An elevated preoperative serum calcium level is a significant predictor for positive peritoneal cytology in endometrial carcinoma
Xingchen Li,Yuan Cheng,Yangyang Dong,Boqiang Shen,Xiao Yang,Jiaqi Wang,2,Jingyi Zhou,2,Jianliu Wang
1Department of Obstetrics and Gynecology,Peking University People’s Hospital,Beijing 100044,China;2Beijing Key Laboratory of Female Pelvic Floor Disorders Diseases,Beijing 100044,China
Abstract Objective:To evaluate preoperative serum calcium concentration and investigate the association between calcium level and positive peritoneal cytology in endometrial carcinoma (EC).Methods:A total of 510 patients who were diagnosed with EC and had surgery were initially enrolled in this study at Peking University People’s Hospital between January 2012 and December 2016.Clinical characteristics and preoperative serum calcium,albumin,carbohydrate antigen (CA)125,CA19-9,carcinoembryonic antigen(CEA) were extracted from patient records and evaluated according to postoperative peritoneal cytology.Predictive factors were assessed with Cox univariate and multivariate analyses.Factors selected from multivariate analysis results were used to build a predictive model.Results:A total of 510 patients are identified in our database and 444 patients who fulfilled inclusion and exclusion criteria are included in this study.Univariate analysis revealed that ionized calcium concentration was closely related to positive peritoneal cytology,tumor grade and lymph-vascular space invasion (LVSI).Moreover,peritoneal cytology was significantly associated with hypertension,tubal ligation,serum CA125,CA19-9,CEA and ionized calcium level.Multivariate analysis revealed that albumin-adjusted calcium level,CA125 and tubal ligation were independent predictive factors of positive peritoneal cytology (P<0.05).A combination of ionized calcium level with the other two indexes yielded significantly great area under the curve (AUC=0.824).Conclusions:This study enhanced the value of preoperative ionized calcium level.We also identified several potential biomarkers to predict positive peritoneal cytology in EC patients before surgery.
Keywords:Endometrial carcinoma;serum calcium;peritoneal cytology;logistic regression;predictive model
Introduction
Endometrial carcinoma (EC) is the most common gynecologic cancer in developed countries (1).EC ranked top 10 incidence of female patients in China (2,3).The incidence of EC reaches 63.4 per 10,000 in China in 2015(4) and is responsible for 74,000 deaths per year worldwide(5).Though the incidence and mortality rates of EC in China were relatively low compared with other countries,the significant increase in incidence rate and marked decrease in patient age suggest the urgency to prevention and control (6).In 2009,the Federation International of Gynecology and Obstetrics (FIGO) revised EC staging system (7).Positive peritoneal cytology from the current staging qsystem is lack of evidence regarding the prognostic impact on EC and is removed from the EC stage.However,there are mounting evidences showing that there is a decreased survival in women with EC who have abnormal peritoneal cytology with EC,including a 2013 report of 14,704 women with stage I/II EC from the Surveillance,Epidemiology and End Results (SEER)database shows that positive cytology predicted decreased survival (8),and the number is increasing (9).Despite many diagnostic modalities,none has proved to be high predictive value and it still remains difficult to reach a precise diagnosis of peritoneal dissemination.Peritoneal dissemination is usually diagnosed with an operation.Although intraoperative peritoneal washing cytology has been regarded as the golden standard to detect peritoneal cytology,there might be false negative rate in the diagnosis.It has been known that positive peritoneal cytology is associated with decreased overall survival in women with stage III.Treatment of these patients with adjuvant chemotherapy increases survival significantly (10).Therefore,identifying positive peritoneal cytology in EC is essential for predicting prognosis and conducting reasonable adjuvant therapy preoperatively.
