Efficacy of Surgical Therapy for Carotid Body Tumors
Li-shan Lian,Chang-wei Liu,Heng Guan,Yue-hong Zheng,Xing-ming Chen,and Yong-jun Li*
Department of Vascular Surgery,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
THE carotid body tumor is a rare clinical chemical receptoma.Carotid body origins from the neural crest ectoderm and mesoderm of the organization,the so-called nerve nodule.Carotid body tumor accounts for 0.22% of head and neck cancers,1and has an incidence rate of about 0.012% in general population.2The carotid body tumor locates at the branch of the common carotid artery,where many important nerves approach to it.Because of its unique anatomical position,the disease has imposed great difficulties for surgeons,and brought a considerable incidence of postoperative complications following surgical therapy.The present study analyzes the diagnosis,surgical treatment,and postoperative complications in patients with carotid body tumors to evaluation the efficacy of surgical therapy for this condition.
PATIENTS AND METHODS
Patients with carotid body tumors in Peking Union Medical College Hospital from 1949 to May,2011 were included in the present study.All preoperative diagnosis was confirmed with ultrasound,computed tomography angiography (CTA),or magnetic resonance angiography examination.A total of 48 cases had preoperative digital subtraction angiography (DSA) test.According to Shamblin classification,3the tumors were categorized into type I,II,and III.In pathological test,malignant behavior showed as local lymph node metastasis,ipsilateral recurrence,remote metastasis (including bone and pancreas),and ipsilateral carotid artery occlusion.In cases with evidence of malignancy,careful follow-up was advised by pathologists.The records were reviewed regarding demographic data,clinical manifestations,diagnosis,surgical procedure,postoperative pathological result,and follow-up findings.
RESULTS
General information
A total of 120 cases of carotid body tumors were enrolled,including 46 males and 74 females (male∶female=1∶1.61).The mean age of the patients was 39.2±3.1 years(range,18-68 years).Nineteen cases lived in high altitude area such as Inner Mongolia and Qinghai.
Most of the patients were asymptomatic and tumors were found unintentionally during daily life or medical examination.However,18 patients had different symptoms when a carotid body tumor was found,including:oppressive pain in 8 cases,dizziness and headache in 10 cases,tinnitus in 2 cases,tongue skewed in 3 cases,hoarseness in 2 cases,transient amaurosis in 1 case,transient ischemia attack in 1 case,and obstructive sleep apnea syndrome in 1 case.
The course of disease varied from 3 months to 35 years.There were 104 unilateral tumors and 16 bilateral ones.For bilateral body tumors,2 patients were hereditary,and one proband’s aunt also had bilateral carotid body tumors.The largest size of tumor was up to 10 cm×9 cm×8 cm,and the minimum size was 2 cm×1.5 cm×1.5 cm.In all the 120 patients,29 cases had type I tumor,40 had type II tumor,and 51 had type III tumor.
Postoperative pathological test had been done in all the operative cases.Eight cases were diagnosed as malignant paraganglioma by pathology and biological behavior.Another 10 cases showed pathological active growth (8.3%)which needed careful follow-up.
Surgical information
One hundred and eleven patients were operated under general anesthesia with sternocleidomastoid incision.The surgical excision rate was 92.5%,with 9 cases did not take operation.In the 9 cases,4 cases took puncture examination,and 2 cases received the neck mass exploratory biopsy,histologically confirming carotid artery body tumor.However,due to high risk (very large size,location extending to the bottom of the skull or carotid artery invasion),the tumors were left without totally excised.
Of the 111 patients undergoing surgical excision,50 had simple tumor excision,42 had resection of tumor body and ligation of the external carotid artery,12 had vascular reconstruction of the carotid artery (6 with saphenous vein,5 with artificial grafts,and 1 with jugular vein),7 cases underwent co-resection of tumor body and common carotid artery,internal carotid artery as well as external artery,without vessel reconstruction.For some difficult cases,such as when the tumors extended to the bottom of the skull,the surgery was completed with accompany of otorhinolargyngologists.Complete resection of the tumors was preformed by releasing the mandibular joint,and even removing the mastoid to fully reveal the blood vessels and nerves in the bottom of the skull.
One patient had a mediastinal tumor accompanied by hypertension,and the highest blood pressure was 240/120 mmHg.After resection of the mediastinal tumor,the blood pressure returned to normal,and the tumor was diagnosed as pheochromocytoma.Then the left carotid body tumor was excised.The patient had a good recovery with a normal blood pressure.
