Prognostic utility of NT-proBNP greater than 70,000 pg/mL in patients with end stage renal disease
Julio Perez-Downes, Carlos Palacio, Saif Ibrahim, Patrisha Shelley, Alan Miller, Pramod Reddy
?
Prognostic utility of NT-proBNP greater than 70,000 pg/mL in patients with end stage renal disease
Julio Perez-Downes1, Carlos Palacio1, Saif Ibrahim2,*, Patrisha Shelley1, Alan Miller3, Pramod Reddy1
1Division of General Internal Medicine, University of Florida College of Medicine- Jacksonville, USA2Department of Interventional Cardiology, University of Alabama Birmingham, Birmingham, AL, USA3Division of Cardiology, Department of Medicine, University of Florida College of Medicine- Jacksonville, USA
J Geriatr Cardiol 2018; 15: 476?478. doi:10.11909/j.issn.1671-5411.2018.07.002
End stage renal disease; Heart failure; Heart failure reduced ejection fraction; Mortality; NT-proBNP
Natriuretic peptides are synthesized in ventricular myocytes and released into the circulation in response to increased myocardial wall stress.[1]Causes of myocardial wall stress include pulmonary hypertension, ventricular dilatation, as well as heart failure with reduced or preserved left ventricular function.[1]The 108 amino acid pro-brain natriuretic peptide (pro-BNP) is the cleavage product of the 134-amino acid hormone Pre-Pro-BNP,[2]which once released into circulation it further cleaves into C-terminal pro-BNP (32 amino acids, BNP) and N-terminal pro-BNP (76 amino acids, NT-proBNP).[3,4]Physiological effects of pro-BNP include reduction of sympathetic tone and activity of the renin-angiotensin system, promotion of vasodilation, natriuresis and diuresis.[5]
Multiple studies have determined the diagnostic and prognostic value of BNP and NT-proBNP in patients with heart failure with reduced as well as preserved ejection fraction.[6–10]Although defined NT-proBNP cutoffs support the diagnosis of heart failure among patients with normal as well as impaired renal function,[11]there is no consensus regarding specific NT-proBNP levels and their prognostic utility in patients with end stage renal disease (ESRD).[12–19]In addition, no study to date has evaluated the significance of severely elevated NT-proBNP values in mortality rates.
To evaluate the prognostic value of NT-proBNP values > 70,000 pg/mL, a total of 157 patients were identified at the University of Florida Health-Jacksonville (UF) in the time period of January 1st, 2012 through January 30th, 2016. Characteristics including age, gender, race, body mass index (BMI), medical therapy, ejection fraction (EF), renal function and presence of diastolic dysfunction were all gathered via systematic chart review. Patients without a transthoracic echocardiogram (TTE) or those missing E/e’ on tissue doppler imaging were excluded. One hundred and forty-one patients were included in the final analysis and mortality was determined by review of electronic medical records and the social security death index.
All-cause mortality was 45.39% over four years with a mean survival time of 204.1 days (= 64, SD 274.6, Median = 94 days). No statistically significant difference in mortality was noted among patients with relation to gender (= 0.6116), race (= 0.5428), ESRD status (= 0.9163), E/e’ > 12 (= 0.6740), medical treatment (= 0.9310), BMI (= 0.2295), diastolic heart failure (HF) (= 0.5644), systolic HF (= 0.5076) and combined systolic and diastolic HF (= 0.6757)
In a sub-sample analysis among patients with systolic HF, there was a statistically significant difference in mortality (= 0.0089) and survival (= 0.0043) among patients with an EF of < 25%. Patients with EF < 35% revealed a trend towards decreased survival (= 0.0920). The best-fit logistic regression model predicting mortality contained only age [= 0.0203; odds ratios (OR): 1.0301, 95% confidence intervals (CI): 1.005–1.057] and an indicator variable for EF < 25% (= 0.0306). The odds of death were 2.5 (95% CI: 1.091, 5.934) times higher for those with EF < 25% compared to those with EF > 25% (Figure 1 & 2).
In view of the above findings, the study demonstrates that among patients with uniformly severely elevated NT- proBNP, heart failure and ESRD, EF continues to be a sig-nificant predictor of mortality. While elevated NT-proBNP levels in patients with ESRD are partially due to renal clearance, values exceeding 70,000 pg/mL are unlikely to be due solely to renal dysfunction.[4]Evidence suggests renal clearance of BNP and NT-proBNP to be equivalent, while additional clearance of NT-proBNP is present in liver and skeletal tissue.[20,21]Previous studies have demonstrated that neither length of time of hemodialysis nor duration of renal disease has significant correlation with NT-proBNP levels.[14]This suggests that while renal function plays a role in elevated NT-proBNP levels, left ventricular function is the most critical variable influencing mortality and NT- proBNP.