Several molecular biomarkers have shown values in predicting the positive peritoneal cytology in gastric and colorectal cancer (11,12).However,to our knowledge,risk factors for positive peritoneal cytology in EC have been examined in few studies and are still unclear.Novel biomarkers are urgently needed for predicting abnormal peritoneal cytology in EC.Previously we found that ionized calcium influx to EC cells promotes their proliferation and migration (13).Serum calcium is playing an increasingly crucial role in many types of cancers such as breast cancer (14),ovarian cancer (15) and prostate cancer(16).It is also a novel parameter to assess metabolic syndrome in EC (17).Approximately 50% of calcium in blood is bound to albumin and not physiologically active.An estimate of the active fraction of serum calcium adjusts the serum calcium for the level of serum albumin (18).We therefore examined the association between tumor metastatic ability such as peritoneal cytology,lymphvascular space invasion (LVSI),tumor grade,lymphanode metastasis,FIGO stage and preoperative serum calcium level or albumin-corrected calcium level (ionized calcium).Finally we established a risk prediction model by a combination of ionized calcium level with some clinical features or biomarkers from multivariate analysis for abnormal peritoneal cytology.
Materials and methods
Patients
We conducted a retrospective,observational,noninterventional cohort study and included all EC patients who had surgical operation and identified from the comprehensive management system of medical record statistics from January 2012 to December 2016 in Peking University People’s Hospital (Beijing,China).For preoperative diagnosis,all patients underwent diagnostic curettage or hysteroscopy examination.The confirmation as primary EC was based on the histopathology of specimens after the surgery.Peritoneal washing lavage fluid was centrifuged at 1,500 r/min for 10 min to collect intact cells.The remaining precipitate was smeared on to four slides,fixed with acetone and stained with conventional haematoxylin and eosin.An experienced cytopathologist interpreted the samples.Detection of free tumor cells after the histopathological examination of the peritoneal washing fluid was accepted as positive cytology.We excluded the cases according to the following criteria:1) patients with a history of other malignancies;2) patients with hyperparathyroidism or other parathyroid diseases;3) patients with chronic kidney disease;or 4) missing clinical data or calcium and albumin values prior to surgery.The biologically active fraction of serum calcium was calculated by the following formula:serum albumin-corrected calcium(mg/dL)=total calcium (mg/dL)+0.8 × [4 -albumin(g/dL)].
Data collection
Patients’ demographics and clinical-pathological parameters include age,body mass index (BMI),menopausal status,diabetes,hypertension,tubal ligation history and hormone treatment.Laboratory findings,such as serum carbohydrate antigen (CA)125,CA19-9,carcinoembryonic antigen (CEA),calcium and albumin level,were retrospectively reviewed before surgery.To explore serum calcium level in different metastatic ability tumors,we collected some postoperative clinical features including ascites cytology,tumor grade,FIGO stage,lymphanode metastasis,LVSI,living status and recurrence.This study was approved by the Institutional Review Board of Peking University People’s Hospital (2015PHB116-01).
Statistical analysis
All analysis was performed by IBM SPSS Statistics (Version 21.0;IBM Corp.,New York,USA).Qualitative variables were expressed as numbers and percentages and were analyzed by the Chi-square test.Quantitative variables were reported aswith 95% confidence interval (95%CI) and analyzed by Student’st-test.Multivariate logistic regression model was used to identify the independent risk factors for positive peritoneal cytology in EC.Receiver operating characteristic (ROC) curve was used to assess the predictive power of risk factors for abnormal ascites.Statistical significance was set as P value less than 0.05.
Results
Patients’ selection
We selected the patients according to the criteria mentioned above and the flowchart detailing patient selection was shown inFigure 1.Table 1showed the demographics of patients with EC.The mean age of the group was 55.7±9.6 years old.The mean BMI was 26.2±4.7 kg/m2.Calcium concentration decreased compared with pre-adjustment calcium concentration.Over the 444 patients,the majority people were in menopausal state,and less people had complications such as hypertension,diabetes.The minority of the patients had tubal ligation history.Peritoneal cytology accounts for 10.8% of all the participants.The most common FIGO stage and grade was stage I and grade 2,which occupied the majority (79.7%and 43.5%,respectively).There were far less people who had lymph node metastasis (43,9.7%) than those who had not.
