Arachnoiditis Ossificans of Lumbosacral Spine: a Case Report and Literature Review
Liang Wang and Yi-peng Wang
Department of Orthopedic Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
ARACHNOIDITIS ossificans (AO) is a rare type of chronic arachnoiditis characterized by the presence of calcification in, or ossification of the spinal arachnoid. Small plaques of calcification of the dura mater are frequently observed in radiography or during surgery, which are often asymptomatic and have no apparent clinical significance.1AO and dura calcification should not be confused.
To our knowledge, most AO cases reported are from western or Japanese population and there is rarely a case reported with long-term follow-up to identify the progressive course of this disease. In this article, we report a case of AO in a 63-year-old Chinese man and review the radiographic images during 8-year’s follow-up, with consent obtained from the patient for publication.
CASE DESCRIPTION
A 63-year-old man visited our out-patient clinic in September 2013. He had undergone two surgeries of posterior lumbar canal decompression for L3-L5 in 1997 and 1998 for lumbar spinal stenosis at local hospital. The images of computed tomography (CT) before the first surgery showed the lumbar spinal stenosis (Fig. 1). Before the first surgery, the myelography with oil-based contrast was performed and presented the contrast breakoff. The preoperative severe low back pain and numbness of lower limbs relieved after the last operation in 1998. After remission from symptoms for about 1 year, the patient began to complain of repeated buttock pain, numbness of both lower limbs, and progressive claudication. He received conservative treatments, including bed rest, oral non-steroidal anti-inflammatory drugs and neurotrophic medicine, acupuncture, and physical therapy. However, the symptoms were not relieved apparently. The claudication distance shortened from 1000 m to 200 m progressively.
The CT scan performed in 2005, 2011, and 2013 showed hyperdense calcifications of thecal sac and around the cauda equina and nerve roots in the lumbosacral region L4-S1, which were the typical features of AO (Fig. 2). These CT scan images from 2005 to 2013 showed no obvious difference in the degree of ossified plaques formation. The images of X-ray and magnetic resonance imaging (MRI) at the last follow-up visit in 2013 showed ossification plaque located in the lumbar spinal around the thecal sac (Fig. 3). When he came to our hospital, he was diagnosed as AO and informed in detail the high risk of operation. He declined another surgery, only agreed to receive conservative management including oral non-steroidal anti-inflammatory drugs, acupuncture, and physical therapy.
