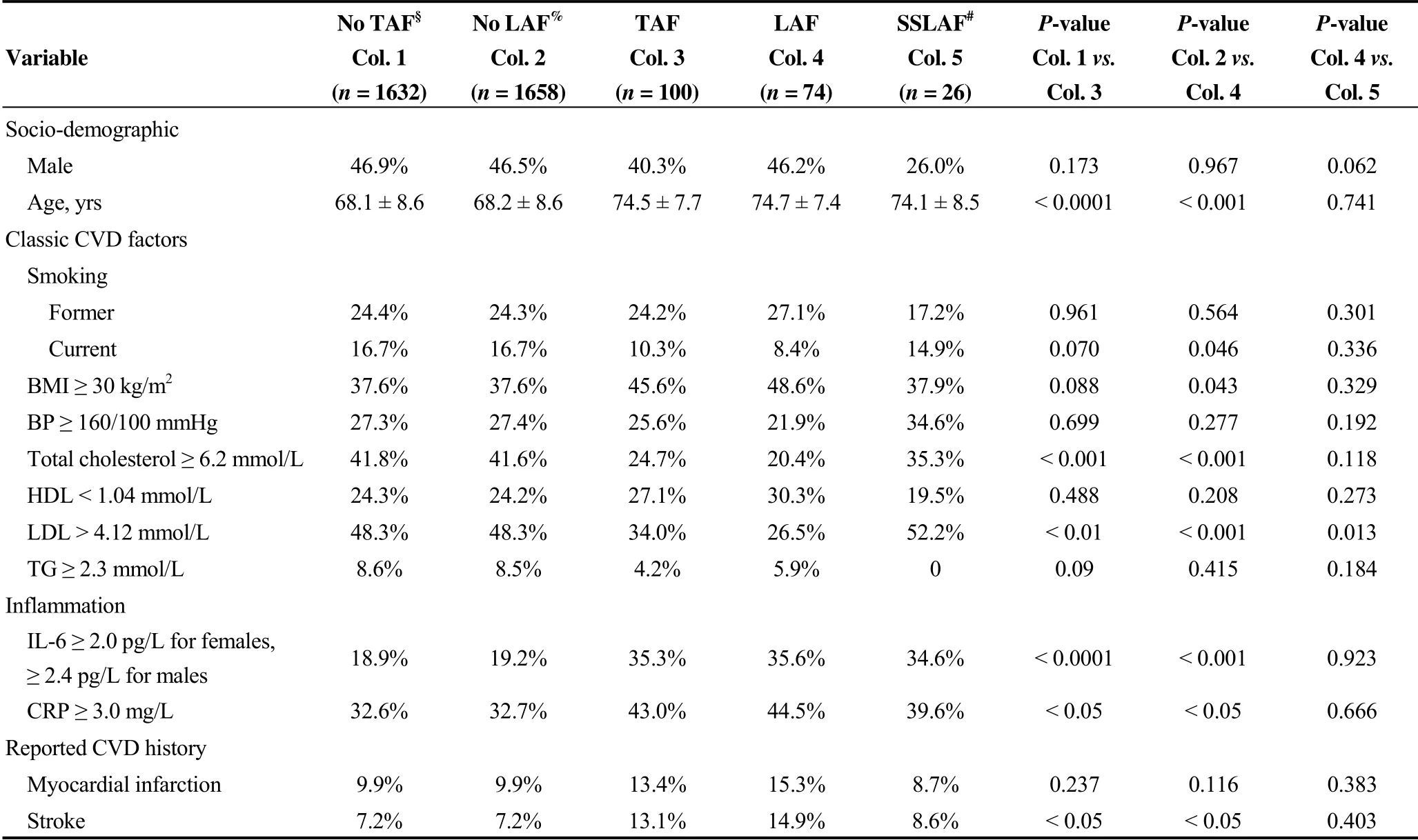
Table 2. Socio-demographic and biomedical characteristics depending on the atrial fibrillation status.