Association between serum calcium and metastatic capability
In this univariate logistic analysis,we assessed the relationship between low/high serum total/ionized calcium level and clinical outcomes such as tumor grade,FIGO stage,LVSI,lymph node metastasis and recurrence.This result revealed that the distribution of peritoneal cytology(P<0.001),tumor grade (P=0.007) and LVSI (P=0.012)were obviously different distributed in ionized calcium level group and what’s more,abnormal ascites showed the most significant difference.There were no statistically significant differences on FIGO stage,lymph node metastasis,recurrence between the two groups in this study (Table 2).
Risk factors for peritoneal metastasis in patients with EC

Figure 1 Flowchart detailing patient selection.CKD,chronic kidney disease;CA,carbohydrate antigen.
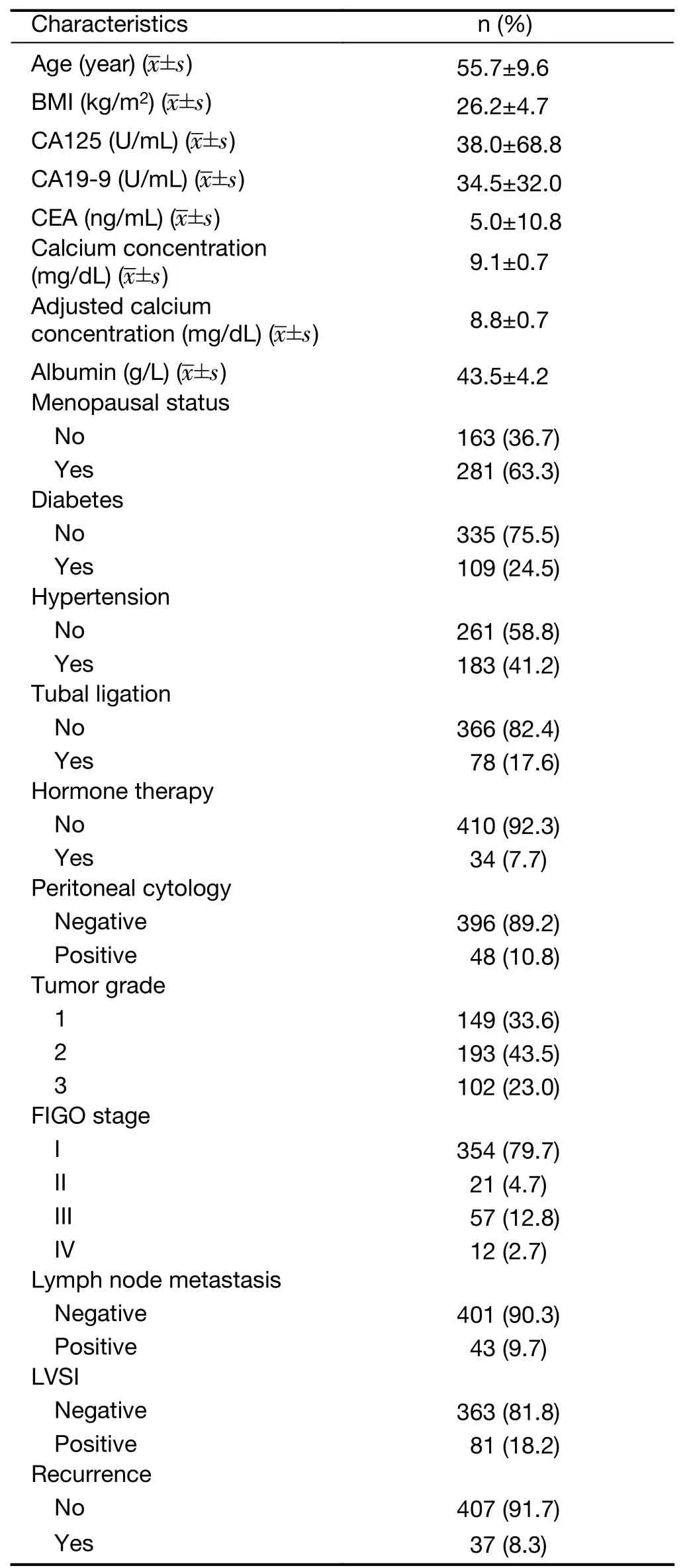
Table 1 Demographics of patients with endometrial carcinoma
In the former univariate analysis,we found that ionized calcium concentration had the most significant impact on peritoneal cytology.Furthermore,we detected the risk factors of positive peritoneal cytology.The univariate analysis revealed that there were no statistically significant differences on age,BMI,menopausal status,diabetes,hormone therapy,calcium and albumin level.However,preoperative ionized serum calcium level [odds ratio(OR)=6.061,95% CI:3.358-10.939,P<0.001]were significantly higher in patients with positive peritoneal cytology patients.Meanwhile,positive ascites were closely related to hypertension (OR=0.499,95% CI:0.256-0.972,P=0.041),tubal ligation history (OR=0.088,95% CI:0.012-0.649,P=0.017),CA125 (OR=1.007,95% CI:1.004-1.011,P<0.001),CA19-9 (OR=1.008,95% CI:1.003-1.013,P=0.018) and CEA (OR=1.021,95% CI:1.002-1.040,P=0.032) (Table 3).Multivariate logistic regression analysis indicated that serum ionized calcium level (OR=7.912,P<0.001),CA125 (OR=1.009,P<0.001)and tubal ligation (OR=0.060,P=0.010) were the independent risk factors correlated with peritoneal metastasis in patients with EC (Table 4).