The 16 cases with bilateral carotid body tumor had the tumors totally resected with twice operation.
Several methods were adopted to improve the brain tolerance to the temporary or permanent carotid artery obstruction,for example,the Matas training,which was pressing the common carotid artery and gradually increased the pressing time.The training was started one or two weeks before surgery.In this study,the longest time of Mastas test was 35 minutes,the shortest time was 3 minutes,which meant the patient could not endure.For those patients whose tolerant time was less than 10 minutes,temporary balloon occlusion (TBO) was further conducted to evaluate the Willis cycle and inner-carnal collateral circulation.If the evidence of poor collateral circulation evidence was found,carotid artery reconstruction and shunt was emphasized to avoid stoke.During the operation,4 cases received the shunt management because of severe carotid artery stenosis.
Outcomes
No operative mortality happened in those 111 cases receiving operation.Postoperative complications rate was 29.7% (33/111),showed as:stroke in 3 cases,Horner’s syndrome in 5 cases,vagus damage in 10 cases,andhypoglossal nerve damage in 15 cases (Table 1).In the 3 patients who developed cerebral infarction,2 were due to carotid artery ligation as well as the huge tumor,and 1 suffered sinus reflex vagal with heart beat down to 48 beats per minute and hypotension.
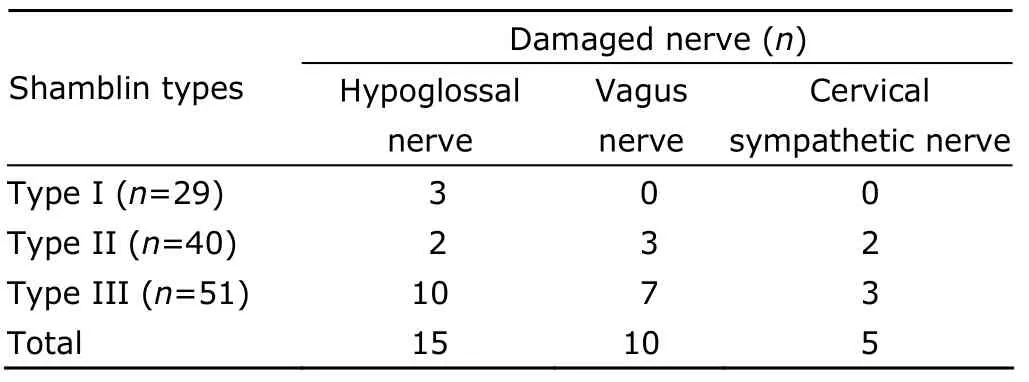
Table 1.Cranial nerve injury information
Follow-up result
All the patients were followed up through mails or telephones.The average follow-up time was 8.46±1.1 years.According to follow-up records,only 1 case of cerebral infarction was getting gradual recovery with muscle power improving from 0 to 2 grade,and partial recovery with talking function.In all the eight malignant carotid body tumor patients,recurrence was observed in 6 cases,with distant metastasis of bone,pancreas,followed by death.The other 2 cases of malignant tumor showed no evidence of recurrence,but had residual cranial nerve damage during follow-up period.The recurrence rate of malignant tumor was calculated as 75% (6/8) and most resulting in death.On the other hand,in the benign patients,the recurrence rate was 1.9% (2/103).One was due to the large size of the tumor and partial resection in the first operation.The other was histologically active.Moreover,they all had local recurrence.After re-operation,and total removal of the residual tumor,the patients remained in good condition in follow-up.In the 9 cases having no surgery for carotid body tumor,8 patients were Shamblin type III,1 was type II,and 2 had bilateral tumors.All their tumors were found more than 5 years ago when they visited our hospital.During the follow-up,the tumors grew and induced nerve injury.CTA showed carotid artery involvement and severe stenosis or occlusion.The patients presented with hoarse voice,dizziness,memory lost,and cerebral infarction.One patient died due to tumor-induced carotid artery ischemic stroke.
DISCUSSION
The etiology of carotid body tumor is not clear.Chronic hypoxia,succinodehydrogenase mutations,and long-period of living at high altitudes are considered relevant with tumor etiology.4However,in this study,only 1 case was associated with sleep apnea syndrome,and 19 lived in high altitudes.The percentage is 15.8%,far from enough to account for the majority of the patients,indicating that chronic hypoxia may only be part of the cause,and further research should be performed on the tumorgenesis.