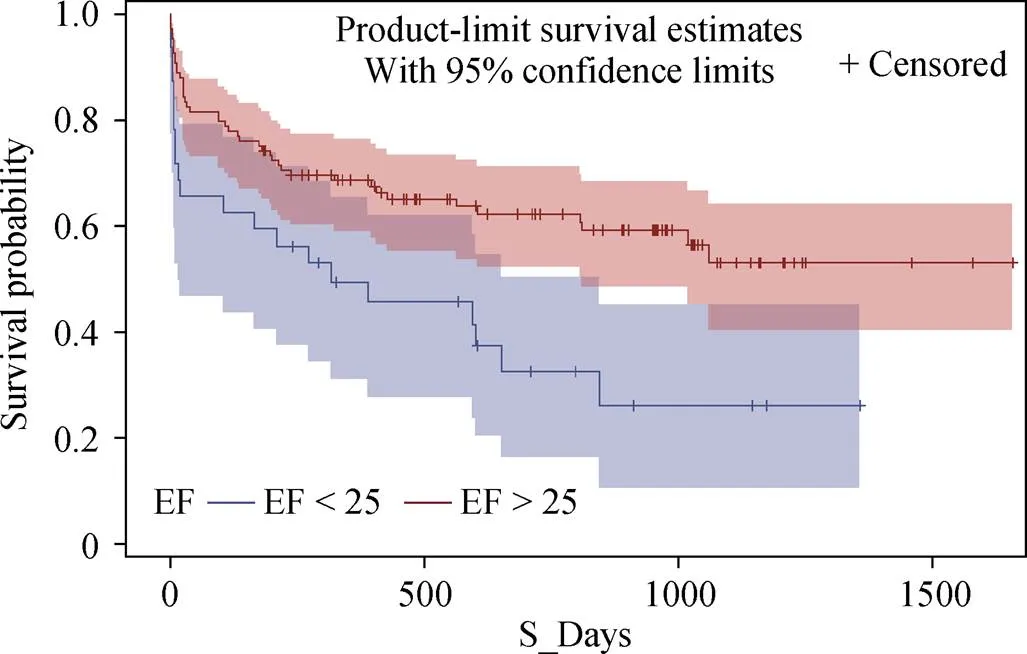
Figure 1. Survival estimates between patients with an EF < 25 versus those with an EF > or equal to 25 - Y-axis represents the probability of survival. The X-axis represents survival in number of days. The blue line represents those patients with an EF < 25%, while the red line represents patients with an EF > or equal to 25%. The shaded areas represent the 95% confidence intervals for the curves. Note the significant divergence between survival curves in the two populations.= 0.0043. EF: ejection fraction.
Figure 2. Survival estimates between patients with an ejection fraction of < 35% versus those with an ejection fraction > 35%.= 0.0920 for the small but appreciable divergence between survival curves among the two different populations. Y-axis represents the probability of survival. The X-axis represents survival in number of days. The blue line represents those patients with an EF >35%, while the red represents those with an EF < 35%. The shaded areas represent the 95% confidence intervals for the curves. EF: ejection fraction.
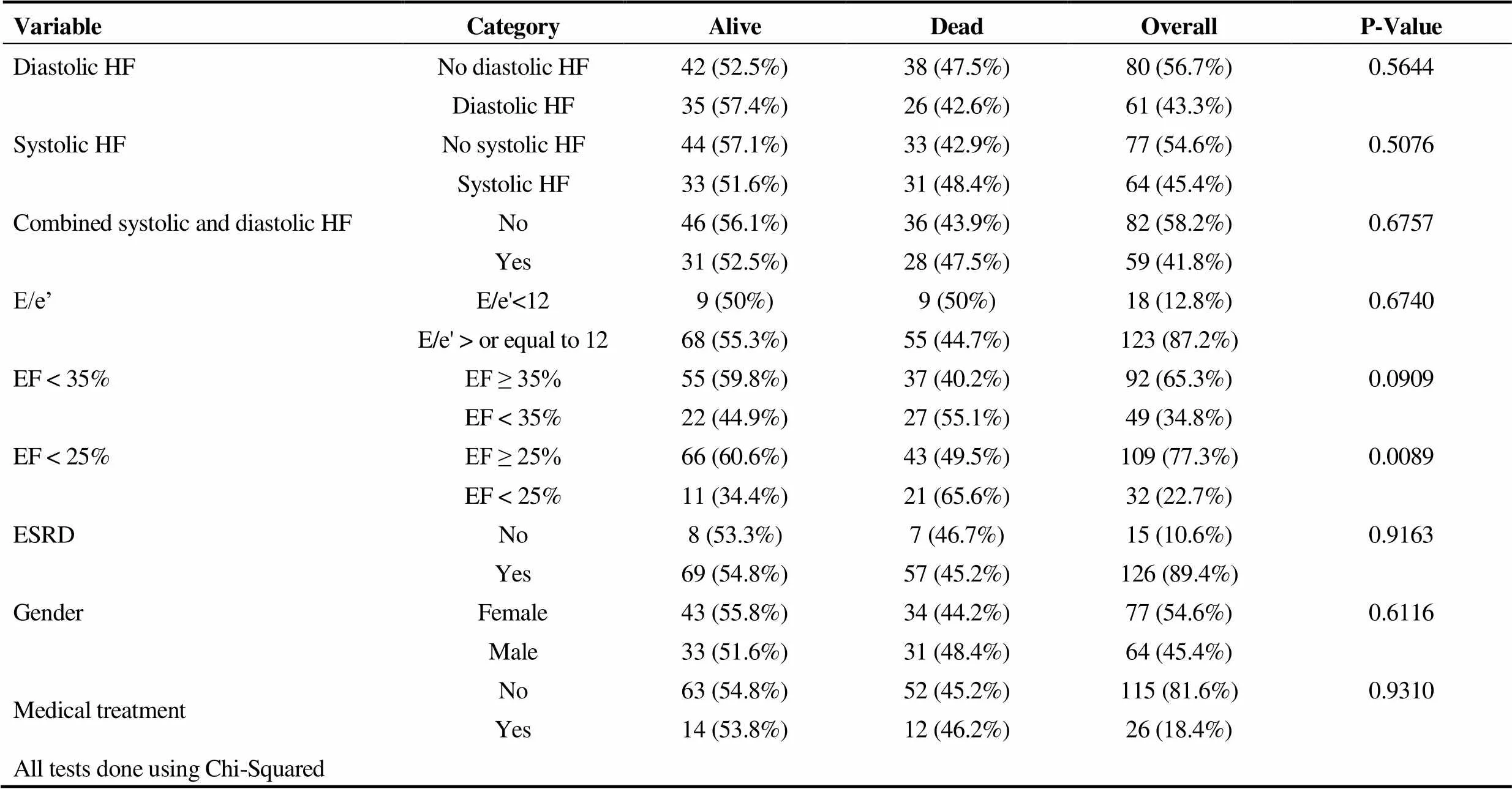
Table 1. Association between mortality rate and clinical variables among patients with NT-proBNP > 70,000 pg/mL -Tabulation and statistical analysis of variables which may affect mortality rates among patients with NT-proBNP > 70,000 pg/mL.
Data were presented as(%). Only EF < 25% is statistically significant. Medical treatment consists of angiotensin inhibitors, diuretics and beta blockers. ESRD: end-stage renal disease; EF: ejection fraction; E/e': Tissue Doppler from Echo; HF: heart failure;NT-proBNP: N-terminal pro-brain natriuretic peptide.
