Surgical Removal of a Giant Vegetation on Permanent Endocavitary Pacemaker Wire and Lead
Guo-tao Ma,Qi Miao*,Chao-ji Zhang,and Li-hua Cao
Department of Cardiovascular Surgery,Peiking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peiking Union Medical College,Beijing 100730,China
PACEMAKER lead infections are rare.There are only about 0.4%-1.1% of the patients who have been implanted permanent pacemakers suffering from serious infections which lead to endocarditis.1Generally,removal of the infected pacemaker wire and lead,long-term anti-infection therapy,and implantation of a new pacemaker to another anatomic site are accepted approaches for these patients.2,3
CASE DESCRIPTION
A 49-year-old man had implanted a permanent pacemaker 3 years ago owing to bradycardia with a heart rate as low as 38 beats per minute (bpm) (Fig.1).He had intermittent fever and backing cough 6 months ago,empirical antibiotic therapy was sometimes effective,but the above symptoms appeared repeatedly.He fainted while queuing up for visiting our clinic and recovered 5 minutes later with profuse sweating.Multiple blood cultures turned out negative.A transthoracic echocardiography revealed a large vegetation (approximately 3.0-4.0 cm) on the right atrium and right ventricular pacemaker lead (Fig.2),which obstructed the tricuspid orifice.
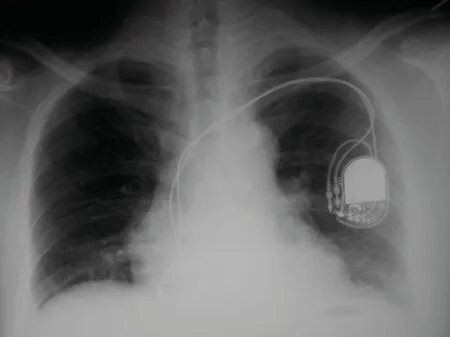
Figure 1.Chest radiograph shows the pacemaker and lead implanted via subclavian vein,innominate vein,and superior vena cava into the right atrium and ventricle.
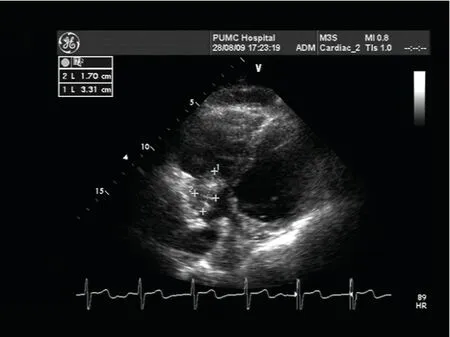
Figure 2.Transthoracic echocardiographic image shows a large vegetation in the right atrium.
Based on the blood cultures results,we gave empirical antibiotic therapy with vancomycin [1000 mg intravenously guttae (ivgtt) once per 12 hours],but he still had a fever and dry cough.Then we replaced vancomycin with tazocin (4.5 g ivgtt once per 8 hours) and his temperature decreased to normal level.Considering the size of the vegetation and all the symptoms,we were afraid of pulmonary embolism or obstructed tricuspid orifice leading to a faint again,thus decided to surgically remove the pacemaker wire and lead as well as the vegetation.Because the patient’s heart rate was about 90 bpm and the cardiac rhythm was sinus rhythm before operation,Holter monitoring was performed and the physician determined that he did not need to implant pacemaker again.