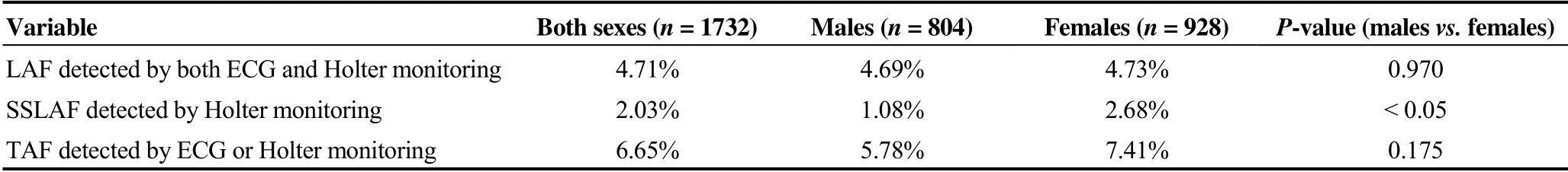
Table 3. Prevalence of atrial fibrillation.
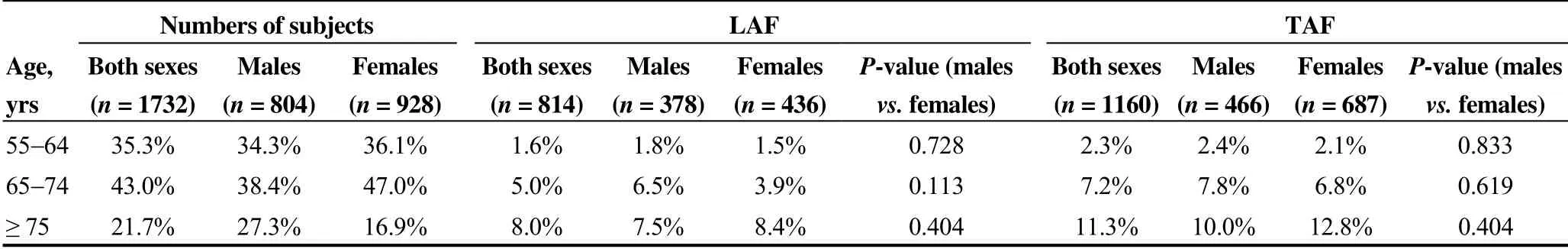
Table 4. Prevalence of the long non-self-limiting atrial fibrillation and of the total atrial fibrillation by sex and age group.
The relationships between the presence of LAF and of the total AF and age and sex were assessed by means of tabulations (Table 4) and logistic regression models (Table 5). These analyses were not carried out for SSLAF due to the scarcity of cases in sex- and age-specific cells.

Table 5. Odds ratios$ for the association of the long, non-self-limiting atrial fibrillation and of the total atrial fibrillation with age and sex.
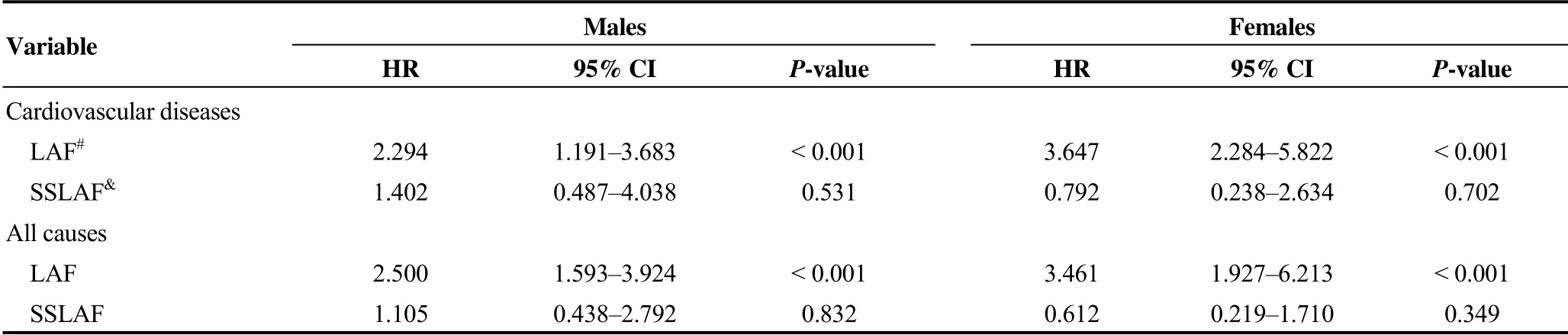
Table 6. Hazard ratios$ for the associations between mortality from cardiovascular diseases and mortality from all causes and two forms of atrial fibrillation.