During the evaluation of renal function of our population, we incidentally discovered a large prevalence of ESRD. Pre-vious studies diverge on a normal NT-proBNP in patients with ESRD.[15,19,23]The prevalence of heart failure among patients with ESRD is estimated to be 31%, while the median survival is 36 months.[22]Despite the known decreased survival in patients with heart failure and ESRD, no previous study has demonstrated such a strong corre-lation between EF and mortality in patients with NT- proBNP > 70,000 pg/mL (Table 1).
Mortality rates in the studied population remained uniformly elevated in both systolic and diastolic HF. The subset of patients with severe systolic HF (< 25%) were noted to have 65.6% mortality over four years. We are unable to explain the occurrence of normal E/e’ in 12.8% of patients with diastolic HF, despite elevated NT-proBNP levels. Possible reasons for such observation include operator error or poor acoustic windows at the time of imaging.
In view of the above findings, we assert that among patients with NT-proBNP > 70,000 pg/mL and ESRD, left ventricular EF < 25% is an indicator of increased mortality rate. Utilization of a uniform NT-proBNP level allows for better characterization of variables significant in mortality prediction among patients with ESRD. It is essential to emphasize the importance of aggressive medical management of heart failure patients with ESRD to prevent such magnitude of NT-proBNP levels and decrease mortality rates.