Diagnosed accuracy of risk factors for predicting positive peritoneal cytology in EC patients
In order to identify the accuracy for diagnosing positive peritoneal cytology,we analyzed the ROC curves for different combinations of risk factors.Figure 2showed the ROC curve of any two of the three factors and the combined three factors for predicting the risk of positive peritoneal cytology in patients with EC.Based on the analysis,the results indicated that combined serum CA125,tubal ligation with ionized calcium level had the highest diagnostic accuracy for predicting abnormal peritoneal cytology in EC (AUC=0.821,P<0.001) (Table 5).
Discussion
In our study,we had observed a statistically significant correlation between positive peritoneal cytology and preoperative ionized serum calcium level.The correlation remained significant after multivariate analysis.Furthermore,we established a prognostic model of ionized calcium to predict abnormal peritoneal cytology.This study reinforced the potential benefit of using preoperative serum calcium to assess patients with EC and found that positive peritoneal cytology was associated with calcium for the first time.
Abnormal peritoneal cytology was found in about 11%of EC patients (19).Microscopic peritoneal metastasis wassuspected when cytopathologic examination of pelvic washings demonstrated malignant cells.Although the FIGO 2009 stage removed peritoneal cytology as staging criteria from the EC staging system (7),positive cytology is still an independent risk factor of survival in multiple studies in EC (20-22).There were many studies focusing on CA125 (23),stages (24),BMI (25),tumor grade (26) to predict peritoneal tumor cell in colorectal and prostate cancer.However,the biomarkers for prediction in EC were still unknown.Identifying available and inexpensive indexes of positive peritoneal cytology had a meaningful benefit for timely intervention and prevention.Thus,we carried out this study to determine the risk factors for patients’clinicopathological parameters of abnormal peritoneal cytology.