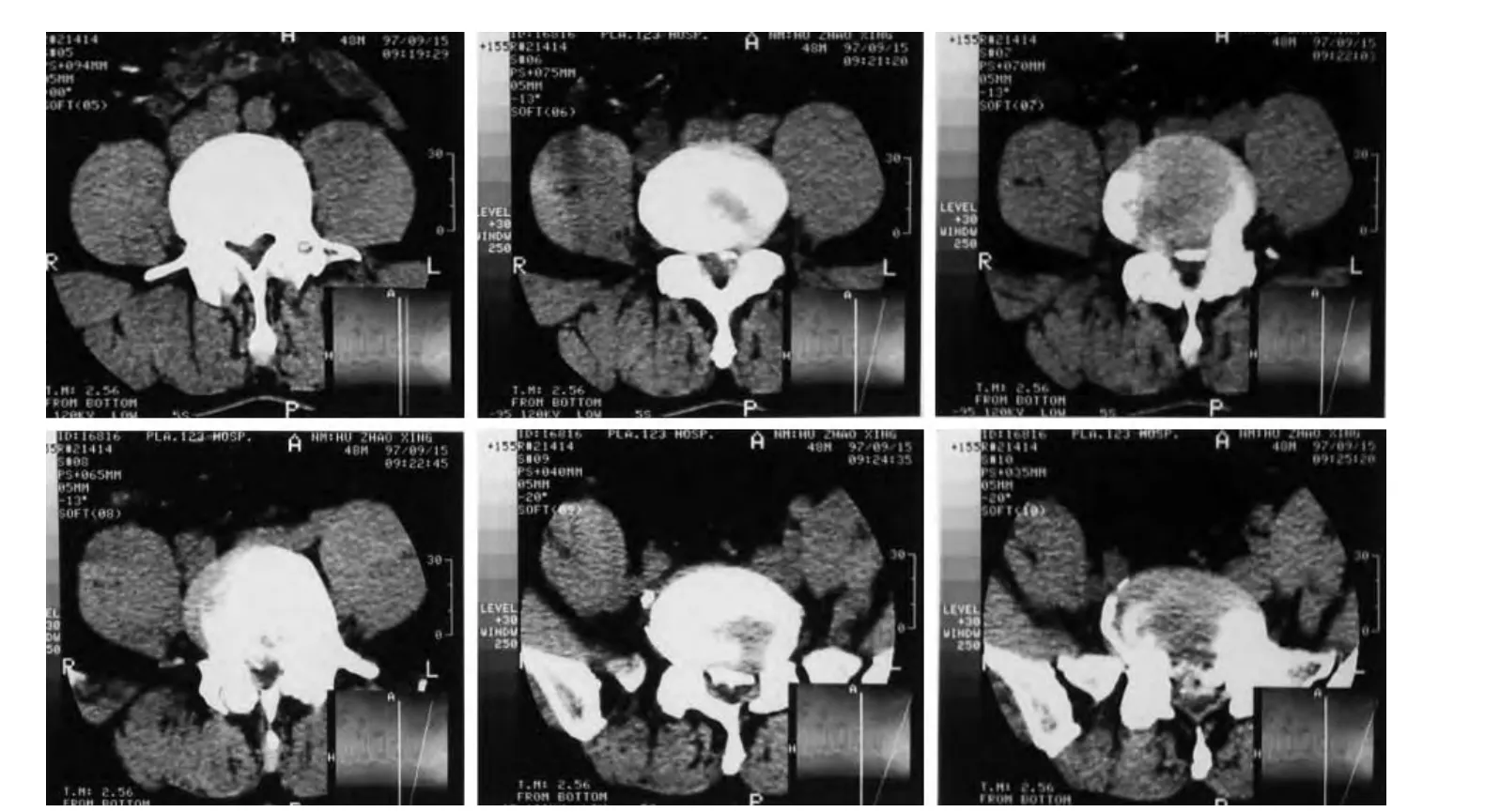
Figure 1. The images of axial CT scan before the first surgery show the lumbar spinal stenosis from L3 to L5.
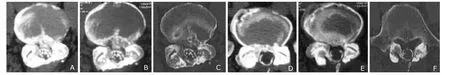
Figure 2. Axial CT scans without contrast show the intradural arachnoiditis ossificans. A. Axial CT scan of L4-L5 segment in 2005; B. Axial CT scan of L4-L5 segment in 2011; C. Axial CT scan of L4-L5 segment in 2013; D. Axial CT scan of L5-S1 segment in 2005; E. Axial CT scan of L5-S1 segment in 2011; F. Axial CT scan of L5-S1 segment in 2013.

Figure 3. The images of X-ray and magnetic resonance imaging at the last follow-up visit in 2013 showed ossification plaque located in the lumbar spinal around the thecal sac.
DISCUSSION
In 1971, the term of “arachnoiditis ossificans” was proposed by Kaufman and Dunsmore2to describe a different and ominous entity that causes a progressive neurological disability with intractable pain, paraparesis, and incontinence due to compression of the spinal cord or spinal nerve roots. AO represents a series of proliferative changes to a patient’s arachnoid and thecal sac, resulting in adhesive intrathecal bony metaplasia. According to the literature, the thoracic spine is involved in 66% of all the AO patients and the lumbar spine in 24%.3
The true incidence of spinal AO is uncertain and this condition tends to occur with increasing frequency with advancing age.2There are a few reports of AO in relation to various disease entities. The co-occurrences of AO with syringomyelia have been reported previously.4,5In addition, Joo et al6reported a case of AO of thoracolumbosacral spine in the advanced ankylosing spondylitis.
The pathogenesis of AO is not yet understood. Multiple factors are responsible for AO, some of which are local, whereas others are general. Prior trauma, surgery, subarachnoid hemorrhage, injection with drugs such as anaesthetic agents and oil-based contrast media for myelography, spinal infection, dural vascular anomalies, tumorous conditions and repeated mechanical insults to the spinal meninges have all been implicated as causative factors of AO.2,7,8The patient in this report had myelography with oil-based contrast and twice lumbar surgeries, both of which are risk factors for AO. His progressive deterioration of neurological deficits in recent years suggested the possible development of AO, but the radiographic findings do not aggravate during 8-year follow-up.
AO is usually associated with progressive neurological deficits. There was no uniform clinical presentation in the patients. This patient’s clinical course of progressive disabling symptom was presumably directly related to involvement of spine or nerve roots in the cauda equina, due to primary compression or secondary to other causes.
