Efficacy and Safety of Low Molecular Weight Heparin Prophylaxis for Venous Thromboembolism Following Lumbar Decompression Surgery
Zhi-jian Sun,Yu Zhao*,Giu-xing Qiu,Yi-peng Wang,Xi-sheng Weng,Hong Zhao,Jian-xiong Shen,Yu Jiang,Ye Li,and Xiang Li
Department of Orthopedics,Peking Union Medical College Hospital,Chinese Academy of Medical Sciences &Peking Union Medical College,Beijing 100730,China
VENOUS thromboembolism (VTE) includes deep venous thrombosis (DVT) and pulmonary embolism (PE).Total knee arthroplasty,total hip arthroplasty,and hip fracture surgery are all associated with a high incidence of postoperative VTE,resulting in high mortality.1,2There is a consensus on standardised VTE prophylaxis for these operations.3,4However,few reports have been published discussing the use of prophylactic anticoagulation following spine surgery.Glotzbecker et al5surveyed 94 spine surgeons regarding their use of prophylactic anticoagulation,and found significant inconsistencies,with 63% of the surgeons replying that they relied on personal experience to manage anticoagulation.Owing to the lack of published data and evidence,the American College of Chest Physicians (ACCP)guidelines for DVT prevention (8th edition) do not provide definitive guidelines for spine surgery patients,but suggest the use of either pharmacological or mechanical prophylaxis for VTE in patients with other risk factors.3Pharmacological prophylaxis can be achieved with low dose unfractionated heparin (Grade 1B recommendation) or low molecular weight heparin (LMWH) (Grade 1B recommendation),which is strongly recommended by ACCP guidelines.
One reason for the uncertainty is that the incidence of VTE after elective spine surgery without prophylactic anticoagulation varies in different reports.Glotzbecker et al6undertook an analysis of 25 articles and found a DVT range of 0.3%-31% following spine surgery,with an overall incidence of 2.1% (181/8618).Sansone et al7reviewed 14 studies including 4383 patients,in whom the incidence of DVT was 1.09% and the incidence of PE was 0.06% following elective spine surgery.In patients with pre-existing VTE risk factors,the incidence of postoperative VTE is greatly increased.8Some authors think the incidence is also related to the type of spine surgery,with major spinal reconstruction placing patients at greater risk.9,10
Although the incidence of VTE after elective spine surgery varies and the debate regarding the need for prophylactic anticoagulation is going on,many patients with degenerative lumbar spine have concomitant cardiovascular disease for which postoperative anticoagulation treatment is required.It is therefore also necessary to evaluate the safety of anticoagulation treatment in the patients at high risk early after lumbar spine surgery.
Apart from insufficiency in published data,surgeons have concerns regarding the safety of anticoagulation treatment in the perioperative period,such as the risk of increasing bleeding complications (e.g.subdural haematoma).How to prevent VTE with anticoagulation safely following lumbar decompression surgery in normal clinical practice? To answer this question,a prospective observational study was carried out to evaluate the safety of LMWH administration for VTE prophylaxis following lumbar decompression surgery.
PATIENTS AND METHODS
Patients
The present study enrolled patients admitted to the Peking Union Medical College Hospital from January 2004 to April 2011 for lumbar decompression surgery,who were classified as having high risk or the highest risk of VTE according to the 6th edition of ACCP Venous Thromboembolism Prevention Guideline and Levels of Thromboembolism Risk in Surgical Patients without Prophylaxis (Table 1).11Patients with haemorrhagic disease or other contraindications to LMWH were excluded.
The study protocol was approved by the Ethics Committee of Peking Union Medical College Hospital,and informed consent was obtained from all the enrolled patients.
VTE prevention
Following posterior lumbar spinal decompression under general anaesthesia,all patients received a half dose of LMWH (2050 U) administered subcutaneously 6 hours after surgery,followed by a full dose (4100 U) once per day until discharge.Ambulation was encouraged for discharged patient as further VTE prophylaxis.