Because of the unspecific symptoms,carotid body tumor is often misdiagnosed.It not only increases the diagnostic process,but also creates obstacles for further surgery.Ultrasonography,a non-invasive inspection,can clearly show the size and shape of the tumor,and its relationship with peripheral vessels.5Thus ultrasonography could serve as a preferred method for carotid body tumor.Although DSA is still thought as the gold standard of carotid body tumor diagnosis,CTA has recently become the first-line technology and is replacing DSA.CTA can display the tumor size,neck arteries situation,and carotid arteries erosion.Furthermore,CTA can evaluate cranial collateral circulation and provide more detailed information for surgery treatment.6
Most of the carotid body tumors are biologically benign and grow slowly.However,literature data indicate that surgery remains the preferred treatment for carotid body tumor.7That is due to the special anatomical location of the tumor,i.e.adjacent to important cranial nerves and blood vessels.Early diagnosis and early surgery are still effective and can reduce complications.The data of this study showed a surgical resection rate of 92.5%,no surgery-related mortality,and an incidence of postoperative complications of 29.7%.Those patients who did not take surgical therapy gradually showed tumor progression,cranial nerve injuries,and even death in the follow-up period.
Malignant carotid body tumor in general population was around 2%-8%.8In the patients in this study,the malignant ratio was 6.7% (8/120),consistent with the previously reported data.However,the recurrence rate of malignant tumors was much higher (75%),and the patients always have a poor prognosis.9Pathological diagnosis of carotid body tumor is still controversial.It has been showed that even though the tumor cell atypia is not obvious,local lymph nodes or distant metastases could still be found.On the other hand,some tumors present histological malignancy,but no recurrence evidence is observed during follow-up after radical surgical resection.Therefore,the malignant pathological possibility based on histological findings,such as the arrangement of tumor cells in nests,cellular pleomorphism,more nuclear split,and central necrosis and vascular invasion,could not clearly distinguish between benign and malignant tumors.10The differential diagnosis should thus be based on both the histological findings and biological behavior of the tumor,such as local invasion,adjacent organ invasion,solid organs and lymph nodes erosion,and even remote metastases.11
One patient in the present study had a bilateral carotid body tumor and a mediastinal tumor.During preoperative investigation at the neck and mediastinum,the patient showed a transient increase in blood pressure,suggesting the carotid body tumor might be functional.However,after resecting the mediastinal tumor,his blood pressure returned to normal,and remained such in postoperative follow-up,with no recurrence.That result excluded a functional carotid body tumor.Literature suggested that 5% of carotid body tumors were functional,12which secret catecholamines or dopamine.Although no functional carotid body tumor has been found in our hospital so far,it is worth noting that the carotid body tumor may be part of multiple endocrine neoplasia.
The need of common carotid artery pressure test or Matas test for patients is still controversial.Some reports confirmed with ultrasound that percutaneous pressure of common carotid artery could not totally block the blood flow and shunt flow from the external to the internal carotid artery to improve the intracranial blood supply.13Nevertheless,all of our patients underwent preoperative Matas training.Sometimes preoperative TBO is performed to confirm the compensation of cerebral circulation and fully assess the risk of surgery.14
Three patients (2.5%) in this study had postoperative stroke.The cerebral infarction rate was higher as 4.5%from 1949-2000,15and reduced to the 1.3% from 2001-2011 in this study.Those 3 cases were all type III in Shamblin classification,and during surgery,no involved carotid arteries were reconstructed for various reasons.This result indicates the necessity of carotid artery reconstruction in operation.In recent years in the present study,12 difficult cases were performed with carotid arteries reconstruction,using artificial grafts in 5 cases,autologous vein in 6 cases,and internal jugular vein in 1 case.Anticoagulation or antiplatelet therapy was continued after operation.All the 12 patients were free from central nerve syndromes.
