Economic evaluation of cervical cancer screening strategies in urban China
Li Ma,Yuying Wang,Xiaohong Gao,Yi Dai,Yu Zhang,Zhaojing Wang,Xiaoxia Wang,Limin Wang,Jing Jiang,Xinhua Jing,Chunxia Yang,Fanghui Zhao,Jinghe Lang,Youlin Qiao,
1Department of Epidemiology,School of Public Health,Dalian Medical University,Dalian 116044,China;2Department of Obstetrics and Gynecology,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences/Peking Union Medical College,Beijing 100730,China;3Department of Obstetrics and Gynecology,Wafangdian Maternal and Child Health Care Hospital,Dalian 116300,China;4Department of Epidemiology and Biostatistics,West China School of Public Health,Sichuan University,Chengdu 610041,China;5Department of Epidemiology,National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China
Abstract Objective:This study evaluated the feasibility of different cervical cancer screening strategies in urban China.Methods:A Markov model was constructed to simulate a hypothetical cohort of 100,000 females aged 30-59 years in a 20-year period.Screening strategies included liquid-based cytology (LBC) every three years,human papillomavirus (HPV) DNA testing every three and five years,respectively,and a combination of HPV DNA testing and LBC (HPV+LBC) every three and five years,respectively.Model outcomes included cumulative incidence over 20 years,cumulative risk of cervical cancer,costs,life year saved (LYS),quality-adjusted life years(QALYs) and benefits.The cost-effectiveness ratios (CERs),incremental cost-effectiveness ratios (ICERs),costutility ratios (CURs),and benefit-cost ratios (BCRs) were used as outcomes in the health economic evaluation analysis.Univariate sensitivity analyses were performed to examine the stability of the results.Results:The cumulative incidence of the five screening strategies ranged from 833.02 to 1,158.07 cases per 100,000 females.HPV DNA testing was most effective in reducing the cumulative risk of cervical cancer,saving life years and QALYs and gaining benefits.The CERs of HPV DNA testing every three and five years,and LBC every three years were considered to be very cost-effective if they were below China’s GDP per capita.The CERs of HPV+LBC were considered to be cost-effective if they were below three times GDP per capita.The incremental cost-effectiveness analysis showed that HPV DNA testing every three and five years,LBC every three years and HPV+LBC every five years were dominant strategies.Conclusions:The findings of this study indicated that HPV DNA testing every five years or LBC every three years should be recommended in urban China.
Keywords:Cervical cancer;Markov model;economic evaluation
Introduction
Cervical cancer is one of the most common cancers among females worldwide.It can be directly observed,sampled and detected early.With an estimated 570,000 cases and 311,000 deaths in 2018 worldwide,cervical cancer ranks as the fourth most frequently diagnosed cancer and the fourth leading cause of cancer-related deaths in females (1).In the past few decades,the incidence and mortality of cervical cancer have declined worldwide due to early screening,early diagnosis,early treatment and vaccination.However,the occurrence of cervical cancer has not been effectively controlled.China has one of the heaviest burdens of cervical cancer disease worldwide.The burden of cervical cancer in China varies greatly in the different regions of the country due to the differences in the population size,geographical location,economic conditions,and other factors (2).According to a study of the National Central Cancer Registry of China,the incidence of cervical cancer was 15.62/100,000 in urban areas and was 14.65/100,000 in rural areas,the mortality rate of cervical cancer was 3.85/100,000 in urban areas and was 4.14/100,000 in rural areas (3).Another study showed that crude incidence rates(CIRs) and age-standardized incidence rates (ASIRs) for cervical cancer in urban and rural China generally showed sharp increasing trends during the period 2000-2014 in China (4).
In urban China,cervical cancer screening methods mainly include liquid-based cytology (LBC) and human papillomavirus (HPV) DNA testing.The application of LBC in clinical practice can significantly improve the diagnostic level of related diseases,sensitivity and specificity of cervical lesion screening,and overcome the high false-negative rate in traditional diagnosis (5-7).Recent clinical studies have reported that HPV DNA testing has a higher sensitivity for detecting high-grade precancerous lesions (8-11),thereby potentially facilitating early detection and treatment.Both screening techniques have their advantages.Hence,choosing a suitable strategy for cervical cancer screening in urban China is very complex and involves multiple tradeoffs.
In this study,we constructed a Markov model to predict the impact of adopting five screening strategies,including LBC every three years,HPV DNA testing every three years,HPV DNA testing every five years,HPV+LBC every three years,and HPV+LBC every five years,for determining the optimal strategy for cervical cancer screening and informing policy recommendations in urban China.