Cox proportional hazard models were used to estimate changes in the death hazard in response to AF (Table 6). The respective associations were expressed by the hazard ratios (HRs). We used fully adjusted models with the classic CVD factors, markers of inflammation, and histories of MI and stroke under control. We ran proportional hazard regressions both for CVD and all-cause mortality. In the CVD mortality models, individuals who died from causes other than CVD were treated as censored as of the date of death.
After estimating each model, we visually checked that the double logged survival probability curves on the logged time corresponding to different values of the covariates were reasonably parallel. We then checked that the fitted survival curves were well approximated by the Cox model curves. Finally, we confirmed that the Schoenfeld residual test returned no evidence of a violation of the proportional hazard assumption for specific variables, or globally.
Logistic regression models were applied to assess the associations between the AF indicators (LAF and SSLAF) on the one hand and the markers of inflammation (AF and CRP) and of the lipid profile (total and LDL cholesterol) on the other hand (Table 7). All statistical analyses were carried out using Stata 15.0 (Stata Corp, College Station, TX, USA).
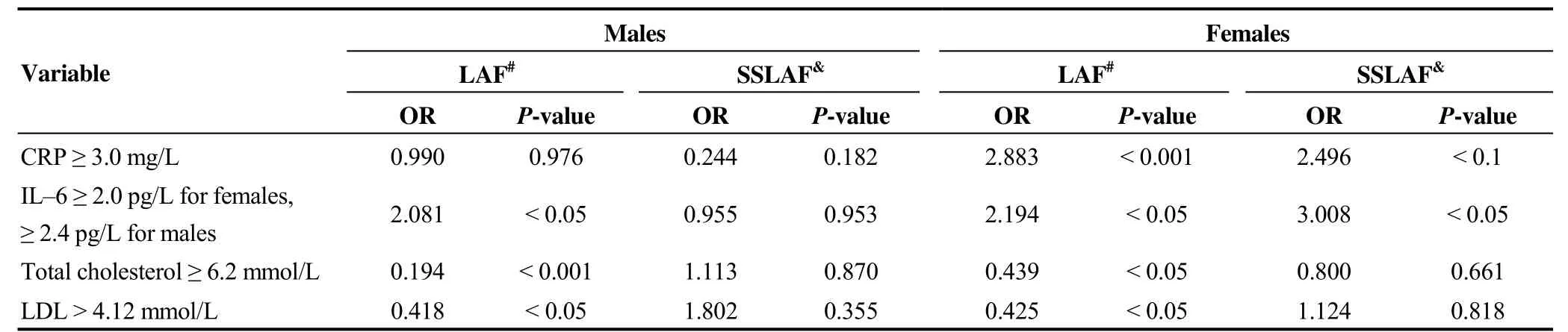
Table 7. Odds ratios$ for associations between two forms of atrial fibrillation and markers of inflammation, total and low-density lipoprotein cholesterol.
2.6 Ethical approval
We conducted a secondary analysis of SAHR data. The original SAHR study was approved by the ethics committee of the State Research Centre of Preventative Medicine (Moscow, Russia) and by the Institutional Review Board at Duke University (Durham, USA). All participants provided informed consent prior to data collection.
3 Results
The study comprised of 804 male and 928 female subjects (subject characteristics are presented in Table 1). For the sample broken down by sex, the table shows the percentages with high, middle, and low levels of education; the percentages in each of the smoking status categories, the percentages in the high-risk categories for the classic CVD risk factors and markers of inflammation; and the percentages who reported experiencing MI or stroke. Table 1 also shows that there were statistically significant differences between men and women in all of the variables except middle education, triglycerides, and markers of inflammation.
Of the 1732 participants, AF was detected in 100 subjects: LAF was found in 74 subjects (41 men, 33 women), and SSLAF was found in 26 subjects (10 men, 16 women).
Table 2 shows the demographic and biomedical characteristics of the subjects depending on their AF status. Compared to other participants, the subjects with any type of AF were older, had lower total and LDL cholesterol, and had higher levels of inflammation markers (both CRP and IL-6). Very little difference was found between subjects with LAF and those with SSLAF. Among those with SSLAF, the percentage of males was lower than the percentage of females (26% vs. 46%, P = 0.062) with a marginal statistical significance, and the prevalence of elevated LDL was significantly (P < 0.05) higher.