Although the rate of cerebral infarction has significantly declined,the cranial nerve injury rate is still around 20%.16Cranial nerve injury in this study was 25% (30/120).Large size of the tumor indicated more nerve complications.In addition,the most vulnerable nerve was the hypoglossal nerve (15/30),followed by the vagus nerve (10/30),and sympathetic nerve (5/30).In addition to the direct impact by the tumor invasion,the nerve injury may also be related with local anatomy.Hypoglossal nerve goes over the external and internal carotid artery in the mandibular angle at the bow.It is necessary to detach the nerve in almost all the carotid body tumor surgeries.Vagus nerve in the neck is very close to internal and common carotid arteries,while sympathetic nerve is located deeply under the surface of pre-vertebral fascia,thus hardly damaged during the operation unless it is eroded directly by the tumor.In order to avoid the occurrence of nerve injury,early diagnosis and careful surgical treatment are significant.
In conclusion,it is important to have an early diagnosis for the carotid body tumor.Given its special location,an appropriate surgical time and procedure can decrease the incidence of severe complications.
1.Wang SJ,Wang MB,Baraskas TM,et al.Surgical management of carotid body tumors.Otolaryngol Head Neck Surg 2000;123:202-6.
2.Grotemeyer D,Loghmanieh SM,Pourhassan S,et al.Dignity of carotid body tumors.review of the literature and clinical experience.Chirurg 2009;80:854-63.
3.Shamblin WR.Carotid body tumor.Clinicopathologic analysis of ninety cases.Am J Surg 1971;122:732-9.
4.Knight TT Jr,Gonzalez JA,Rary JM,et al.Current concepts for the surgical management of carotid body tumor.Am J Surg 2006;191:104-10.
5.Zhang LH,Yang N,Feng F,et al.Comparative diagnostic imaging of the carotid body tumor.Chin J Med Imag Technol 2008;24:51-3.
6.Kramer M,Vairaktaris E,Nkenke E,et al.Vascular mapping of head and neck:computed tomography angiography versus digital subtraction angiography.J Oral Maxillofac Surg 2008;66:302-7.
7.Sajid MS,Hamilton G,Baker DM,et al.A multicenter review of carotid body tumor management.Eur J Vasc Endovasc Surg 2007;34:127-30.
8.Pacheco-Ojeda L.Malignant carotid body tumors:reports of three cases.Ann Otol Rhinol Laryngol 2001;110:36-40.
9.Qin RF,Shi LF,Liu YP,et al.Diagnosis and surgical treatment of carotid body tumors:25 years’ experience in China.Int J Oral Maxillofac Surg 2009;38:713-8.
10.Georgiadis GS,Lazarides MK,Tsalkidis A,et al.Carotid body tumor in a 13-year-old child:case report and review of the literature.J Vasc Surg 2008;47:874-80.
11.Hall TC,Renwick P,Stafford ND.Recurrent familial malignant carotid body tumour presenting with lymph node metastasis:case report,and review of diagnosis and management of familial carotid body tumours.J Laryngol Otol 2010;124:1344-6.
12.Al-Harthy M,Al-Harthy S,Al-Otieschan A,et al.Comparison of pheochromocytomas and abdominal and pelvic paragangliomas.Endocr Pract 2009;15:194-202.
13.Zhang XM,Li W,Zhang XM,et al.Application of carotid shunt in extra-cranial vascular surgery:report of 23 cases.Chin J Gen Surg 2002;17:657-9.
14.Wang ZG,Pan SL.Surgical treatment of carotid body tumor.Chin J Gen Sug 2002;11:396-8.
15.Zheng YH,Guan H,Liu CW,et al.Surgical treatment of carotid body tumor of 44 cases report.Tumor 2002;22:64-6.
16.Wang YQ,Chen B,Fu WG,et al.Postoperative complications of patients undergoing resection of carotid body tumor.Chin J Gen Surg 2005;20:549-51.
 Chinese Medical Sciences Journal2011年4期
Chinese Medical Sciences Journal2011年4期
- Chinese Medical Sciences Journal的其它文章
- Neurological Manifestations of Takayasu Arteritis
- Efficacy and Safety of Low Molecular Weight Heparin Prophylaxis for Venous Thromboembolism Following Lumbar Decompression Surgery
- Contrary Regulation of TIMP-1 and MMP-9 by Hepatocyte Growth Factor Antibody after Lung Injury
- Atypical Chronic Myeloid Leukaemia with Trisomy 13:a Case Report
- Surgical Removal of a Giant Vegetation on Permanent Endocavitary Pacemaker Wire and Lead
- Open Partial Nephrectomy in Solitary Kidney with Multiple Renal Cell Carcinoma:a Case Report