Materials and methods
Analytical approach
We constructed a Markov model to simulate the natural development of cervical cancer in 100,000 females aged 30-59 years old using five different screening strategies over a 20-year period.The screening strategies that were compared included LBC every three years,HPV DNA testing every three and every five years,respectively,HPV+LBC every three and every five years,respectively.The screening process is shown inFigure 1.Model outcomes included cumulative incidence over 20 years,cumulative risk of cervical cancer,costs,life year saved(LYS),quality-adjusted life years (QALYs) and benefits.The cost-effectiveness ratios (CERs),incremental costeffectiveness ratios (ICERs),cost-utility ratios (CURs),and benefit-cost ratios (BCRs) were used as outcomes in the health economic evaluation analysis.ICER,calculated as the additional cost (RMB) for each additional LYS of a strategy compared with the next most costly strategy,was used as a performance indicator.Strategies that were most costly and less effective or less costly and less cost-effective were excluded from the incremental cost-effectiveness calculations.The“most cost-effective”strategy is not necessarily the one that has the lowest ratio as the society may be willing to pay more for health benefit.Since China does not have a clear survey on willingness to pay,we used gross domestic product (GDP) per capita instead as a measure of whether an intervention is“good value for money”.We adapted a societal perspective,and all costs and outcomes were discounted by 3% (12) annually.Univariate sensitivity analysis was performed to assess the stability of the model’s assumptions on the study findings.Additionally,we performed probabilistic sensitivity analyses(PSA) to assess parameter uncertainty by varying key model parameters and conducted 5000 Monte Carlo simulations with sampling from the distributions of these parameters.A 50% increase or decrease in the base-case value for the costs of screening and treatment were changed during analysis.Beta distributions were applied for the transition probability and the sensitivity and specificity of screening tests.The results of these simulations were presented as cost-effectiveness acceptability curves (CEACs).
Screening tests
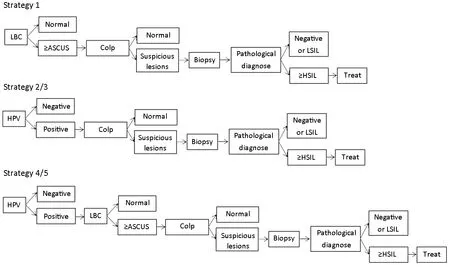
Figure 1 Process of five screening strategies.Strategy 1:LBC every 3 years.Strategy 2/3:HPV DNA testing every 3 years or every 5 years.Strategy 4/5:HPV DNA testing combined with LBC every 3 years or every 5 years.LBC,liquid-based cytology;HPV,human papillomavirus;ASCUS,atypical squamous cells of uncertain significance;Colp,colposcopy;LSIL,low-grade squamous intraepithelial lesions;HSIL,high-grade squamous intraepithelial lesions.
HPV DNA testing was performed using fluorescence polymerase chain reaction (PCR),which can identify HPV16,HPV18 and other high-risk HPV types.HPV DNA testing has high sensitivity and negative predictive value.LBC is a smear screening method that uses liquidbased thin-layer cytology (TLC) detection system to detect cervical cells for cytological classification diagnosis.Compared with conventional Pap smear,LBC improved the sample collection rate and evenly distributed the cells on the slides by controlling the cell overlapping density,which not only was conducive to the film reading and evaluation but also improved the sensitivity of detecting cervical lesions of high and low degrees.
Construction of Markov model

Figure 2 Natural history of cervical cancer.HPV,human papillomavirus;CIN,cervical intraepithelial neoplasia.
A Markov model based on the natural history of cervical cancer (Figure 2) was developed to simulate transitions between eight health states [healthy,HPV infection,cervical intraepithelial neoplasia (CIN) stages 1-3,cervical cancer,death due to cervical cancer and death due to other diseases]in the presence of screening.The initial probability of this study was derived from 17 populationbased cross-sectional surveys conducted by the Cancer Institute of the Chinese Academy of Medical Sciences(CICAMS) in five urban areas and nine rural areas between 1999 and 2008,covering nine provinces in China (13).These results can accurately reflect the distribution of different stages of cervical cancer in China,and have good representativeness.The transition probability used in this study was partly derived from the evaluation of cervical cancer screening methods in Shanxi Province (14),and the results showed good representativeness.Data of cancer transit to death was derived from high-quality international literature.Data of mortality due to other diseases were obtained from the Chinese Statistics Pocketbook in 2016.Other parameters were based on the review of literature(15).The health utility value was used to investigate and evaluate the quality of life of the enrolled females.After calculation,the weight values of CIN1,CIN2,CIN3 and cancer at each stage were 1.000,0.863,0.797 and 0.621,respectively.All analyses were conducted using Microsoft Excel 2003 (Microsoft,Redmond,WA,USA) and TreeAge Pro 2011 (TreeAge Software,Inc.,Williamtown,MA,USA).
Epidemiological data
The age of the 100,000 females ranged from 30 to 59 years,and the females were divided into six age groups at an interval of five years.The population distribution of each age group referred to the data of the sixth national population census,and was sorted to obtain the population composition ratio of each age group.Screening test characteristics (i.e.,sensitivity and specificity) were based on a combination of published studies (16,17) and expert opinion.Colposcopy referral rates were obtained from the results of a preliminary project of the CICAMS on the referral rate of cervical carcinoma with colposcopy,including Shanxi Province of Cervical Cancer Screening(SPOCCS) studies and the Screening Technologies to Advance Rapid Testing (START) (18-21).The screening coverage rate adopted in this study was 70%,which was the coverage rate of cervical cancer screening in China achieved by CICAMS database (22,23).
