Application of optical coherence tomography in diagnosis of thrombosis secondary to in-stent plaque rupture after bare metal stent implantation in one case
Case presentation
A 67 years old female patient, complaining of"paroxysmal chest pain for more than half month",was admitted to Second Affiliated Hospital of Harbin Medical University on April 14, 2010. Half month ago,the patient suffered paroxysmal precordial squeezing pain with unclear incentive. The pain radiated outwards the shoulders and lasted for 5 minutes, which was relieved by taking nitroglycerin. The patient had been treated with antiplatelet, anticoagulant and lipid-lowering, but the symptom still attacked intermittently. The patient was admitted to our hospital for further diagnosis and treatment.
Past medical history: The patient had a 7-year history of hypertension with the highest blood pressure at 200/120mmHg, and the systolic pressure and diastolic pressure were controlled within range from 120mmHg to 130mmHg and 90mmHg to 95 mmHg respectively by taking oral Nifedipine Controlled-Release Tablets. The patient also had a 7-year history of hyperlipidemia and took oral atorvastatin calcium tablets daily, but the plasma lipid level did not meet the target level. The patient has undergone percutaneous coronary intervention (PCI) twice. A bare-metal stent (BMS) was implanted in the middle of right coronary artery (RCA) seven years ago, and a drug-eluting stent (DES) in the distal portion of RCA six months ago. She denied a history of diabetes.
Physical examination: Body temperature was 36.7℃, pulse rate 62 beats/min, respiratory rate 18 times/min, and blood pressure 160/100 mmHg. The patient had clear consciousness. On chest auscultation,pulmonary sounds were clear and symmetrical, neither dry nor moist rale was heard. Her cardiac rhythm was regular at 62 beats/min. No pathological murmur was heard in each valve area. Physical examination revealed soft abdomen, no tenderness or rebound tenderness. Liver and spleen were not enlarged. The patient presented with no edema on lower limbs.
Examination after admission: The plasma lipid level test: TG5.43 mmol/L, TC3.97 mmol/L, HDL-C 1.45 mmol/L, LDL-C 3.92 mmol/L; fasting serum glucose 7.32 mmol/L; 2h postprandial plasma glucose 13.8mmol/L; glycosylated hemoglobin 6.9%; hs-CRP 11.3 mg/L; electrocardiogram showed ST-segment depression in leadsⅡ,Ⅲ,avF.
Treatment: On the second day after admission,the patient successfully underwent coronary angiography (CAG) and PCI. The CAG showed 60%stenosis in the proximal of the left descending artery(LAD), 80% stenosis in the ostium of the first diagonal branch, 30% stenosis in the proximal of the left circumflex coronary artery (LCX), 80% stenosis in the BMS located in the middle of RCA, and no stenosis in the DES. Optical coherence tomography(OCT) revealed ruptured lipid-rich plaque and thrombosis inside BMS(Figure 1). One DES was successfully implanted in the BMS which was located in the middle of RCA,and then the symptom disappeared. The patient is currently in the follow-up with stable postoperative condition.
Clinicopathologic discussions
Dr. MENG Lingbo:This patient was admitted to our hospital due to “paroxysmal chest pain for more than half month”. Half month ago, the patient began to suffer chest pain for unknown cause, which was considered as unstable angina pectoris. The patient had undergone PCI twice, and had a history of hyperlipidemia. In addition,diabetes mellitus was diagnosed when the patient was hospitalized this time. So we considered the chest pain might be caused by plaque rupture and secondary thrombosis, restenosis in stent, thrombosis in stent, coronary spasm and so on. The patient had been treated with antiplatelet therapy, anticoagulant therapy and lipid-lowering therapy before she was admitted to our hospital, but the symptom was not obviously relieved. So CAG should be performed as early as possible to definite the causes, which could assist us to choose the correct management.