Cardiopulmonary bypass (CPB) was adopted for the operation.During the operation,we found two pacemaker wires and leads entering from superior vena cava (SVC)into the right atrium.One was adherent to the right auricle,the other to septal leaflet of the tricuspid valve and then extended to the right ventricular septum.Both wires and leads were enwrapped by the vegetation and the septal cuspa of tricuspid valve was involved (Fig.3).The site where the SVC connected with the right atrium was found stenosis because of the local inflammation,edema,and fibroplasia.The lead and the vegetation were cleaned off.Due to the firm adherence to the septal leaflet and its chordae,the septal leaflet and adhesive structures were dissected too.A piece of pericardium was used to replace septal leaflet to patch tricuspid valve.Under deep hypothermic CPB,superior caval cannule was clamped and removed.Pump flow was decreased and CPB continued with single venous cannule.The right atrial incision was extended to SVC,through which we found the vegetation extended to SVC,which prolonged about 1 cm above the entry of the SVC.The vegetation in SVC was cleaned off and the wire was cut off.Both the pacemaker and the proximal tip of the wire and lead were pulled off from the subcutaneous site.A piece of pericardium was used to patch and expand the entry of the SVC (the diameter enlarged to 1.5 cm).SVC was cannulated again.Right atrium was closed.
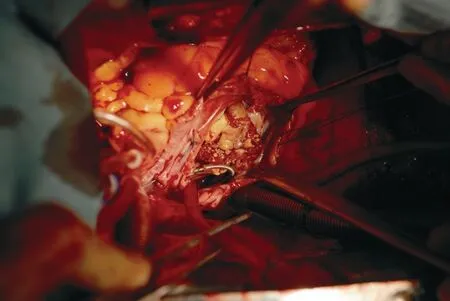
Figure 3.A photo demonstrates the pacemaker lead with giant vegetation in the right atrium during the operation.
After perfusion rewarming,aorta declamping,and heart resuscitation,electrocardiography showed nodal rhythm,and the heart rate was about 50 bpm.A temporary pacemaker was applied to maintain the heart rate at 80 bpm.A unipolar pacing lead was implanted on to the lateral wall of the left ventricular surface.The proximal tip of the lead went through left anterior chest wall and was buried subcutaneously.
After the operation,the patient was transferred to the Intensive Care Unit (ICU).His heart rhythm recovered to sinus rhythm within postoperative 72 hours.The heart rate was about 86 bpm,so the temporary pacemaker was removed.He stayed in ICU for 4 days,then returned to the general ward.Drainage tubes were removed on the 5th postoperative day.The patient had a normal temperature after the operation.Antibiotic therapy consisting of vancomycin (1000 mg ivgtt once per 12 hours) and tazocin(4.5 g ivgtt once per 6 hours) was continued for 1 week.Then a low fever began and dry cough reoccurred.In 2 weeks after operation,the vegetation culture was positive for Scopulariopsis sp,and pathological result revealed fungus infection.The drug sensitivity result was voriconazole,so vancomycin was replaced with voriconazole.Three days after the replacement,the patient’s temperature declined to normal but the cough was dot relieved.The consulted otorhinolaryngologist considered that the patient had got respiratory allergy and advised him to take chlorpheniramine.The cough relieved remarkably.Voriconazole was administered for 6 months.The patient was discharged on 21st postoperative day,and follow-up visits in the 5th and 9th week,the 6th and 12th month revealed no signs of recurrent infection.The sinus rhythm was well maintained.
DISCUSSION
Pacemaker-related endocarditis is a rare condition,but has a high risk of mortality if left untreated.The most common pathogenic bacteria are Staphylococcus aureus and Staphylococcus epidermidis.But in the present case,the pathogenic bacteria is Scopulariopsis sp,a very rare type of fungus.Fortunately,it is sensitive to voriconazole.The reason of Scopulariopsis sp infection in this case is unknown.The patient is a healthy man otherwise and has no bad habits or diabetes mellitus,which is considered a risk factor of pacemaker-related endocarditis.4Before the infection,he had to work hard for months,and felt very tired.It was possible that he was infected by a common bacterium at first,got a long-term antibiotic therapy,and was infected by Scopulariopsis sp finally.