Cost data
Costs associated with screening and treatment were estimated using a micro-costing method.Screening costs included direct medical cost,direct non-medical cost and indirect cost.Direct medical costs were estimated to account for consumables,equipment and human costs.We selected 11 urban cities and 3,000 people from each city to investigate the consumables,equipment and human costs associated with the screening process.In addition,we also considered accommodation,nutrition and transportation costs (direct non-medical costs).Indirect cost associated with screening was mainly the productivity loss,which means the economic loss caused by the missed work.Indirect costs also included resource inputs (e.g.,planning,training,mobilization,management,etc) .
Treatment costs refer to the costs for the treatment of CIN2 and above in accordance with the principles of clinical diagnosis and treatment,including direct medical cost and indirect medical cost.We collected data on different clinical stages of cervical cancer from January 1,2015,to December 31,2015,including treatment costs for CIN2,CIN3,early stage (IA/IB/IIA) and advanced stage(IIB/IIIA/IIIB/IVA/IVB).Given that some CIN2 and CIN3 patients can be treated in the outpatient department,CIN2 and CIN3 survey subjects included outpatient and inpatient departments,respectively.Indirect medical costs include nutrition costs,round-trip fares,lost wages,etc.This study summarized and sorted the primary data collected from various urban areas involved in the screening.We referred to numerous relevant studies to summarize the data and characteristics,and select representative values.We selected the mean of the normal distribution data and the median of the skewed distribution data as the model parameters.The cost parameters used in this Markov model are shown inTable 1.
Results
Costs and impacts of five screening strategies
In the group with no intervention,the total cost was 26.1993 million RMB,the cumulative incidence over 20 years was 1,496.67 cases per 100,000 females,the life years were 761,287.73 years,and the QALY were 755,475.80 years.The cumulative incidence over 20 years of the five screening strategies ranged from 833.02 to 1,158.07 cases per 100,000 females.Compared with no screening,all screening strategies reduced the cumulative risk by 22.62%-44.34%,increased the cost from 28.57 to 51.42 million RMB,prolonged LYS from 