Wound drain was removed when 24-hour drainage volume was less than 50 mL,and was scheduled 2 hours prior to LMWH administration (Fig.1).
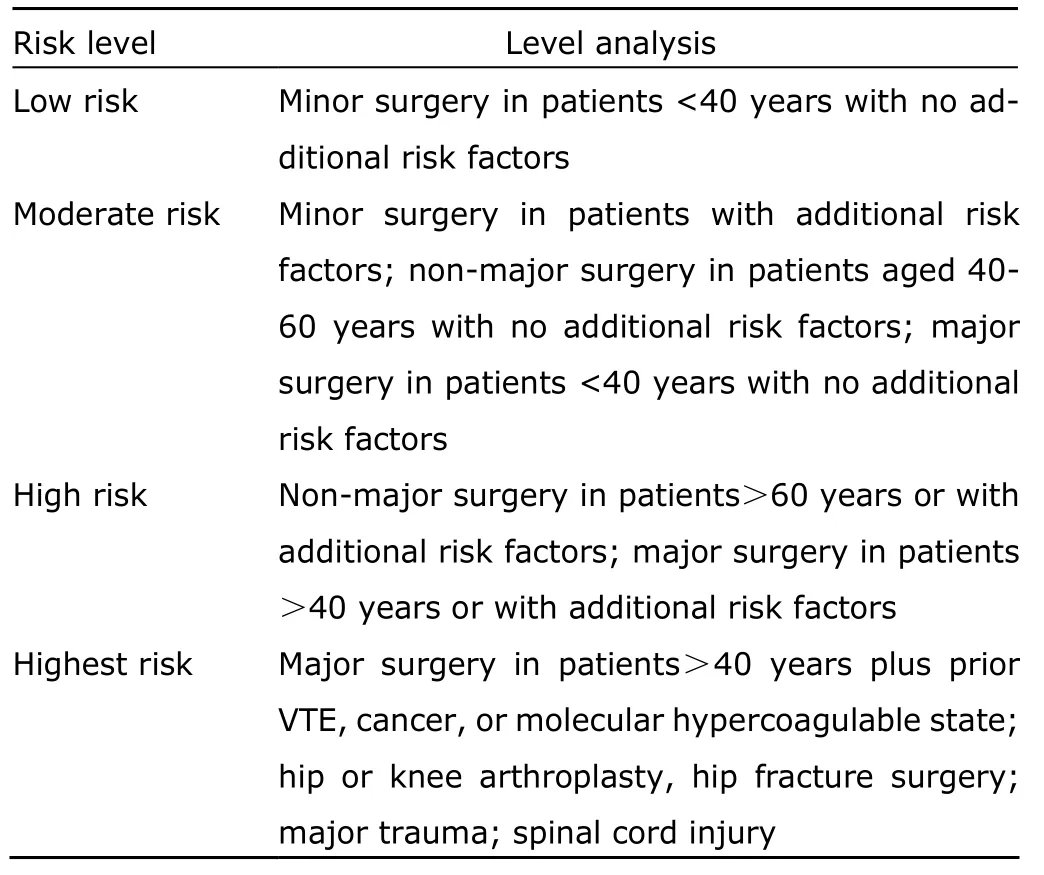
Table 1.Levels of thromboembolism risk in surgical patients without prophylaxis
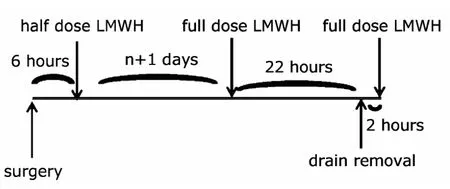
Figure 1.Timing of drain removal in lumbar decompression patients receiving low molecular weight heparin (LMWH)treatment.