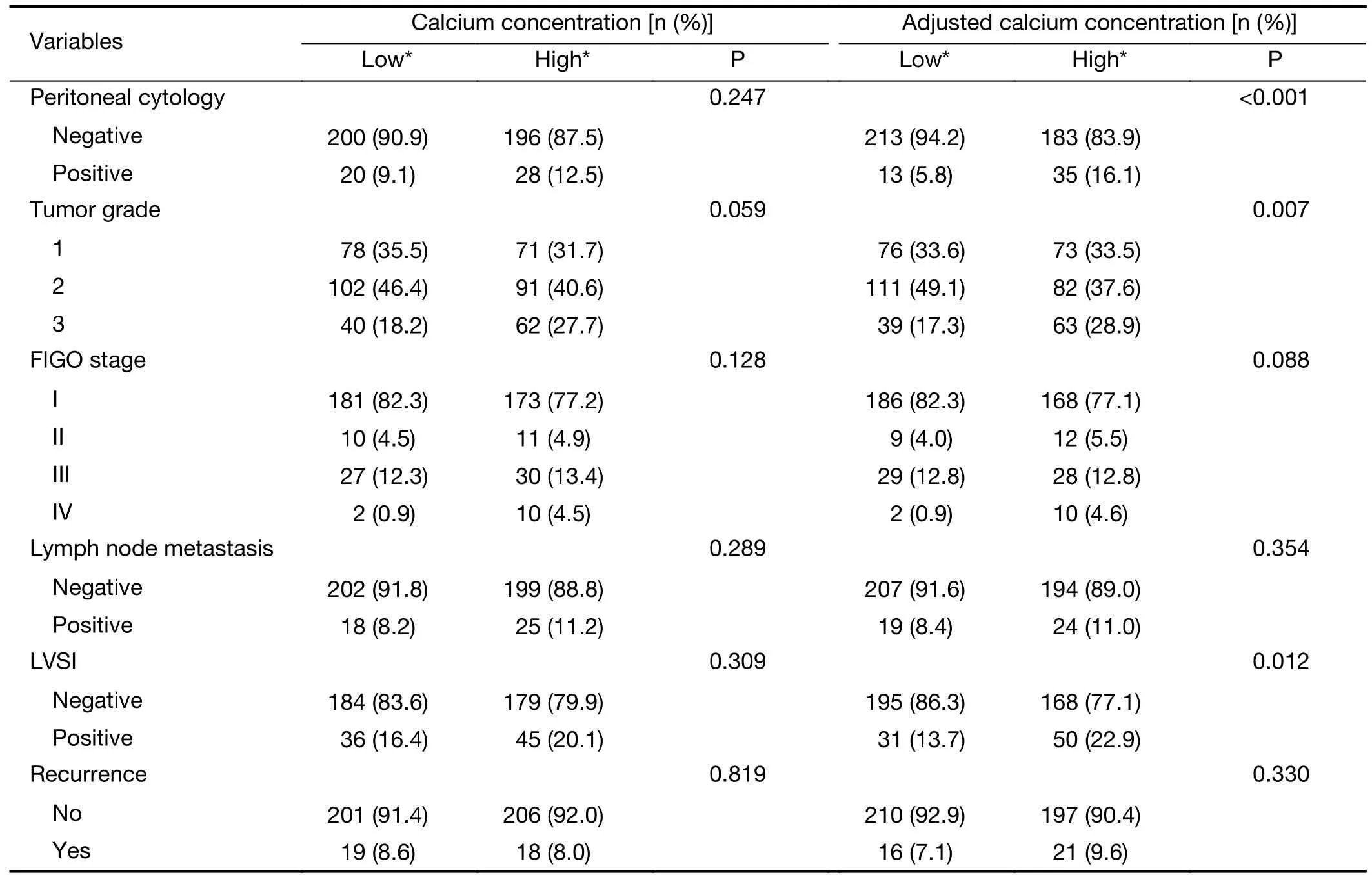
Table 2 Association between serum total/ionized calcium level and clinical parameters
Based on the analysis of this study,hypertension,tubal ligation,serum CA125,CA19-9,CEA levels and ionized serum calcium were found to be significantly correlated with abnormal ascites results.Liet al.revealed that tubal ligation was associated with lower possibility of peritoneal metastasis,which is in line with our results (27).Our group had also early found that serum calcium is also a biomarker for metabolic syndrome in EC.Calcium and its related channels were found to promote migration in EC,indicating that EC cells may require a high Ca2+microenvironment and more active Ca2+entry into cells.The association between higher serum calcium and different cancers had long been reported.Total and ionized serum calcium could elevate risk for fatal prostate cancer (16) and act as a risk factor in bone metastasis in bladder cancer (28),breast cancer (29) and discriminate malignant pelvic masses from benign ones (30),which agreed with our results that elevated calcium value was a negative prognostic factor for positive cytology in peritoneum.In this study,the multivariate analysis results showed that ionized serum calcium was an independent risk factor for positive peritoneal tumor cell (OR=7.912,95% CI:4.033-15.520,P<0.001).It meant that the risk of developing positiveperitoneal cytology was higher when the serum calcium elevated in patients with EC.