444.61 to 868.78 years and QALYs from 1,526.83 to 3,333.70 years,and gained 122.17-241.74 million RMB.For all strategies,the relative cost-effectiveness order for lowering cervical cancer incidence,increasing LYS and QALYs,and gaining benefits were HPV DNA testing every three years (most effective),HPV DNA testing every five years,LBC every three years,HPV+LBC every three years and HPV+LBC every five years (the least effective).These results are shown inTable 2.
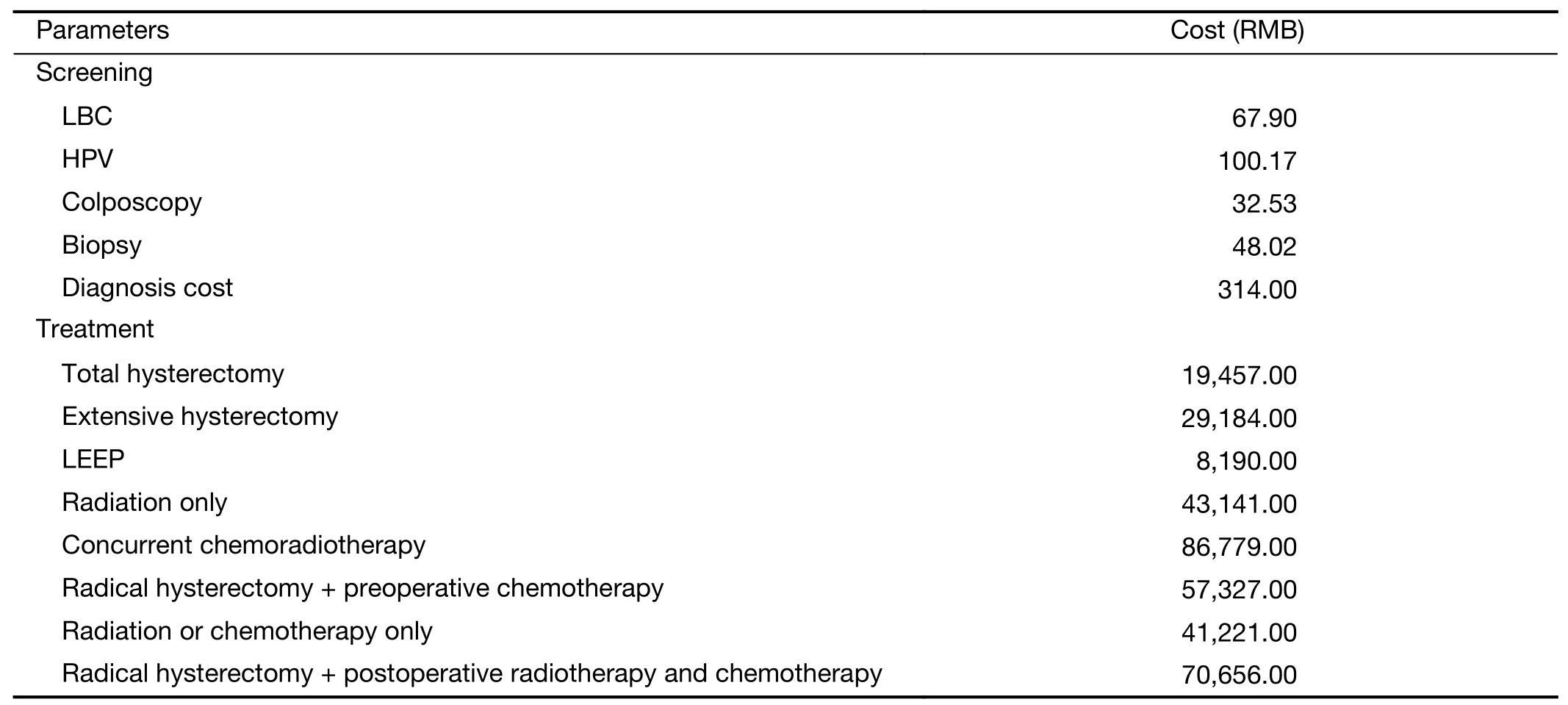
Table 1 Cost parameters used in the model
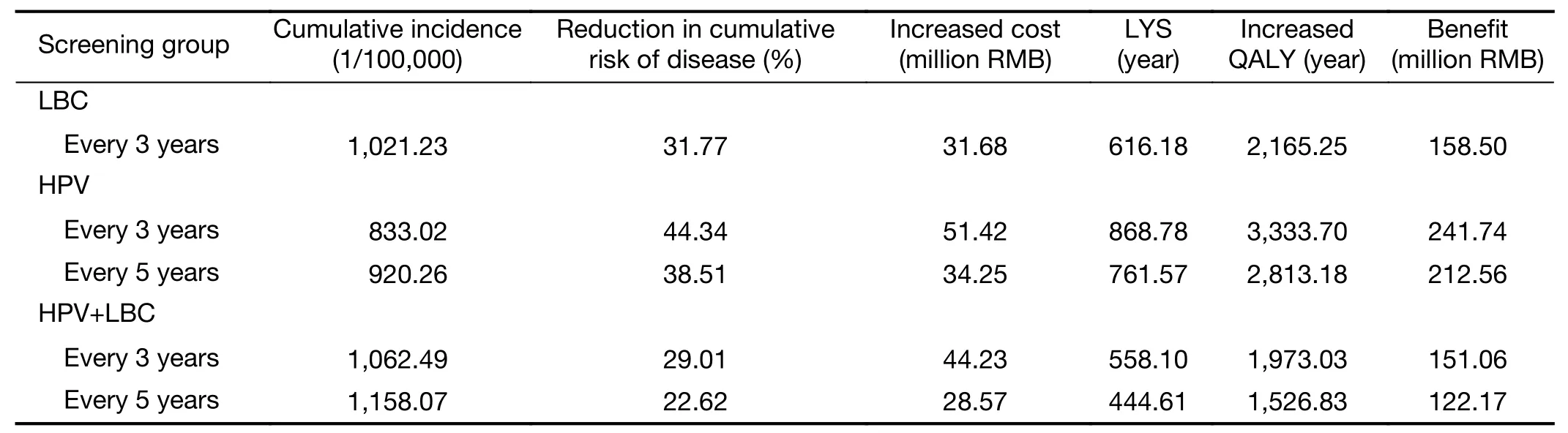
Table 2 Compared with the unscreened group,the increased cost,acquired effect,utility and benefit of the screening group
Economic evaluation outcomes
We calculated the CER,CUR and BCR for each strategy as compared to no intervention.The CERs of the five screening strategies ranged from 44,971.21 to 79,252.94 RMB per LYS,the CURs ranged from 12,174.41 to 22,417.89 RMB per QALY,and the BCRs ranged from 3.42 to 6.21.In accordance with the World Health Organization (WHO) recommendations for health economic assessment (24),the CERs of three screening strategies,including HPV DNA testing every three and five years,and LBC every three years,were below China’s GDP per capita,and could be considered very costeffective.The CERs of HPV+LBC were below three times GDP per capita,and could be considered cost-effective.These results are shown inTable 3.
However,in practice,the CER alone cannot fully explain the merits and demerits of each screening strategy.We used incremental cost-effectiveness analysis to further explain whether or not the screening algorithm is optimal.Figure 3depicts the efficiency frontiers showing the tradeoff between costs and benefits.In this study,HPV DNA testing every three years,HPV DNA testing every five years,LBC every three years and HPV+LBC every five years were dominant strategies.HPV+LBC every three years was excluded from the incremental cost-effectiveness calculation.For HPV DNA testing every three years as compared to HPV DNA testing every five years,the additional cost for each additional LYS was 160,206.14 RMB.For HPV DNA testing every five years as compared to LBC every three years,the additional cost for each additional LYS was 17,636.01 RMB.For LBC every three years as compared to HPV+LBC every five years,the additional cost for each additional LYS was 18,176.84 RMB.