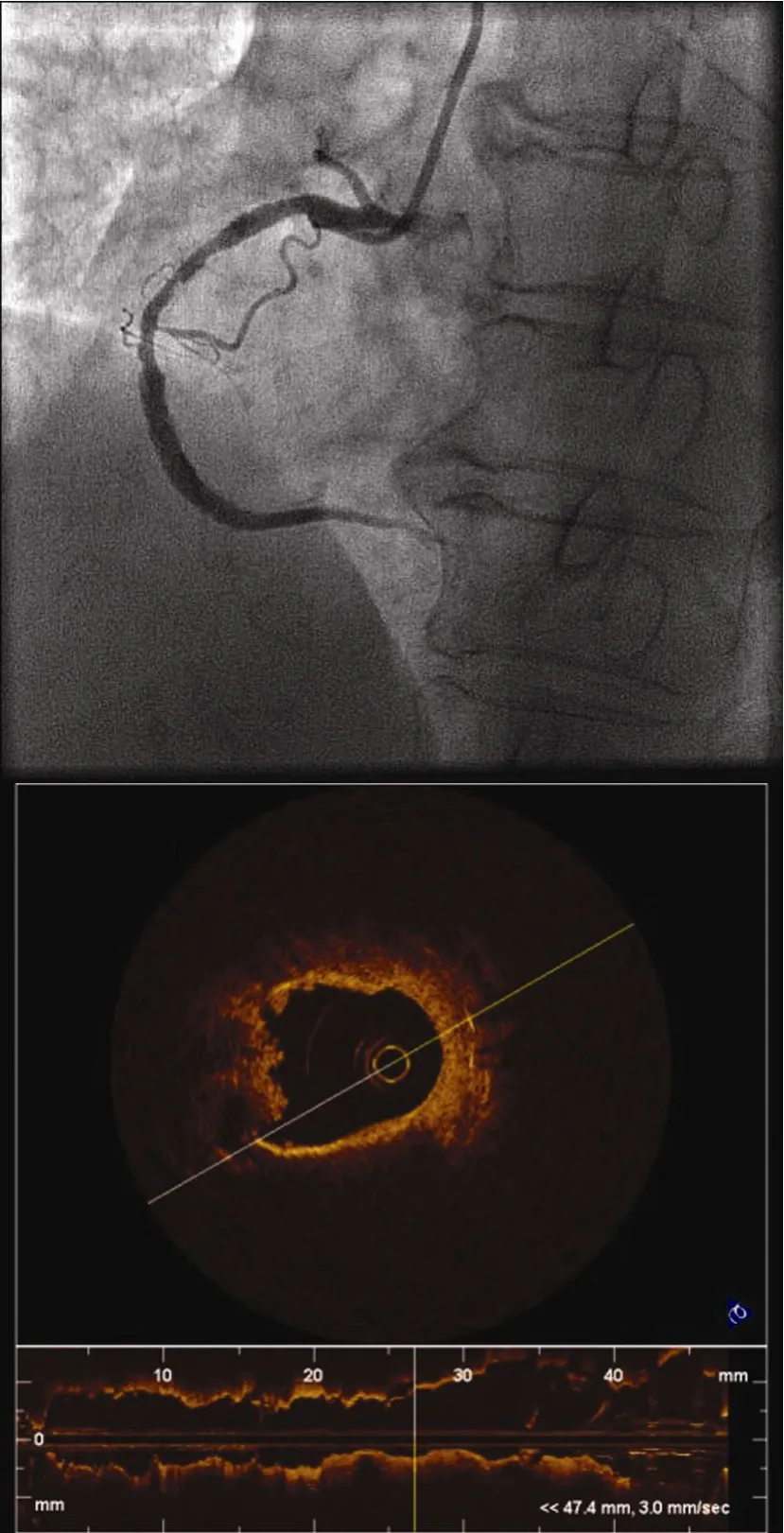
Figure 1 Ruptured lipid-rich plaque and thrombosis inside bare-metal stent revealed by optical coherence tomography
Dr. HAN Zhigang:The patient’s CAG indicated 60% stenosis in the proximal of LAD, 80% stenosis in the ostium of the first diagonal branch, 30% stenosis in the proximal of LCX, 80% stenosis in the BMS which was located in the middle of RCA, and no stenosis in the DES which was located in the distal of RCA. Restenosis,which was considered as unstable lesion through the CAG image, was found in the stent located in the middle of RCA. Moreover, electrocardiogram showed ST-segment depression in leadsⅡ,Ⅲ, avF. All of these were consistent with the clinical symptoms. But the resolution of CAG is not high enough to well reflect the characteristics of the culprit lesion. Moreover, the CAG image cannot identify the detailed characters of the lesion inside the stent. On the basis of clinical features and CAG images mentioned above, we considered there may be neointimal hyperplasia or thrombosis which induced the formation of restenosis in stent. So we need other instruments with higher resolution to identify the culprit lesion inside the stent.
Dr. YANG Shuang:To identify the features of the lesion in stent located in the middle of RCA and to choose the best treatment, we could use intravascular ultrasound (IVUS) or OCT to accomplish it. Both IVUS and OCT are intracoronary imaging techniques with high resolution, which can reveal the feature of the lesion.IVUS, the current clinical technology with the high resolution and penetrating power, has a maximum axial resolution of 100 μm. IVUS can be used to measure plaque burden and positive or negative vascular remodeling, assess the left main stem lesion and evaluate perivascular injury (hematoma or perforation). OCT is a non-contact, light-based imaging modality utilizing newly developed fiber-optic technologies. OCT has higher resolution and faster scanning speed than IVUS.Comparing with IVUS, OCT is superior in defining the plaque and thrombus, evaluating the immediate vascular response to stent implantation, and evaluating the character of neointimal. CAG findings showed in-stent restenosis in middle of RCA, which was considered as neointimal hyperplasia or thrombosis. Moreover, because the diameter of IVUS catheter is bigger, the lesion in the stent could be injured when IVUS catheter passes it. So we tended to prefer OCT for this patient. OCT image acquisition was performed using a commercially available system for intracoronary imaging and a 0.019-inch ImageWire. To acquire the accurate images, we should avoid to injury the lesion when the wire passes the lesion,and use the balloon to interrupt blood at the proximal of the stent.
