New Development and Technology of Sun Protection
Jiang Yihua, Bai Shan, Lu Jie, Mei Hexiang Symrise (Shanghai) Co., Ltd., China
Liu Wei
Dermatology Department of Air Force General Hospital of PLA, China
Sunlight may generate certain adverse effects on human skin while giving us warmth and energy. Since ancient times, human being started trying to protect skin from injury due to sunlight. Along with progress in sun protection technology, physiological knowledge of the scientific research to the skin, has been known deeply. The biological mechanism of premature aging of skin, cased by infrared ray and visible light, also becomes readily apparent.[1~3]
Influence of ultraviolet radiation on skin
Irritation from ultraviolet rays include UVA (315~400 nm), UVB (280~315 nm) and UVC (100~280 nm),arriving on the earth is very weak, because the majority is absorbed by the atmosphere and would not generate great direct harm to human body.[4]Reaching the earth,where the sunlight radiates onto skin, may lead to a release of a series of inflammatory mediums; the process of important medium induction is shown in Figure 1.As shown in Figure 1, the keratinocyte in the epidermis releases excessive free radicals decompose the lipid molecule of the cytomembrane directly, and induce the primary inflammatory factor leukotrienes (LTB4) and prostaglandin E2(PCE2) with the presence of enzymes. The other pathway of the free radicals damage is to increase the nucleoside transcriptase NF-kB, in order to prompt DNA to express more secondary inflammatory factors —tumor necrosis factor TNF-α and interleukin IL-1. The inflammatory factors and the proinflammatory factors may induce different inflammations of the skin through signal transduction and regulatory mechanisms, including erythema, swelling and induced hyperthermia. At the same time, collagen A and elastin are further decomposed due to activation of IL-1, increasing expression and activity of the matrix metalloproteinase A (MMP) cased by activation of IL-1, thereby leading to decreased elasticity and compactness which means skin aging.
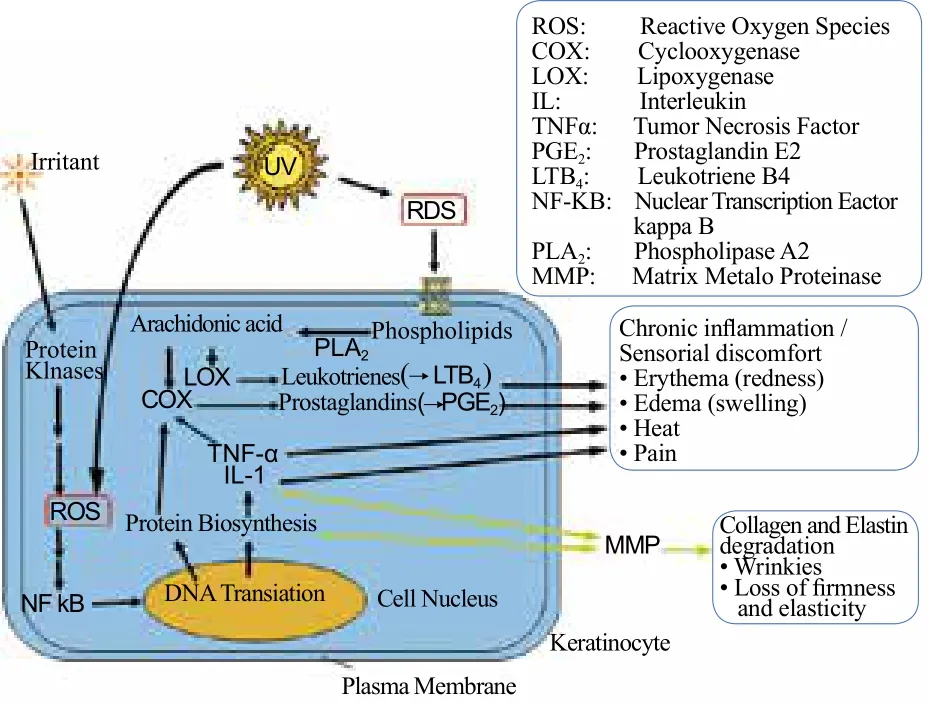
Figuer l. UV Induced inflammation and skin aging
Influence of AhR induced by UVB to the skin
Besides direct induction from the above-mentioned UVA and UVB, Fritsche, of the University of Düsseldorf in Germany, found that tryptophan on the skin might absorb UVB and form the coupled photoproduct FICZ(Forrmylindol-(2,3)-carhazole), and further enter into the cell nucleus after combining with AhR. This induces a release of cytochrome CYP1A1 and a series of reactions (Figure 2) in the cell nucleus, while stimulating epidermal growth factor (EGFR) through activating AhR.Fritsche[5]proved that FICZ is formed from tryptophan by Ultraviolet B irradiated. When that occurred in the cell, the tryptophan might lead to a series of reactions,such as oxidative stress (namely waste glutathione GSH and increased formation of anionic peroxidase), atopic dermatitis, and induction of squamous-cell carcinoma through activating P450 enzyme. This path was consistent with the path of influence of air pollutants on the skin.