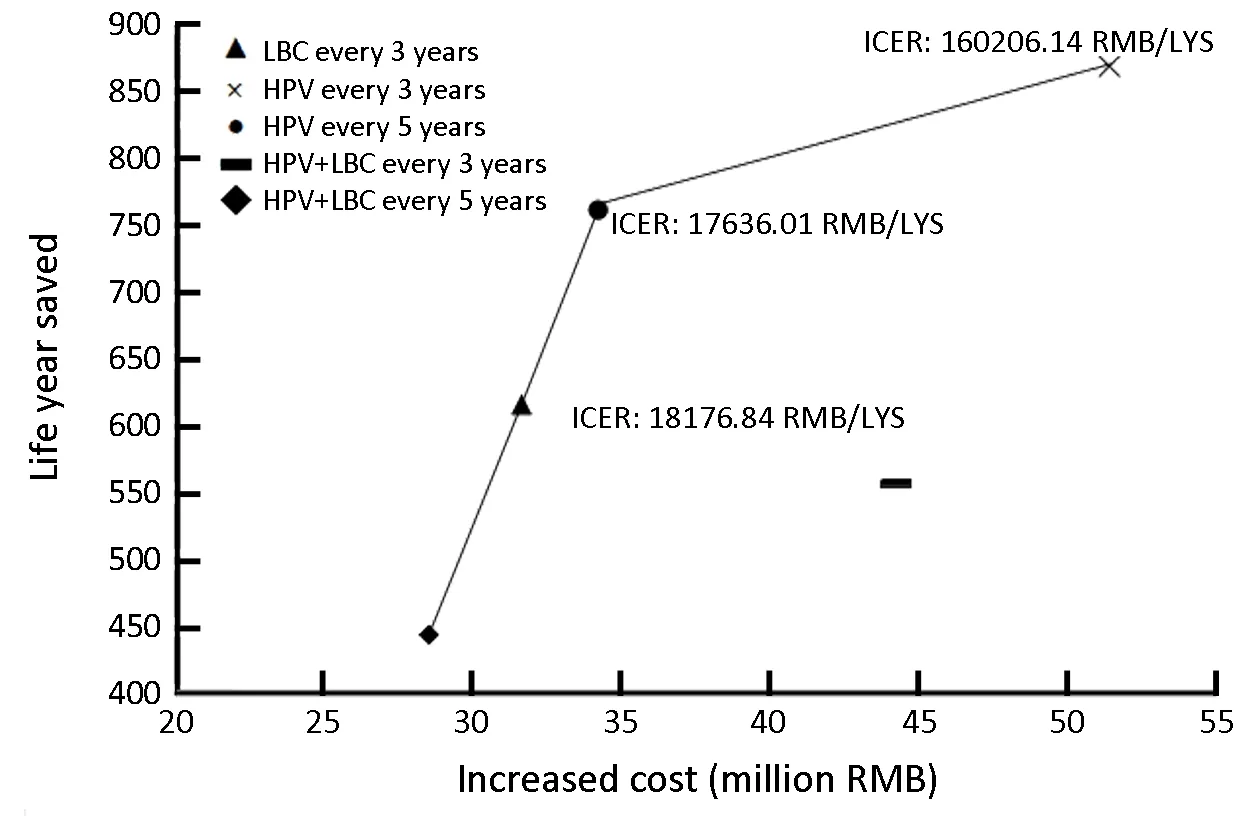
Figure 3 Efficiency frontiers showing trade-off of costs and benefits.Strategies lying on the efficiency curve are either less costly and more effective (i.e.,strongly dominant) or more costly but more cost-effective (i.e.,weakly dominant) than those lying to the right of the curve.The slope of the efficiency curve (also the inverse of the ICER) will be steeper when the net gain in the life expectancy per RMB is greater.LBC,liquid-based cytology;HPV,human papillomavirus;ICER,incremental cost-effectiveness ratios.

Table 3 Results of health economic evaluation
Sensitivity analysis
Univariate sensitivity analysis was performed to assess the stability of the model’s assumptions on the study findings.In this study,the screening coverage was 50%-100%,discount rate was 0-5%,screening and treatment costs varied by ±20%,and the sensitivity of screening techniques varied by ±5%.Univariate sensitivity analysis showed that the results were most sensitive to variations in discount rate and screening and treatment costs,and least sensitive to variations in the sensitivity of screening tests.However,screening coverage had no effect on the results.Using CER of triennial screening as an example,these results are shown inFigures 4-6.The PSA results were presented inFigure 7in the form of CEACs.The frontier is formed by selecting only those strategies that have the greatest net benefits at different willingness to pay threshold.As shown,if a decision maker is willing to pay between 10,000 RMB and 120,000 RMB per life year,HPV DNA testing every five years would provide the greatest net benefit.If the willingness to pay is over 120,000 RMB per life year,HPV DNA testing every three years is identified as providing the greatest net benefit.
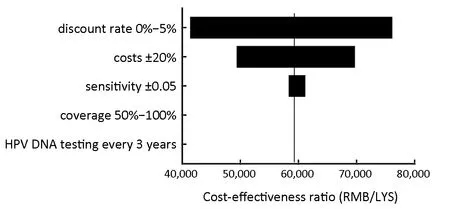
Figure 4 Tornado diagram:univariate sensitivity analysis showing the range of CERs of HPV DNA testing every 3 years.The vertical line represents the base-case analysis CERs.CERs,costeffectiveness ratios;HPV,human papillomavirus.