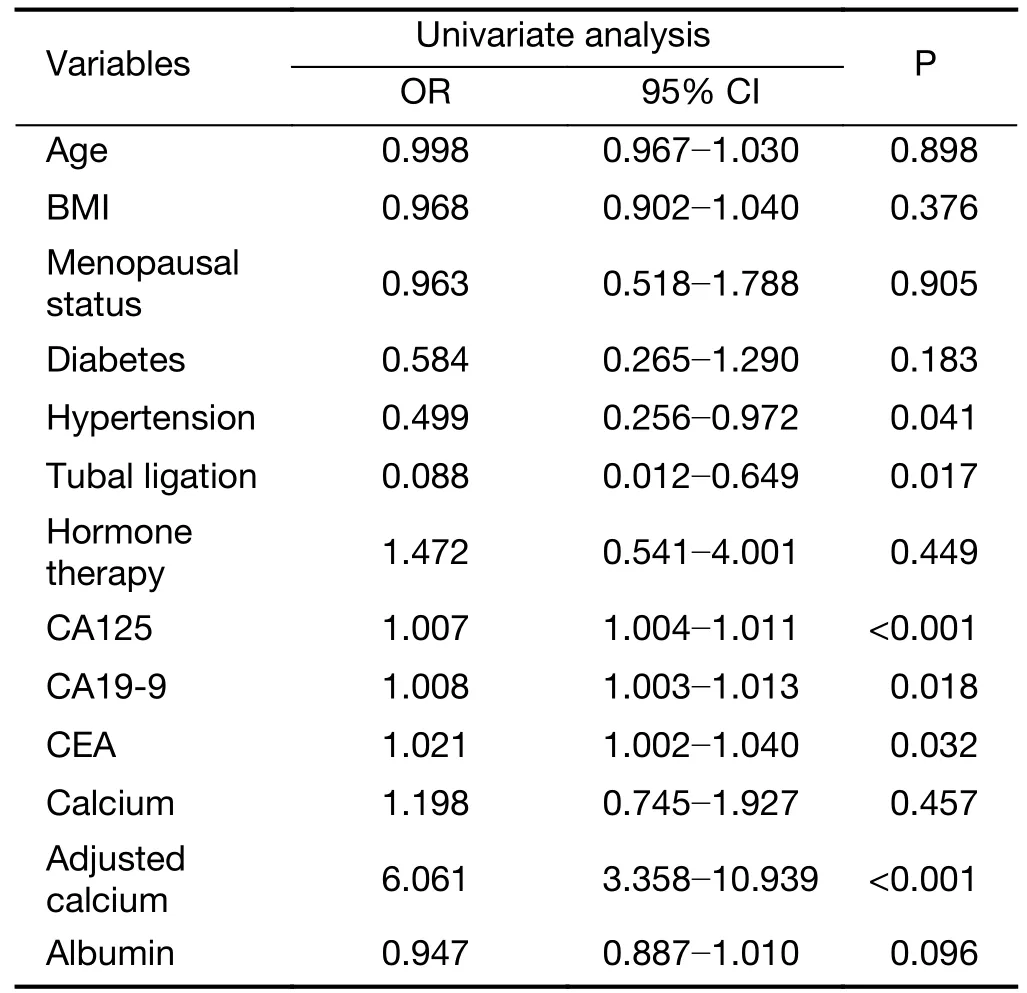
Table 3 Univariate analysis of clinicopathological parameters between patients with positive or negative peritoneal cytology
Calcium acted as a predictive role in many cancers,such as prostate cancer (31),urothelial carcinoma (32),renalcancer (33),ovarian cancer (34) and breast cancer (35) and the combination of risk factors appeared to be more accurate for predicting peritoneal metastasis (36).In the present study,we also analyzed the predictive accuracy of combined risk factors for predicting peritoneal tumor cell in patients with EC.Compared with two-combined factor ROC curves,combination of ionized calcium with serum CA125,tubal ligation had a higher accuracy for predicting positive peritoneal cytology.Therefore,combining serum calcium with other clinical indexes was a good way to predict metastatic peritoneal tumor cells.