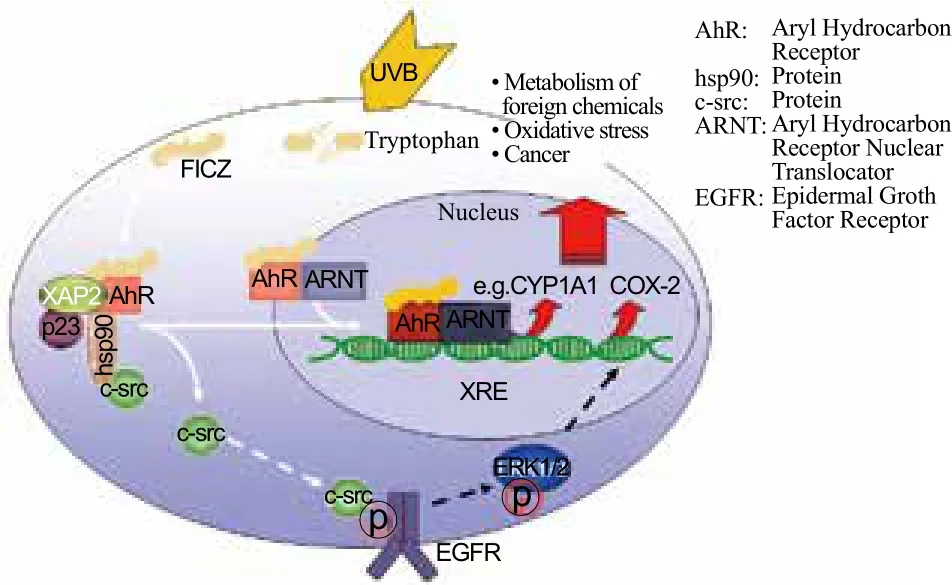
Figure 2. Skin damage through AhR, which is induced by UVB
Influence of visible light to skin
Visible light (400~ 700 nm), carries little enegy, and mainly generates free radicals and hyperpigmentation of the skin. Visible light may penetrate biological tissue and generate ROS to the skin, with the activation of endogenous photosensitizers induced by the photon.[6,7]In order to measure the relative value of UVA, UVB and visible light to ROS quantitatively, the explant skin model(using a series of sunscreens), was exposed to sunlight,at noon, in the open air. The result showed that in the ROS induced, UVA was 46%, UVB was 4% and visible light was 50%.[6]The skin chromophore from the visible light included heme, melanin, bilirubin, riboflavin and porphyrin.[8]In the presence of a dosage equal to 15~90 min sunlight irradiation, visible light might induce the generation of inflammatory factors (including IL-1, IL-6, IL-8 and GM-CSF) and increase the amount of degradation enzymes (MMP-1 and MMP-9) in the skin epidermis. Generation of free radicals was proved through in vivo tests with chemiluminescence method and biopsy. Like UVA, visible light could affect DNA through oxidizing the DNA base,[10,11]however, would not form dimer.[7]
Visible light led to hyperpigmentation in the dark skin group (Filz-patrick type IV-V),[12]and was suspected to aggravate chloasma.[7]Duteil, et al. found that the blue light band in visible light might lead to increasing hyperpigmentation of the skin, and the hyperpigmentation induced by the free blue light was more stubborn (still existing after 3 months) than hyperpigmentation induced by UVB, while the red light hardly led to hyperpigmentation.[14]
Influence of infrared rays on skin
The influence of infrared radiation on the skin has received more and more attention in recent years. The band of infrared rays affecting human skin is 700~1, 000 nm.Peter Schroeder, et al. comprehensively researched the influence of infrared rays on skin.[2]Infrared rays affected the skin by two paths: IRA (near infrared rays) interacting with CcO (cytochrome C oxidase), thereby leading to insufficient generation of energy and increasing ROS,due to damage of the transfer pathway of mitochondrial electrons. This mitochondrial dysfunction might lead to an expression of degraded mitochondrial signals from the mitochondria to nuclear DNA, and further lead to excessive expression of MMP-1 and 1-type precollagen(COL1A1). Further, an increase of MMP promoting degradation of collagen, and a decrease of COL1A1 expression led to decrease of new collagen, thereby leading to formation of photoaging wrinkles.