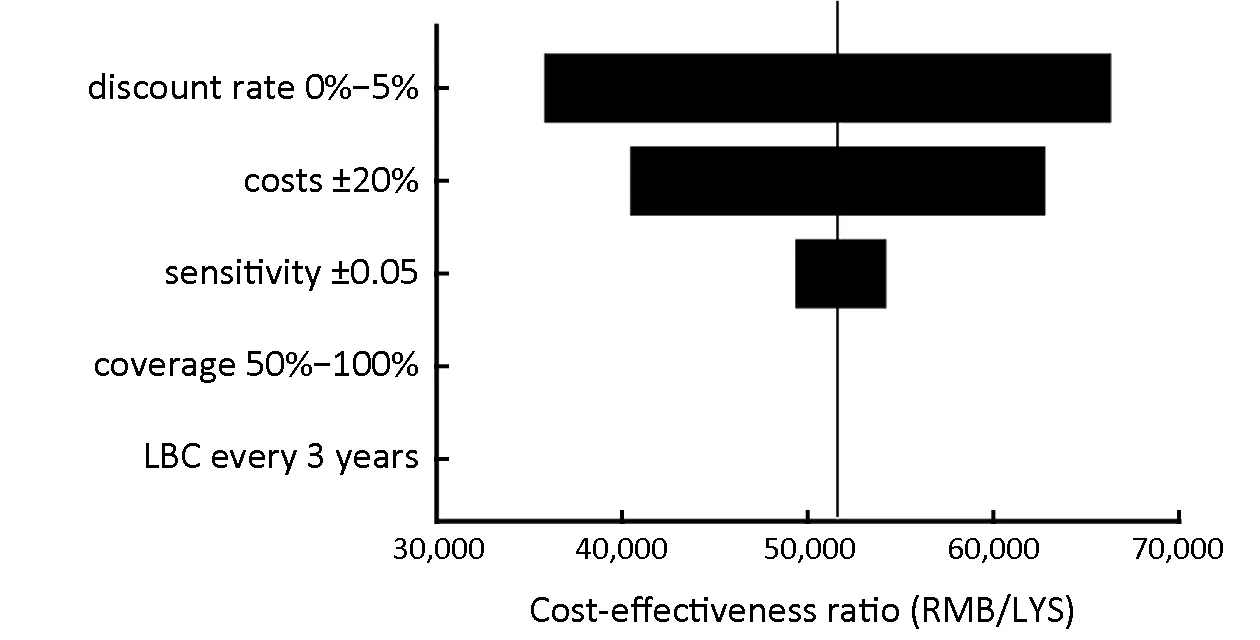
Figure 5 Tornado diagram:univariate sensitivity analysis showing the range of CERs of LBC every 3 years.The vertical line represents the base-case analysis CER.CER,cost-effectiveness ratio;LBC,liquid-based cytology.
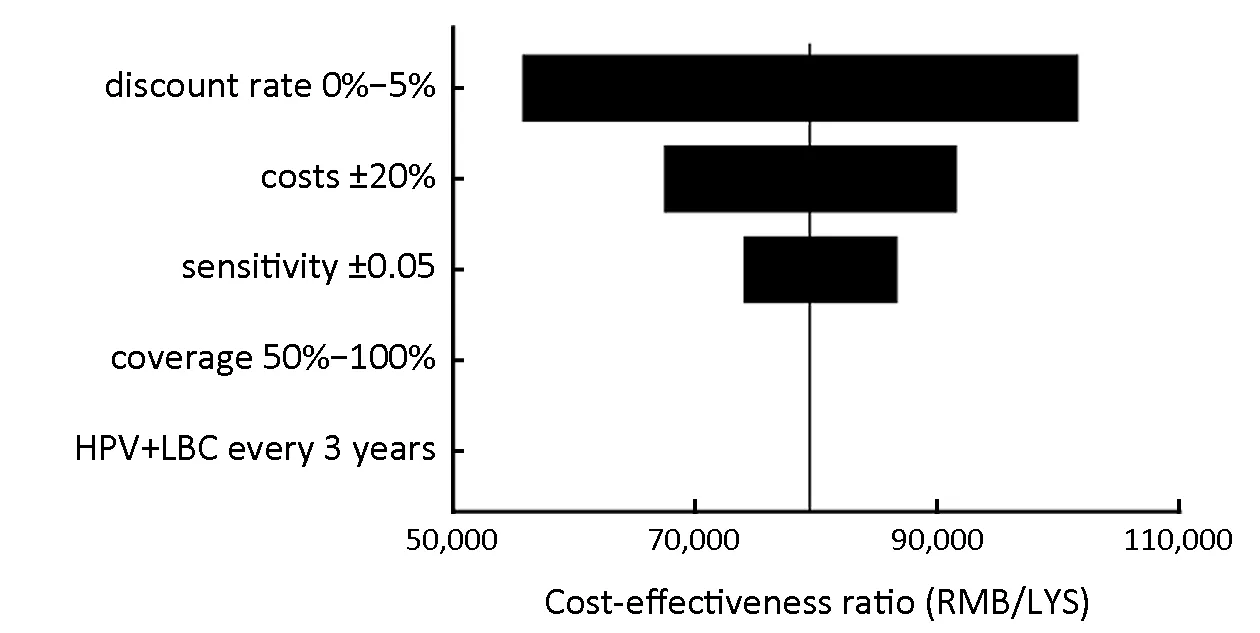
Figure 6 Tornado diagram:univariate sensitivity analysis showing the range of CERs of HPV+LBC every 3 years.The vertical line represents the base-case analysis CER.CER,cost-effectiveness ratio;HPV,human papillomavirus;LBC,liquid-based cytology.