Dr. HOU Jingbo:There was 80% stenosis in the stent located in middle of RCA, and OCT imaging showed ruptured lipid-rich plaque and thrombosis inside the stent. Although the patient had received antiplatelet therapy, anticoagulant therapy and lipid-lowing therapy,the symptom did not disappear. We decided to implant one stent (Cypher) in the BMS. OCT imaging showed complete stent apposition after procedure(Figure 2). The patient undergoing antithrombotic treatment after PCI should strictly control the level of blood pressure as well as blood glucose. To a large extent, the formation of in-stent restenosis is related to the poor lipid control, so we should apply intensive statin therapy to the patient.According to the ATP III guidelines, the target of low-density lipoprotein cholesterol (LDL-C) (<700mg/L)is a therapeutic option for certain patients at very high risk. The lower the level of LDL-C is, the greater the potential gain in terms of disease treatment will be. Intensive statin therapy showed beneficial effects in patients treated with PCI or coronary artery bypass grafting(CABG). Statins play an important role in delaying atherosclerosis, reducing adverse coronary events, and lowing cardiovascular mortality and morbidity in patients with CVD. When the high-risk patient has high triglycerides, fibrates drug can be taken into consideration for controlling the balance of diet and sugar. On the other hand, the atherosclerotic process may gradually progress because the patient has more risk factors. So it will be very important to have regular follow-up of this patient besides pharmacotherapy, so as to observe development of coronary lesion and adjust medication, and eventually all of this will be beneficial to avoid the occurrence of major adverse cardiac events.
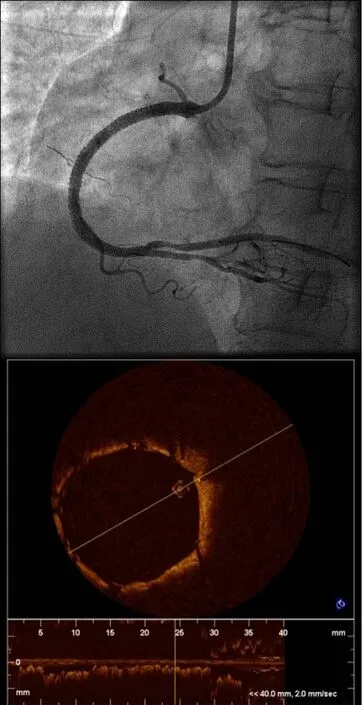
Figure 2 Optical coherence tomographic imaging shows complete stent apposition post procedure
Dr. YU Bo:OCT findings revealed lipid-laden atherosclerotic plaque formed inside BMS located in middle of RCA, and ruptured plaque with thrombosis. So we speculated that the clinical symptoms can be attributed to disruption of thin-cap fibroatheroma and secondary very late stent thrombosis. Finally, the patient presented unstable angina pectoris. Following the development of intracoronary imaging technology and the extension of follow-up time after PCI, the reports about in-stent lipid plaque are increasing. Atherosclerosis of the neointima within the stent was defined as peristrut foamy macrophage clusters with or without calcification,fibroatheromas, thin-cap fibroatheromas, and ruptures with thrombosis. In all cases, there was no communication of the lesion within the stent with the underlying native atherosclerotic plaque. Although the underlying processes responsible for the development of neoatherosclerosis after stent implantation have not yet been fully elucidated, it may be due to the inability to maintain a fully functional endothelialized luminal surface within the stented segment, and the deposition of lipid into neointimal which leads to the formation of plaque within the stent finally. In our previous study, we applied OCT imaging in 39 patients with 60 BMS who developed recurrent ischemia. Lesion that had features of lipid-rich plaque (LRP) was found in 20 stents in 16 patients, and one patient had ruptured plaque with thrombosis within the stent. Seven restenotic lesions with LRP were responsible for unstable angina symptoms. Moreover, we found that the development of LRP inside the BMS was after about 6 years of stenting. Nakazawaet alhave reported that 197 BMS from 147 autopsy cases with implant duration >30 days were examined for the presence of neointimal atherosclerotic disease. The neoatherosclerosis inside the BMS was found in 31 lesions, and 10 lesions displayed vulnerable plaques, and the BMS duration with neoatherosclerosis exceeded six years. The results of above clinical observation and autopsy indicate that the BMS duration with lipid plaques usually exceeds six years. The plaque within the BMS can induce restenosis and late or very late stent thrombosis, which can lead to adverse outcomes, including unstable angina pectoris, myocardial infarction and sudden death. For this patient, she was implanted with a BMS 7 years ago and failed to efficiently control the lipid and blood glucose level; all above are high risk factors for the formation of in-stent plaque. In our hospital, the patient underwent OCT, and we eventually ensured that the culprit lesion which induced recent clinical syndroms was the neointimal hyperplasia and ruptured plaque with thrombosis.