The other path was related to the thermoreceptor TKPV1 (protein thermoreceptor of transient receptor potential vanilloid 1 pathway) on surface of the cytomembrane, especially the fibroblast membrane.This mechanism is involved in thermal induction and TKPV1 activation in the presence of protein kinase C(PKC), to make the calcium ion enter into the cell. In the fibroblast, TKPV1 promoted expression of MMP-1, through regulating the flow of the calcium ion and accelerated degradation of collagen and presenility of skin at the levels of mRNA and protein. In the sensory neuron cells of skin, TKPV1 activated and promoted release of neuropeptides, such as substance P (SP); and permeability of blood capillaries could be improved by increasing synthesis of vascular epidermal growth factors. Moreover,synergistic activation of TKPV1 could further accelerate inflammation and skin aging.
New strategy of sun protection

According to the above-mentioned mechanisms, one all-around sun protection product should include the following ingredients (Figure 3): a sun screen to keep off the direct harm of ultraviolet rays to the skin, an antagonist containing aromatic hydrocarbon receptors and blocking the transfer of AhR, and an antioxidant restraining the signal transduction of free radicals to the cell factors and limiting its activation to MMP.There is no absorbent or screening agent available for infrared rays; however, MMP inhibitor can be selected because IRA radiation leads to premature aging by MMP-expression. Activation of thermoreceptors, induced by IRA, radiation leads to an increase of permeability of blood capillaries and thermal stress damage. Therefore,the THPV1 antagonist and algefacient are considered for use, in order to restrain the thermal stress damage and improve comfort when using a sunscreen product.Moreover, an effective inflammation factor inhibitor can restrain inflammation factors induced by ultraviolet rays,and prevent the irritation from certain ingredients in the sunscreen product to skin during use.
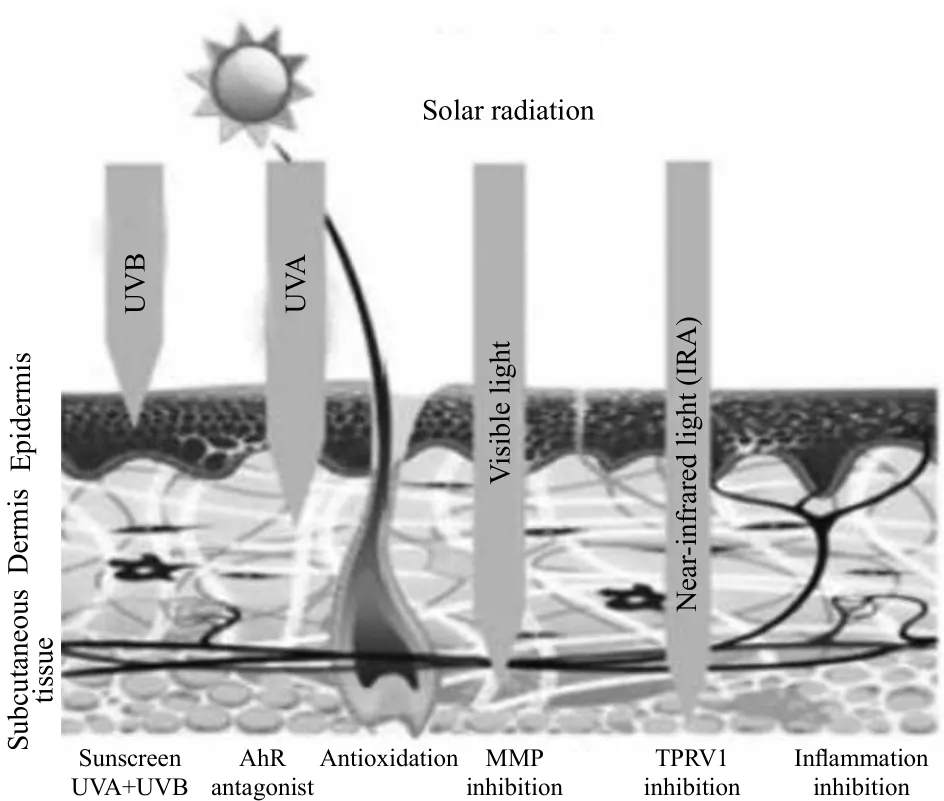
Figure 3. Impact of sun light and sun protection
Sunscreen
There are two categories of sunscreen agents: organic and inorganic. According to different spectral bands of UV absorption, or shielding of various sunscreens, broadspectrum sunscreens protect against both UVA and UVB can be made. When selecting a sunscreen product, you should select a product marked with suitable SPF value(UVB protection) and PA value (UVA protection).