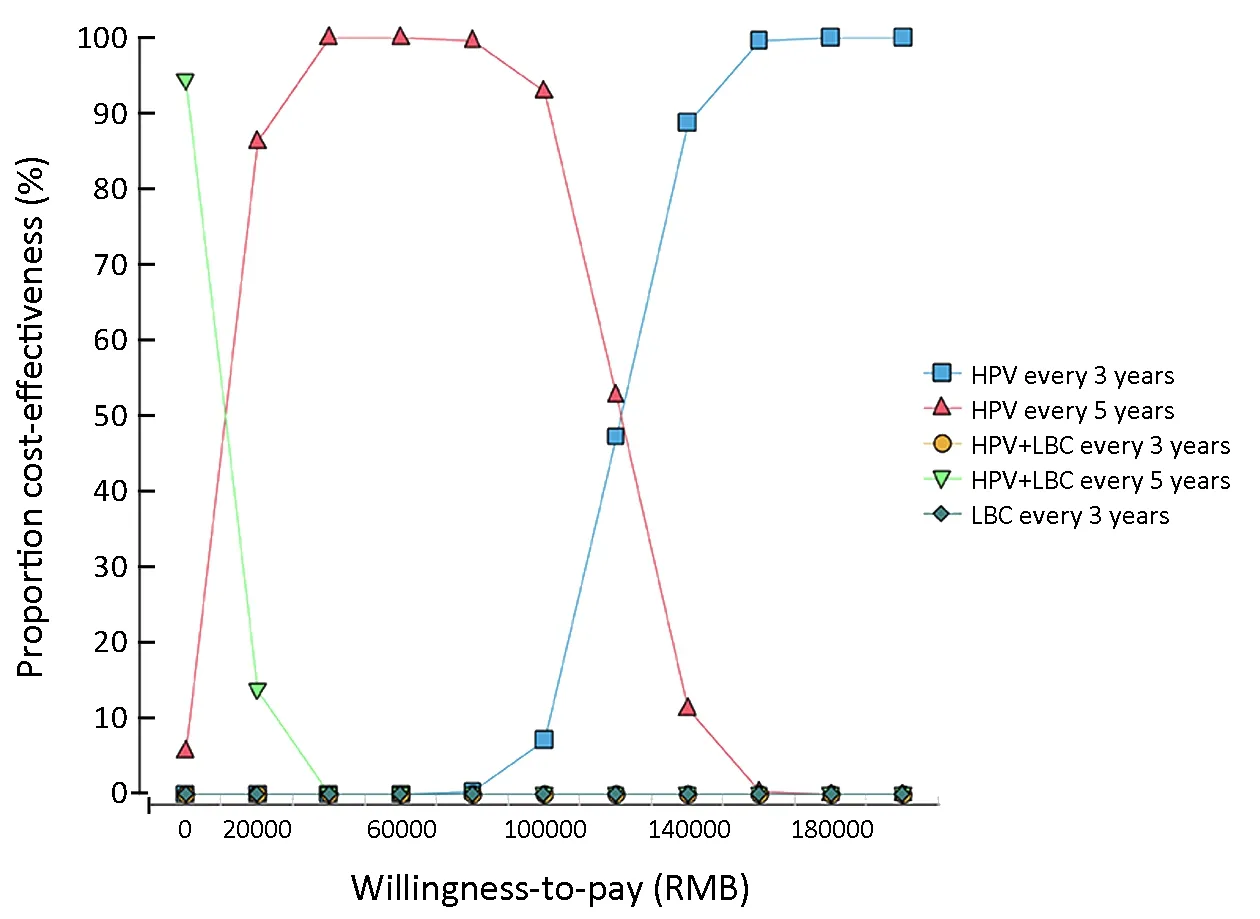
Figure 7 PSA results presented in the form of cost-effectiveness acceptability curves.PSA,probabilistic sensitivity analyses;HPV,human papillomavirus;LBC,liquid-based cytology.
Discussion
This study has presented a comprehensive health economic analysis of five screening strategies for cervical cancer in urban China.The analysis incorporated setting-specific information into the risks of HPV infection,screening and treatment procedures,and the costs associated with screening,diagnosis and treatment.In this study,HPV DNA testing every three years,HPV DNA testing every five years,LBC every three years,and HPV+LBC every five years were dominant strategies.HPV DNA testing every three years was the most effective strategy,followed by HPV DNA testing every five years and LBC every three years,while HPV+LBC every five years was the least effective strategy.Consistent with another analysis in the USA (25),this study showed that HPV screening is more effective than cytology,and is an alternative to co-test screening.
In accordance with the WHO recommendation for health economic assessment (24),the CERs of HPV DNA testing every five years,LBC every three years and HPV DNA testing every three years were found to be less than China’s GDP per capita,and could be considered very cost-effective.The CERs of HPV+LBC every three years and HPV+LBC every five years were below three times GDP per capita,and could be considered cost-effective.Single testing was better than co-testing,so we do not recommend HPV+LBC for cervical cancer screening in urban areas.