Given the unique radiological presentation, diagnosis of AO is typically made based on imaging results. Plain radiographs and MRI may occasionally demonstrate the calcifications but the findings are non-specific and may be misleading. Because the ossification plaques are typically hyperdense on CT scans and can be identified easily against the hypodense thecal sac and nervous tissue, spinal CT scan is the most sensitive imaging modality for the diagnosis of AO and the evaluation of the extent of the lesions. The ossification masses are usually seen surrounding the spinal cord or thecal sac. In the lumbosacral region, they may also be seen intradurally, adjacent to the nerve roots.9,10On the other hand, the hyperdense calcification or ossification may be mistaken for contrast solution if intra-thecal contrast was administered in a myelography.
The prognosis of AO is variable. Some patients may have progressive compressive myelopathy, but some patients remain stable with only mild symptoms. An exact time course for disease progression has not been established due to the rarity of this condition and the fact that it is not typically identified until later stages.11The optimal treatment strategy for AO has not been established. Non-operative measures are often recommended due to the high risk of neurological sequela and reossification.4The surgical option often presents a clinical dilemma, since surgery itself is a known causative factor of AO and may worsen neurological deficits. It is therefore recommended that surgery is only reserved for cases with progressive neurological deterioration. Surgical procedures, including laminectomy, foraminectomy, or plaque excision, are performed mainly to decompress the spinal cord and improve blood and cerebrospinal fluid flow.10
1. Knoblich R, Olsen BS. Calcified and ossified plaques of the spinal arachnoid membranes. J Neurosurg 1966; 25:275-9.
2. Kaufman AB, Dunsmore RH. Clinicopathological considerations in spinal meningeal calcification and ossification. Neurology 1971; 21:1243-8.
3. Kitagawa H, Kanamori M, Tatezaki S, et al. Multiple spinal ossified arachnoiditis. A case report. Spine (Phila Pa 1976) 1990; 15:1236-8.
4. Domenicucci M, Ramieri A, Passacantilli E, et al. Spinal arachnoiditis ossificans: report of three cases. Neurosurgery 2004; 55:985.
5. Papavlasopoulos F, Stranjalis G, Kouyialis AT, et al. Arachnoiditis ossificans with progressive syringomyelia and spinal arachnoid cyst. J Clin Neurosci 2007; 14:572-6. 6. Joo KB, Lee S, Kang CN, et al. Arachnoid ossificans of thoracolumbosacral spine in the advanced ankylosing spondylitis: a case report. Rheumatol Int 2013; 33:1623-5.
7. Bakhsh WR, Mesfin A, Bridwell KH. Arachnoiditis ossificans after revision adolescent idiopathic scoliosis surgery: a 22-year follow-up and review. Spine (Phila Pa 1976) 2013; 38:E1166-70.
8. Bell RB, Wallace CJ, Swanson HA, et al. Ossification of the lumbosacral dura and arachnoid following spinal cord trauma. Case report. Paraplegia 1995; 33:543-6.
9. El Asri AC, El Mostarchid B, Akhaddar A, et al. Arachnoiditis ossificans of the cauda equina. Br J Neurosurg 2012; 26:547-8.
10. Jaspan T, Preston BJ, Mulholland RC, et al. The CT appearances of arachnoiditis ossificans. Spine (Phila Pa 1976) 1990; 15:148-51.
11. Ng P, Lorentz I, Soo YS. Arachnoiditis ossificans of the cauda equina demonstrated on computed tomography scanogram. A case report. Spine (Phila Pa 1976) 1996; 21:2504-7.
 Chinese Medical Sciences Journal2014年2期
Chinese Medical Sciences Journal2014年2期
- Chinese Medical Sciences Journal的其它文章
- Serum Levels of Interleukin-1 Beta, Interleukin-6 and Melatonin over Summer and Winter in Kidney Deficiency Syndrome in Bizheng Rats△
- Minimally Invasive Perventricular Device Closure of Ventricular Septal Defect: a Comparative Study in 80 Patients
- Expression of Peptidylarginine Deiminase 4 and Protein Tyrosine Phosphatase Nonreceptor Type 22 in the Synovium of Collagen-Induced Arthritis Rats△
- Lipocalin-2 Test in Distinguishing Acute Lung Injury Cases from Septic Mice Without Acute Lung Injury△
- False Human Immunodeficiency Virus Test Results Associated with Rheumatoid Factors in Rheumatoid Arthritis△
- Ketamine Abuse-Induced Obstructive Nephropathy and Kidney Injury