The prevalence of LAF was 4.7% for both men and women (Table 3). At the same time, the prevalence of SSLAF was significantly higher among women than among men (1.1% vs. 2.7%, P < 0.05). The prevalence of TAF was 5.8% among men and 7.4% among women (P = 0.175).
The prevalence of AF increased with age. Table 4 displays the prevalence values by age groups for men and women. The table shows that LAF rose from 1.8% (males) and 1.5% (females) at ages 55-64 to 7.5% (males) and 8.4% (females) at ages 75 and older. The prevalence of TAF increased from 2.4% and 2.1% to 10% and 12.8%, respectively. Point estimates of the prevalence of both LAF and TAF were higher among men than among women at ages 55-74 and were higher among women than among men at ages 75 and older. However, Table 4 indicates that none of the male-female differences in the prevalence levels were statistically significant.
The logistic regression models (Table 5) show that for both LAF and TAF, a 10-year increase in age corresponded to the same odds ratio (OR) of 1.08 (95% CI: 1.05-1.12).
The analysis of the associations between LAF and mortality from CVD, adjusted for age, education, classic CVD risk factors, markers of inflammation, MI, and stroke, uncovered a number of strong links (Table 6). For CVD mortality, the HR values were 3.65 (95% CI: 2.28-5.82) for women and 2.29 (95% CI: 1.19-3.68) for men, respectively. For all-cause mortality, the corresponding figures were 3.46 (95% CI: 1.93-6.21) and 2.50 (95% CI: 1.59-3.92). No association between SSLAF and either CVD or all-cause mortality was found.
AF was shown to be directly related to elevated markers of inflammation among women: both CRP and IL-6 were significantly associated with LAF (Table 7). The findings also indicated that there was a significant link between SSLAF and IL-6 and a marginally significant link between SSLAF and CRP. Among men, the only statistically significant association detected was between LAF and IL-6.
Elevated concentrations of total and LDL cholesterol were found to be negatively associated with LAF in both men and women. For SSLAF, no statistically significant association with blood lipids was found.
4 Discussion
4.1 Prevalence
The prevalence of AF observed in our population-based sample (6.7%) and its rate of increase with age were comparable to estimates reported by studies conducted in Western Europe.[27-31]In this region, the AF prevalence was found to be increasing from 2%-3% among individuals aged 55 to 64 to 10%-17% among individuals aged 80 and older.[5,27,31-34]Surprisingly, the AF prevalence figures in our Russian sample (exposed to high CVD mortality) were shown to be close to the lower limits of the range of earlier estimates: i.e., the percentages of ECG-detected cases were 1.6% at ages 55-64 and 8.0% at ages 75 and older.
In the literature, AF was found to be more common in males than in females, with a ratio of around 1.2:1.[5]The mechanisms underlying this difference are unknown and might include the anti-inflammatory effects of estrogens.[35]In our study, the point estimates of the prevalence of LAF were higher among men under age 75 and were higher among women aged 75 and older. However, these differences were statistically insignificant. This finding is in line with the results of the AF study based on the Russian LRC and MONICA data of the 1970s-1990s, which also reported almost no differences in the overall prevalence of the ECG- based AF between men and women in Moscow and St. Petersburg.[36]
Holter monitoring allowed us to additionally identify the 26% of AF cases that were not captured by ECG. These SSLAF cases appeared to be more prevalent in women than in men. This observation is broadly consistent with the findings of studies showing that the duration of AF episodes tends to be shorter in women than in men, which may lead to the under-diagnosis of silent paroxysmal AF in women.[37,38]
4.2 Mortality
We found that among older Muscovites, LAF was strongly associated with mortality from CVD after adjustment for classic CVD risk factors and major health conditions, as mortality was shown to be 3.5 times higher among men and 2.5 times higher among women with LAF. These relative risks are among the higher estimates reported in the literature.[39-42]
We also detected highly elevated relative risks for all- cause mortality among men and women with LAF. This observation is in line with results from earlier research.[2,23]
In our study, the HR for CVD death and death from all causes associated with LAF was higher among women than among men. This result is consistent with the findings of the Copenhagen City Heart Study, and of a study of elderly Japanese that reported substantially higher relative risks of cardiovascular death for women with AF compared to men with AF.[40,42]
Although a higher relative risk of death associated with AF among women has been widely reported across the world, the risk level varies depending on the region and the socio-economic context.[34]The Framingham Study reported only a moderate excess risk in women compared to men.[2]Another study found no difference in the relative risk between the sexes.[23]
The higher relative risk of death among women combined with the similar prevalence of LAF in men and women found in our study implies that the presence of AF alone cannot explain the much higher levels of mortality from CVD and all causes among Russian men than among Russian women.