These findings suggested that HPV DNA testing significantly reduced the cumulative risk of cervical cancer.A study in Thailand (26) showed that HPV DNA testing had a higher sensitivity for detecting high-grade precancerous lesions (8-11),possibly facilitating early detection and treatment,which was consistent with our results.In addition,our findings showed that HPV DNA testing alone can save more life years,increase QALYs,and gain more benefits than LBC testing alone.This was consistent with the findings of Huhet al.(27) that HPV testing was more effective than cytology in developed countries.Preliminary unpublished findings have indicated that only 35% of medical institutions can conduct cytological examination at the grassroots level,and 80%can conduct HPV DNA testing in China.In addition,due to the strong subjectivity and poor repeatability of cytological examination,and the various influencing factors during the process of sampling,preparation and diagnosis,it is necessary to establish a high-quality cytological examination system.LBC examination is a difficult process that requires professional production,long training cycle to train well-trained and skilled film reading cytology technicians,and involves huge cost.HPV DNA testing has the advantages of objective and rapid results,easy repeatability,etc.Moreover,as the HPV DNA cervical cancer screening program can be quickly developed in the grassroots medical and health institutions,its practical applicability is more extensive.Therefore,HPV DNA testing has better feasibility than LBC.
The results of incremental cost-effectiveness analysis showed that HPV DNA testing every three years costs an additional 160,206.14 RMB per additional LYS as compared to HPV DNA testing every five years.Although HPV DNA testing every three years is more effective than HPV DNA testing every five years,the cost for each additional LYS is high and the general population in China is not willing to pay for it.Therefore,HPV DNA testing every three years is acceptable for cervical cancer screening in economically developed urban areas.The cost of each additional LYS by HPV DNA testing every five years was 17,636.01 RMB as compared to LBC every three years.HPV DNA testing every five years is more effective than LBC every three years,and the cost of each additional LYS is low,so HPV DNA testing every five years can be the first choice for cervical cancer screening in urban areas.Although LBC every three years is not as effective as HPV DNA testing every five years,the cost of LBC every three years is low,which makes it very cost-effective.Hence,it can be recommended as a cervical cancer screening strategy in urban areas.The majority of the recent guidelines for screening in developed countries (28,29) recommend that females aged 30-65 years old should be screened every three years by cytology,which is associated with sufficient economic strength,optimal medical service facilities and relatively high medical service level in developed countries.However,compared with HPV testing,fewer staff can provide cytological examination in China since it is more difficult and expensive to train a cytology professional (30).Therefore,it is difficult to popularize cytological examination screening program in China.
In the univariate sensitivity analysis,the altering assumptions included the discount rate,costs of screening and treatment,sensitivity of screening test,and screening coverage.We found that the lower the discount rate,the lower was the cost per LYS,and this finding was generally consistent with a study from Sweden (31).The reductions in the costs of screening and treatment had the same trend as the discount rate.Myerset al.used a Markov model to map the natural history of cervical cancer and examined the effects of changing the sensitivity and specificity of an unspecified screening test.They observed screening intervals of 1-5 years and found that at every interval,increased sensitivity resulted in increased cost even when the cost of the test was held constant.This was attributed to the increased cost of evaluation and treatment of lowgrade lesions that were identified in greater numbers with increased sensitivity (32),so the CERs of screening strategies also increased.This was consistent with our results.
This study had some limitations.For example,screening compliance was assumed to be 100%.All patients with or without cervical cancer screening were diagnosed and received appropriate standard treatment.Adverse reactions to treatment were not considered.This ideal hypothesis may overestimate the long-term effects of screening.However,the purpose of this study was to compare the effects of different screening programs in order to identify an appropriate cervical cancer screening program.Since the above hypothesis had the same impact on each screening program,it had negligible impact on the results.In addition,some of the parameters in this study were from international studies,so the representativeness of the results may be affected.However,the initial probability,sensitivity and specificity,screening and treatment costs,and other important parameters used in the study model were all derived from numerous large domestic research projects.Therefore,the findings of this study are generally representative,and can reflect the situation of screening programs in Chinese population.
Conclusions
Screening can effectively prevent cervical cancer.In this study,HPV DNA testing every three years,HPV DNA testing every five years,LBC every three years,and HPV+LBC every five years were dominant strategies.HPV DNA testing every three years was the most effective strategy,followed by HPV DNA testing every five years and LBC every three years,while HPV+LBC every five years was the least effective strategy.Therefore,HPV DNA testing every five years or LBC every three years should be recommended in urban China.HPV DNA testing every three years is acceptable in developed regions.
Acknowledgements
This study was supported by the National Health Commission of the People’s Republic of China (formerly the Health and Family Planning Commission) of China(No.201502004).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2019年6期
Chinese Journal of Cancer Research2019年6期
- Chinese Journal of Cancer Research的其它文章
- Prediction of pathological nodal stage of locally advanced rectal cancer by collective features of multiple lymph nodes in magnetic resonance images before and after neoadjuvant chemoradiotherapy
- An elevated preoperative serum calcium level is a significant predictor for positive peritoneal cytology in endometrial carcinoma
- Relationship between inter-α-trypsin inhibitor heavy chain 4 and ovarian cancer
- Diagnostic value of negative enrichment and immune fluorescence in situ hybridization for intraperitoneal free cancer cells of gastric cancer
- Stomatin plays a suppressor role in non-small cell lung cancer metastasis
- Genomic dissection of gastrointestinal and lung neuroendocrine neoplasm