Efficacy of LMWH prophylaxis
We used the Wells’ score to evaluate postoperative DVT and PE probability (Fig.2).12,13Patients with a DVT score≥2 or a PE score ≥4 underwent a D-dimer test.If the D-dimer results were negative (<500 μg/L),DVT and PE were temporarily excluded,and patients were closely observed.If the D-dimer results were positive (≥500 μg/L),lowerlimb venous compression ultrasonography (VCUS) was performed in patients with suspected DVT,and computed tomographic pulmonary angiography (CTPA) in patients with suspected PE.Definitive diagnosis of DVT or PE was made if these investigations showed positive results.In patients with negative D-dimer results but with high clinical suspicion of VTE,lower-limb VCUS or CTPA were also performed as a precaution (Fig.2).
Safety of LMWH prophylaxis
Standard postoperative wound observations,wound drainage volume,and drain removal time were carefully recorded.Patient symptoms were noted,and lower limb sensation,muscle tone and strength were under regular examination.Computed tomography or magnetic resonance imaging was undertaken to rule out compression of the spinal cord by haematoma or a dural haematoma if there was a sudden deterioration in limb signs.Instances of bleeding and observations of LMWH administration sites including skin colour changes were recorded.Major haemorrhage was defined as acute bleeding fulfilling at least one of the following conditions:decrease in haemoglobin level by 20 g/L or more within 24 hours,transfusion requirement of two units or more of red blood cells,bleeding at a crucial site (including intracranial,spinal canal,intraocular,pericardial,retroperitoneal),bleeding at the surgical site requiring intervention,or intramuscular haemorrhage causing compartment syndrome.14All other types of bleeding were defined as minor.
Aminotransferase levels and signs of allergic reaction were recorded.Thrombocytopenia was defined as a postoperative platelet count <100×109/L if the preoperative count was >150×109/L,or a 50% reduction after surgery if the preoperative count was <150×109/L.15
RESULTS
General characteristics of the patients
Altogether 78 consecutive patients were eligible and enrolled,of which 10 cases had a diagnosis of lumbar spondylolisthesis,55 cases had lumbar spinal stenosis,and 13 cases had lumbar disc herniation.The mean age was 62.4±10.6 years,with 29 males (37.2%) and 49 females(62.8%).The average hospital stay was 24.9±20.4 days.Lumbar decompression surgery was performed in 65 cases(83.3%),and lumbar laminectomy and discectomy in 13 cases (16.7%).All the patients received the operation under general anaesthesia,with the mean surgical time being 174.2±62.8 minutes.The mean intraoperative blood loss was 441±364.7 mL,with 30 cases (38.5%) requiring intraoperative blood transfusion (autologous or allogeneic)and five cases (6.4%) requiring postoperative blood transfusion.Wound drainage tubes were placed in all except three patients with lumbar disc herniation.The mean total drainage volume was 319.5±218.5 mL,and the time of drain removal was 108±36 hours after surgery on average.The mean time to mobilisation after surgery was 5.5±1.9 days (Table 2).