1 Levin ER, Gardner DG, Samson WK. Natriuretic Peptides.1998; 339: 321–328.
2 Reddy P, Rohan S. Clinical utility of natriuretic peptides in left ventricular failure.2013; 106: 182–187.
3 Weber M, Hamm C. Role of B-type natriuretic peptide (BNP) and NT-proBNP in clinical routine.2006; 92: 843–849.
4 Kim HN, Januzzi JL Jr. Natriuretic peptide testing in heart failure.2011; 123: 2015–2019.
5 Braunwald E. Biomarkers in heart failure.2008; 358: 2148–2159.
6 van Veldhuisen DJ, Linssen GC, Jaarsma T,. B-type natriuretic peptide and prognosis in heart failure patients with preserved and reduced ejection fraction.2013; 61: 1498–1506.
7 Daniels LB, Maisel AS. Natriuretic peptides.2007; 50: 2357–2368.
8 Januzzi JL Jr, Rehman SU, Mohammed AA,. Use of amino-ternimal pro-B-type natriuretic peptide to guide outpatient therapy of patients with chronic left ventricular dysfunction.2011; 58: 1881–1889.
9 Parekh N, maisel AS. Utility of B-natriuretic peptide in the evaluation of left ventricular diastolic dysfunction and diastolic heart failure.2009; 24:155–160.
10 Komajda M, Carson PE, Hetzel S,. Factors associated with outcome in heart failure with preserved ejection fraction: findings from the Irbesartan in Heart Failure with Preserved Ejection Fraction Study (I-PRESERVE).2011; 4: 27–35.
11 Januzzi JL, van Kimmenade R, Lainchbury J,. NT- proBNP testing for diagnosis an short-term prognosis in acute destabilized heart failure: an international pooled analysis of 1,256 patients; The International Collaborative of NT-proBNP Study.2006; 27: 330–337.
12 DeFilippi C, Van Kimmenade RR, Pinto YM,. Amino- terminal pro-B-type natriuretic peptide testing in renal disease.2008; 101: 82–88.
13 Svensson M, Gorst-Rasmussen A, Schmidt EB,. NT-pro- BNP is an independent predictor of mortality in patients with end-stage renal disease.2009; 71: 380–386.
14 Madsen LH, Ladefoged S, Corell P,. N-terminal pro brain natriuretic peptide predicts mortality in patients with end-stage renal disease in hemodialysis.2007; 71: 548–554.
15 Rajagopalan S, Croal BL, Reeve J,. N-terminam pro-B-type natriuretic peptide is an independent predictor of all-cause mortality and MACE after major vascular surgery in medium-term follow up.2011; 41: 657–662.
16 Harrison A, Morrison LK, Krishnaswamy P,. B type natriuretic peptide predicts future cardiac events in patients presenting to the emergency department with dyspnea.2002; 39: 131–138.
17 Taylor CJ, Roalfe AK, Iles R,. The potential role of NT-proBNP in screening for and predicting prognosis in heart failure: a survival analysis. BMJ Open 2014; 4: e004675.
18 Kirk V, Bay M, Parner J,. N-terminal proBNP and mortality in hospitalised patients with heart failure and preserved vs. reduced systolic function: data from the prospective Copenhagen Hospital Heart Failure Study (CHHF).2004; 6: 335–341.
19 Sharma R, Gaze DC, Pellerin D,. Raised plasma N‐terminal pro‐B‐type natriuretic peptide concentrations predict mortality and cardiac disease in end‐stage renal disease.2006; 92: 1518–1519.
20 Maisel AS, Krishnaswamy P, Nowak RM,. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure.2002; 347: 161–167.
21 Palmer SC, Yandle TG, Nicholls MG,. Regional clearance of amino-terminal pro-brain natriuretic peptide from human plasma.2009; 11: 832–839.
22 Harnett JD, Foley RN, Kent GM,. Congestive heart failure in dialysis patients: prevalence, incidence, prognosis and risk factors.1995; 4: 884–890.
23 Osajima A, Okazaki M, Kato H,. Clinical significance of natriuretic pentides and cyclic GMP in hemodialysis pa-tients with coronary artery disease.2001; 21: 112–119.
Correspondence to: saif.ibr@gmail.com
 Journal of Geriatric Cardiology2018年7期
Journal of Geriatric Cardiology2018年7期
- Journal of Geriatric Cardiology的其它文章
- Single-territory incomplete surgical revascularization improves regional wall motion of remote ventricular areas: results from a propensity-matched study
- A three-year longitudinal study of the relation between left atrial diameter remodeling and atrial fibrillation ablation outcome
- Particular evolution in a 72-year-old diabetic patient with acute coronary syndrome
- Management of hypertensive crises in the elderly
- C-reactive protein aggravates myocardial ischemia/reperfusion injury through activation of extracellular-signal-regulated kinase 1/2
- The effectiveness and safety of the RESTORE? drug-eluting balloon versus a drug-eluting stent for small coronary vessel disease: study protocol for a multi-center, randomized, controlled trial