AhR antagonist
Cosmetics contain a little AhR antagonist. 2-benzal-5,6-dimethoxy-3,3-dimethyl- 1-indone (Trade name:SymHelios?1031), were used as an AhR antagonist for cosmetics and developed by the author’s company. HaCaT keratinocyte was cultivated for 1 h with SymHelios?1031 or 0.1% DMSO, and cultivated again for 4 h after being irradiated with 100 J/m2UVB. mRNA was extracted and the CYP1A1, COX-2, etc., were measured quantitatively.Through comparison, the results were decreased significantly in statistics. AhR and the cell nucleus were subjected to double-staining through a fluorescent labeling method during this study; the restraining effect of SymHelios?1031 to AhR, transferred to the cell nucleus,were observed through the fluorescence microscope.
Antioxidant
Free radicals on the skin, generated due to solar radiation, can be removed with a cosmetic in which an antioxidant is added, thereby protecting the skin more excellently. Common antioxidants include vitamin E,vitamin C, β-carotene, mangiferin derivative, etc.[15]Besides, resveratrol, carnosine, etc., are also efficient antioxidants. Sym Vital Age Repair (ginger root extract),developed by the author’s company, is one potent ingredient for resisting oxidation and inflammation. An experiment on human melanocytes and human excised skin, found that this product can effectively restrain hyperpigmentation caused by blue light.

Matrix Metalloproteinase (MMP) inhibitor
Infrared rays cannot be isolated with common methods; and the restraining of MMP decrease, caused by IRA (near-infrared radiation), was one method of effectively resisting aging due to infrared rays[16]. The author’s company found that carnosine (Trade name:Dmgosine? ), could restrain MMP expression; and the restraining effect of carnosine on the primary human dermal fibroblast to MMP-1, induced by IRA (wavelength:760~1,400 nm, light intensity: 360 J/cm2), was detected in the experiment. The experiment showed that the amount of carnosine added has a significant dose-effect relationship with the restraining of MMP-1 expression,induced by infrared ray.
Thermoreceptor TRPV1 antagonist
THPV1 is the protein thermoreceptor of the transient receptor potential vanilloid 1 pathway, and controls the flow of calcium in the skin. TRPV1 neuroreceptors may generate skin irritation and inflammation when activated by infrared rays, or other chemicals, leading to further presenility of skin. Trans-4-tert-butylcyclohexanol was used as an TRPV1 antagonist (Trade name: SymSitiVe l609), for cosmetics and pharmaceutical preparations and developed by the author’s company. This could effectively restrain a series of problems due to excessive activation of TRPV1. Liu Wei, et al. found that, through in vitro and in vivo tests, phenoxyethanol was similar to capsaicin and was the activator of TRPV1. SymSitvie 1609 could significantly restrain excessive activation of TRPV1 caused therefrom.[17]
Inflammation restraining ingredient
The multichannel, anti-inflammatory product (Trade name: DEMUM? KSymrelief?100), developed by the author’s company, using patented technology. Bisabolol was compounded with ginger root extract, therefore the product had the effect of restraining interleukin-1 (lL-l), prostaglandin (PEG2), leucotriene (LTB4), tumor necrosis factor (TNF-α), cyclooxygenase (COX-2) and other inflammation factors. During the test of handling erythema with SDS, 20 volunteers, to whom placebo and active ingredients were applied, were subjected to SDS treatment; and the erythema conditions after 1 day, 3 days, 5 days and 7 days were recorded, respectively. The experimental result showed that the recovery condition of erythema with the active ingredient containing DEMUN,was obviously better than the recovery condition of the group to which the placebo; the bisabolol and ginger root extract had significant synergistic interaction.

Conclusions
Various photoaging factors, complicated metabolic pathways, such as excessive expression of mitochondria,free radicals and cell factors or release of histamine,inflammatory injury induced cell factors were subjected to excessive expression and activation of AhR, and thermoreceptors in the membrane receptors, participated in accelerated aging by the sunlight in the path of photobiological response and photochemical effect.Therefore, it is necessary to take corresponding measures,in traditional sun protection measures, namely resisting UVA and UVB, in order to restrain photobiological responses and photochemical effects caused by UVA,UVB, IRA, etc., synergistically, with the help of measures for restraining inflammatory aging, matrix metalloproteinase (MMP), AhR and TRPV1, etc. while reducing damage to skin more comprehensively.