The relationship between mortality and the form of AF has been previously studied, but the findings are inconsistent. Most of these studies indicated that the mortality risk is higher in patients with permanent AF than in patients with other forms of AF.[5,42-45]Our study found no association between SSLAF and the hazard of CVD or all-cause mortality.
Nevertheless, the early detection of paroxysmal AF is important. Indeed, in our study, SSLAF cases constituted about a quarter of all AF cases, which might still be an under-diagnosis, considering that the majority of subjects were previously unaware of the arrhythmia.
Earlier research has suggested that within a 4 to 5-year period, around one-third of patients with paroxysmal AF develop persistent/permanent AF, and 77% do so within 14 years.[46,47]In our study, SSLAF was detected in 26 subjects, and estimates suggest that in 8-15 of them AF could have become persistent during the follow-up period. With such a small number and such short time intervals between the onset of these hypothetical new cases of persistent AF and the end of the follow-up period, our chances of capturing the mortality effects of paroxysmal AF were low. It may be expected, however, that larger population-based studies with longer follow-up periods will be able to measure more accurately the consequences of paroxysmal AF, including its mortality impacts.
4.3 Inflammation and blood lipids
We found significant links between LAF and markers of inflammation and determined that these links were stronger in women than in men. Both CRP and IL-6 were shown to be associated with LAF in women, but only IL-6 was found to be associated with LAF in men. The association between permanent AF and inflammation markers was examined in earlier studies.[18-22]In particular, the Framingham Study and the Gutenberg Health Study found an association between CRP and AF for both sexes.[18,48]In the Cardiovascular Health Study, CRP was not only proven to be associated with the presence of AF; it was linked to an elevated risk of developing AF in the future.[19]Some studies have also examined a potential relationship between IL-6 and AF. The Chronic Renal Insufficiency Cohort Study and the Heart and Soul Study found an association between the plasma IL-6 and AF.[49,50]
The evidence we found of associations between CRP and IL-6 and both forms of AF in women, but not in men, contradicts the results of the study by Magnussen, et al.[23]which reported no sex differences in links between CRP and AF; and the findings of the study by Nyrnes, et al.[21]which showed that CRP was associated with AF in men only.
An earlier study on the same sample of Muscovites showed that elevated markers of inflammation explain a substantial share of the mortality differences by level of education.[51]The link between AF and inflammation found in the present study suggests that AF may be involved in the biological pathways that underlie the excess mortality in lower socio-economic strata.
We should point out that the general understanding of the biological mechanisms behind the association between inflammation and AF is still insufficient. In particular, it is still unclear whether inflammation is an initiator, a consequence, or a parallel/linked process with respect to AF.[21]
Our study showed strong negative associations between LAF and total and LDL cholesterol levels in both men and women. The possibility that the well-known risk factors of atherosclerosis and CVD are simultaneously protecting against AF has also been raised in several earlier studies.[21,23,52-56]
The anti-inflammatory effect of cholesterol is a potential explanation for the reduction of the risk of AF in situations in which the concentrations of total and LDL cholesterol are high.[57,58]Lipids constitute a part of the cell membrane and thus affect the electrophysiological properties of the cell. It has been shown that in vitro, cholesterol can change the functional activity of ion channels, which are involved in the pathogenesis of atrial fibrillation.[59,60]It is, therefore, possible that low levels of cholesterol can facilitate inflammatory processes that play a significant role in the pathogenesis of AF.
We found no correlation between SSLAF and blood lipids in men or in women.
4.4 Strengths and limitations
This is the first population-based study that provides up-to-date information on the prevalence of AF and its association with CVD and all-cause mortality among older- age Russians. AF was identified using both ECG and 24- hour Holter monitoring, which also allowed for the detection of paroxysmal AF.