The symptoms of pacemaker-associated endocarditis are mostly subacute or chronic,which will delay the proper diagnosis.In general,fever is the most frequent and dominant symptom.The period from the onset of fever to the diagnosis of endocarditis may be as long as 3 to 4 months.5,6In the present case,the delay period was 6 months,which may be caused by the lack of awareness of endocarditis on the part of local hospital.Echocardiography examination is very important in diagnosing endocarditis,able to provide prognostic information,evaluate the risk of embolization and the need of cardiac surgery.7Conservative medical therapy often fails in that type of endocarditis.8Total removal of the pacemaker system should be preferred in pacemaker-associated endocarditis.Because extraction of the infected parts alone may lead to recurrent infection,and the percutaneous method has potential risks such as rupture in the tricuspid valve,right ventricular perforation,and vegetation peeling,which may lead to pulmonary embolism,especially when the size of the vegetation is more than 10 mm,the risk of pulmonary embolism is higher than surgical method.9Surgical extraction of the lead using CPB is a safe approach.10This method eliminates the risk of mechanic injury to the tricuspid valve and right ventricle,and prevents embolization of the lungs.In this case,if the lead was extracted by percutaneous method,the patient’s heart would be damaged badly and might lead to death directly because of pulmonary embolism.Therefore,simple percutaneous extraction has to be avoided especially when the tip of the lead carries vegetation.CPB is a safe procedure without major complications.On the other hand,without performing the operation,we might never identify the pathogen of the infection.Thus complete removal of infected pacemaker lead should be a part of the standard therapy.Certainly,long-term antibiotic therapy is essential in the preoperative period and should be continued to the postoperative period,especially for the fungal infections.
1.Erdinler I,Omken E,Zor U,et al.Pacemaker-related endocarditis:analysis of seven cases.Jpn Heart J 2002;43:475-85.
2.Gilligan DM,Dan D.Excimer laser for pacemaker and defibrillator lead extraction:techniques and clinical results.Laser Med Sci 2001;16:113-21.
3.Massoure PL,Reuter S,Lafitte S,et al.Pacemaker endocarditis:clinical features and management of 60 consecutive cases.Pacing Clin Electrophysiol 2007;30:12-9.
4.Arber N,Pras E,Copperman Y,et al.Pacemaker endocarditis.Report of 44 cases and review of the literature.Medicine (Baltimore) 1994;73:299-305.
5.Cacoub P,Leprince P,Nataf P,et al.Pacemaker infective endocarditis.Am J Cardiol 1998;82:480-4.
6.Villamil Cajoto I,Rodríguez Framil M,Van den Eynde Collado A,et al.Permanent transvenous pacemaker infections:an analysis of 59 cases.Eur J Intern Med 2007;18:484-8.
7.Jassal DS,Weyman AE.Infective endocarditis in the era of intracardiac devices:an echocardiographic perspective.Rev Cardiovasc Med 2006;7:119-29.
8.Karchmer AW,Longworth DL.Infections of intracardiac devices.Cardiol Clin 2003;21:253-71.
9.Klug D,Lacroix D,Savoye C,et al.Systemic infection related to endocarditis on pacemaker leads:clinical presentation and management.Circulation 1997;95:2098-107.
10.Ruttmann E,Hangler HB,Kilo J,et al.Transvenous pacemaker lead removal is safe and effective even in large vegetations:an analysis of 53 cases of pacemaker lead endocarditis.Pacing Clin Electrophysiol 2006;29:231-6.
 Chinese Medical Sciences Journal2011年4期
Chinese Medical Sciences Journal2011年4期
- Chinese Medical Sciences Journal的其它文章
- Efficacy of Surgical Therapy for Carotid Body Tumors
- Neurological Manifestations of Takayasu Arteritis
- Efficacy and Safety of Low Molecular Weight Heparin Prophylaxis for Venous Thromboembolism Following Lumbar Decompression Surgery
- Contrary Regulation of TIMP-1 and MMP-9 by Hepatocyte Growth Factor Antibody after Lung Injury
- Atypical Chronic Myeloid Leukaemia with Trisomy 13:a Case Report
- Open Partial Nephrectomy in Solitary Kidney with Multiple Renal Cell Carcinoma:a Case Report