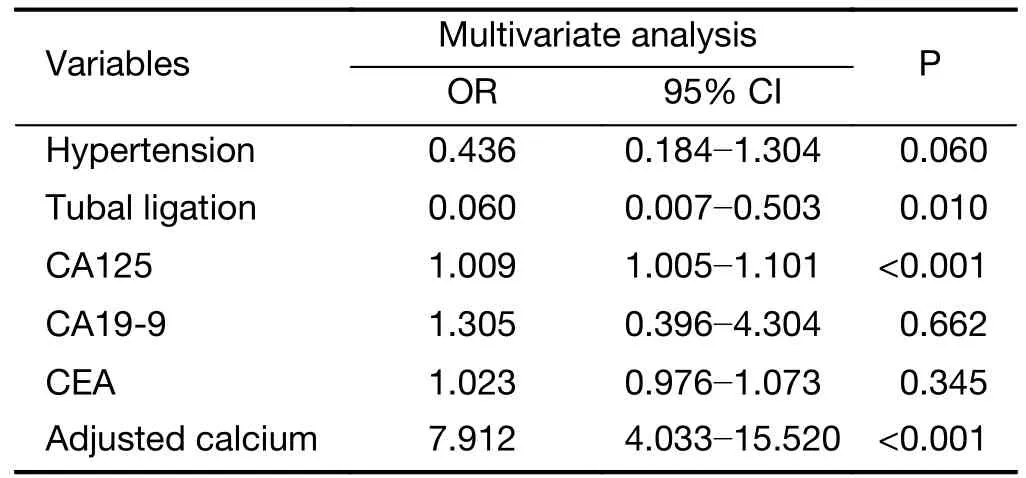
Table 4 Multivariate analysis of risk factors for endometrial carcinoma patients with positive peritoneal cytology
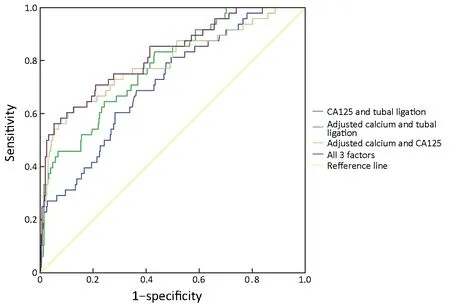
Figure 2 Receiver operating characteristic (ROC) curves for predicting risk of positive peritoneal cytology in endometrial carcinoma (EC)patients.CA,carbohydrate antigen.