[1] Duput E; Gomez J; Bilodeau D.Beyond UV rediation: a skin under challenge. International Joural of Cosmetic Science 2013, 35(3), 224-232.
[2] Schroeder P; Lademann J; Krutmann J; et al. Infrared rediationinduced matrix metalloproteinase in human skin:Implications for protection.Journal of Investigative Dermatology 2007,128(10), 2491-2497.
[3] Godley B F; Shamsi F A;Liang Fongqi; et al.Blue light induces mitochondrial dna damage and free radical production in epithelial cell. The Journal of Biological Chmistry 2005, 280,21061-21066.
[4] Liu Wei; Dai Caihong;Tian Yan. The Scientific Basis and Application of Ultraviolet Radiation.Beijing: People’s Medical Publishing House 2013, 29.
[5] Fritsche E; Schfer C.Lightening up the UV response by identification of the arylhydrocarbon receptor as a cytoplasmatic target for ultraviolet B radiation. Procedings of the National Academy of Sciences 2007,104,8851-8856.
[6] Zastrow L; Grith N;Klein F;et al. The missing link-lightinduced(280-1, 600 nm) free radical farmation in human skin.Skin Pharmacology and Physiology 2009, 22(1), 31-44.
[7] Liebel F; Kaur S; Ruvolo E;et al. Irradiation of skin with visible light induces reactive oxygen species and matrix-degrading enzymes. Journal Investigative Dermatology 2012, 32(7),1901-1907.
[8] Mahmoud B H;Hexsel C L;Hamzavi I H;et al. Effects of visible light on the skin.Photochemistry and Photobiology 2008, 84,450-462.
[9] Cho S;Lee M J;Kim M S;et al. Infrared plus visible light and heat from natural sunlight participate in the expression of MMPsand type Ⅰprocollagen as well as infiltration of inflammatory cell in human skin in vivo. Journal of Dermatological Science 2008,50, 123-133.
[10] Cadet J;Berger M; Douki T;et al.Effects of UV nad visible radiation on DNAfinal base damage. Biologival Chemistry 1997, 378, 1275-1286.
[11] Kielbassa C;Roza L;Epe B.Wavelength dependence of oxidative DNA damage induced by UV and visible light.Carcinogenesis 1997,18,811-816.
[12] Mahmoud B H; Ruvolo E;Hexsel C L;et al. Impact of longwavelenth UVA and visible light on melanocompetent skin.Journal of Investigative Dermatology 2010, 130, 2092-2097.
[13] Verallo-Rowell V M; Pua J M;Bautista D.Visible light photopatch testing of common photocontactants in female filipino adults with and without melasma:a cross-sectional study.Journal of Drugs in Dermatology 2008,7,149-156.
[14] Duteil L;Cardot-Leccia N;Queille-Roussel C;et al. Differences in visible light-induced pigmentation according to wavelengths:a clinical and histological study in comparison with UVB exposure. Pigment Cell & Melanoma Research 2014,27(5),822-826.
[15] Mahendran S; Badami S; Ravi S; et al. Synthesis and evaluation of analgesic and anti-inflammatory activities of most active free radical scavenging derivatives of mangiferin. British Journal of Applied Science& Technology 2014, 35 (4), 4959-4973.
[16] Schroeder P; Haendeler J; Krutamnn J. The role of near infrared radiation in photoaging of the skin. Experimental Gerontology 2008, 43(7), 629-632.
[17] Guangl D;Yang D H;Liu Wei;et al.Ingibition of TRPV1 prevented skin irritancy induced by phenoxyethanol.A preliminaty in vitro and in vivo study. International Journal of Cosmetic Science 2017, 39(1),11-16.
 China Detergent & Cosmetics2017年3期
China Detergent & Cosmetics2017年3期
- China Detergent & Cosmetics的其它文章
- Surface Performance Testing of Cardanol Polyoxyethylene Ether and Its Application in Detergent
- Application of New Polymeric Additive in Detergent for Automatic Dishwasher
- Study of a Whitening and Anti-wrinkle Bio-functional Ingredient Based on Epigenetics
- Review of Cosmetic Regulations and the Spot Check in China 2016
- China National Standard
——Alycosides (GBl/kT 1y9l4p64o-20l1y4g) - Technology Development and Market Trends of Laundry Detergent Sheets