This is also the first study that has assessed the associations between AF and markers of inflammation and cholesterol among elderly Russians.
This study has some limitations. Firstly, as our study of the presence of AF was cross-sectional, we were unable to monitor the development and incidence of AF over time using the initial values of the biomarkers and other characteristics at baseline. Thus, we had no chance to examine the causal links between the risk factors and the development of permanent AF. Secondly, because the clinical histories of AF in the subjects were not available, we were unable to diagnose with full confidence the persistent and paroxysmal forms of AF and had to use the LAF and SSLAF categories instead. This drawback was especially important for diagnosing paroxysmal AF. In particular, for cases in which AF was not detected on either the ECG or the Holter recording, it was not possible to be absolutely sure that episodic AF was completely absent. Last but not least, the number of subjects with SSLAF identified by Holter monitoring was small and lacked statistical power in the analyses. Statistical power was also a problem for some of the analyses involving LAF. In particular, we were unable to obtain conclusive results on the sex-age interaction for the odds of LAF.
In spite of these limitations, the study produced a range of novel and meaningful results.
4.5 Potential clinical and health-care implications
The study’s findings raise several important issues that have significant implications. Firstly, the large share of AF cases that were detected by Holter monitoring suggests that prolonged ECG registration technique should be implemented in population-based studies, and used more actively in clinical practice. Resting ECG, which has long been considered the gold standard for diagnosing AF in patients, may be insufficient in some cases and should, therefore, be reassessed. Long-term ECG recording may be the better technology to use when testing elderly patients at high risk of stroke. Secondly, the negative association we found between AF and serum LDL and total cholesterol should be investigated further. Specifically, researchers should attempt to determine whether serum LDL and cholesterol protect against AF, and, if so, how this evidence could be used for AF prevention. Last but not least, the risks associated with paroxysmal AF detectable by Holter monitoring should be further evaluated in studies with larger sample sizes and longer follow-up periods.
5 Conclusions
In this population-based study, we assessed for the first time the prevalence of AF among elderly residents of Moscow. The results showed that the prevalence for all forms of AF was 6.7% for both sexes and that the prevalence of long AF episodes (mainly persistent arrhythmia type) was somewhat lower than the levels detected in a majority of comparator studies.
LAF was shown to be strongly and independently associated with CVD and all-cause mortality: i.e., mortality was found to be 3.5 times higher among men and 2.5 times higher among women with LAF. These estimates are consistent with some of the highest relative risks reported in the literature.
We also found that markers of inflammation were associated with AF and that these associations were stronger for women than for men. Serum LDL and total cholesterol levels were shown to be inversely associated with AF. These findings suggest that serum LDL and total cholesterol might play a protective role, although whether this is actually the case requires further investigation.
Acknowledgements
This work was supported by the U.S. National Institutes of Health (NIH) grant P01AG031719. D.A.J. and V.M.S. were partly supported by the Russian program of the state support of leading universities of the Russian Federation “5-100”. E.N.M. was supported by the Russian Federation President Grant Council’s grant #MD-2314.2020.7. We used data from SAHR, an earlier study that had been supported by the NIH grant R01AG026786. The funders had no role in the study design; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the manuscript.
We are grateful to Evgeny Andreev at the Higher School of Economics in Moscow and to Alexander Deev at the National Research Center for Preventive Medicine in Moscow for their rigorous work on cleaning and processing of the SAHR data.
 Journal of Geriatric Cardiology2020年2期
Journal of Geriatric Cardiology2020年2期
- Journal of Geriatric Cardiology的其它文章
- Diagnostic chest X-ray in atrial septal defects
- Short-term efficacy of unibody single-branched stent in the treatment of lesions involving the left subclavian artery: two-year follow-up outcomes
- Is it better to choose immediate dialysis treatment for renal transplant patients after PCI?
- A novel treatment of refractory coronary embolism: thrombus aspiration catheter-assisted twisting wire technique
- MicroRNA-29a attenuates angiotensin-II induced-left ventricular remodeling by inhibiting collagen, TGF-β and SMAD2/3 expression
- Beneficial effects of moderate to vigorous physical activity on cardiovascular disease among Chinese adults