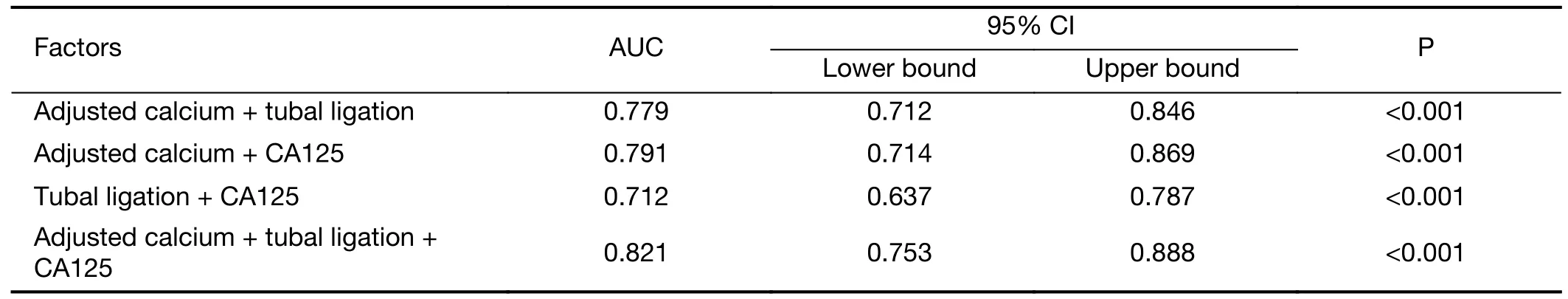
Table 5 AUC and P-value of risk factors for predicting positive peritoneal cytology with endometrial carcinoma
The influence the biological mechanism of serum ionized calcium had on peritoneal cytology remained to be determined.We speculated that the metastatic ability of peritoneal tumor cells might stem from calcium influx through calcium channel.An increase in plasma membrane calcium channel expression and activity sustained an elevated calcium entry,promoting higher cell proliferation and migration in most cases (37).For example,T-type voltage-gated calcium channel increased calcium influx and enhanced the metastatic ability of breast cancer cells (38).Piezo2 channel regulated cell cytoskeleton and metastasis by increasing intracellular calcium concentration (39).Calcium changes the cytoskeleton (40) and surface stiffness(41) during the process of migration.Therefore,calcium may play a role in promoting metastasis by mediating cytoskeleton and mechanical characteristics of cancer cells.
Predicting peritoneal tumor cells is of great importance and value in EC patients.First,serum calcium is affordable and easily acquired because no extra examination is needed.Then,although pathological diagnosis is the gold standard for peritoneal cytology,the diagnosis becomes more precise when combined with other preoperative indicators like calcium level because the structure of abdominal cavity is too complex to obtain metastatic peritoneal tumor cells if the amount of tumor cell is very few.What’s more,it will guide the extent of peritoneal lavage during the surgery.If the level of preoperative serum calcium increases dramatically,it indicates that peritoneal cytology is likely to be positive and surgeons should be careful to avoid abdominal dissemination during the operation and flush the abdominal and pelvic cavity cautiously during the operation.Finally,the prediction of peritoneal tumor cells by increased serum calcium indicates that calcium and its channel may cause tumor cells to migrate and adhere,whose molecular mechanism needs further study.This study provides a new idea for the combination of clinical research and basic research.
Although the results of this study are interesting,there are still some limitations in it.First,this is a retrospective study and some of the patients’ records have missed,which leads to patients’ selection bias.Second,the study is conducted in a single medical center with relative small sample,which may not present the generalized characteristics of the whole population with EC.In the future,we plan to carry out a validation study in other centers and explore the mechanism of metastatic peritoneal tumor cells caused by calcium level.
Conclusions
This study suggested that ionized calcium concentration indicated metastatic ability including peritoneal metastasis,tumor grade and LVSI and it was also an independent risk factor for positive peritoneal tumor cells in patients with EC.Combination of ionized calcium with CA125,tubal ligation had the highest diagnostic accuracy for predicting positive peritoneal cytology.However,this study needs to conduct further external validation in clinical practice and the detailed mechanisms still need further study.
Acknowledgements
This study was supported by National Natural Science Foundation of China (No.81874108,No.81802607).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2019年6期
Chinese Journal of Cancer Research2019年6期
- Chinese Journal of Cancer Research的其它文章
- Prediction of pathological nodal stage of locally advanced rectal cancer by collective features of multiple lymph nodes in magnetic resonance images before and after neoadjuvant chemoradiotherapy
- Economic evaluation of cervical cancer screening strategies in urban China
- Relationship between inter-α-trypsin inhibitor heavy chain 4 and ovarian cancer
- Diagnostic value of negative enrichment and immune fluorescence in situ hybridization for intraperitoneal free cancer cells of gastric cancer
- Stomatin plays a suppressor role in non-small cell lung cancer metastasis
- Genomic dissection of gastrointestinal and lung neuroendocrine neoplasm