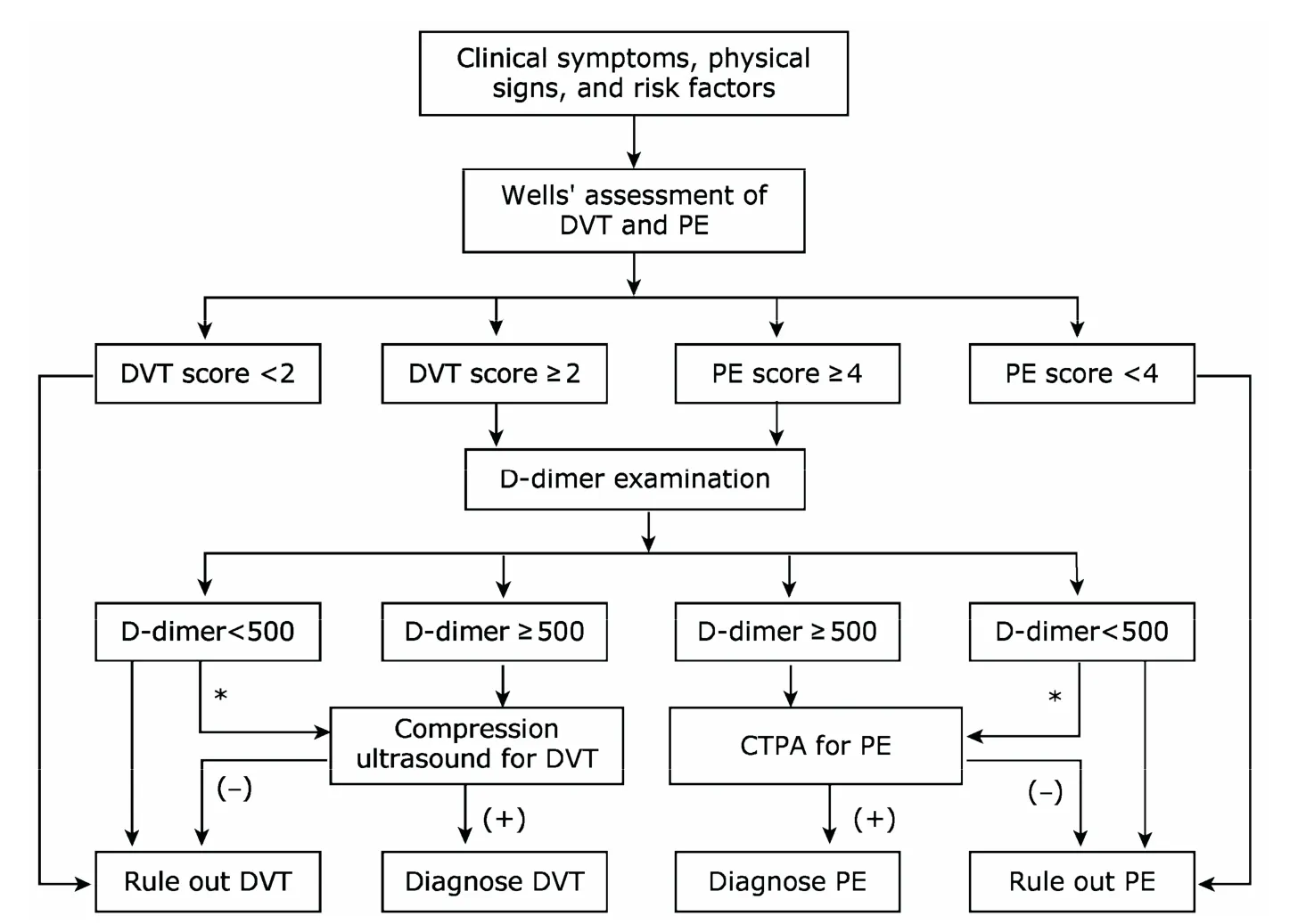
Figure 2.Diagnostic flowchart for DVT and PE following lumbar decompression surgery.
Efficacy and safety analysis results
Postoperative VTE risk assessments categorised 72 cases(92.3%) as having high risk and 6 (7.7%) as having the highest risk.One of the highest risk patients already had a history of DVT prior to surgery.The average anticoagulation time was 8.5±4.5 days.
In the 3 cases with a postoperative Wells’ DVT score ≥2,D-dimer tests were performed,followed by lower-limb VCUS in two cases.No thrombus formation was detected in any of these three cases.In the 4 cases with a postoperative Wells’ PE score ≥4,D-dimer tests were conducted,followed by CTPA in one case.PE was excluded in these 4 patients (Table 3).The patient with a DVT history was taking warfarin prior to admission and was switched to LMWH treatment upon hospitalisation;this patient did not experience any VTE recurrence during hospital stay.
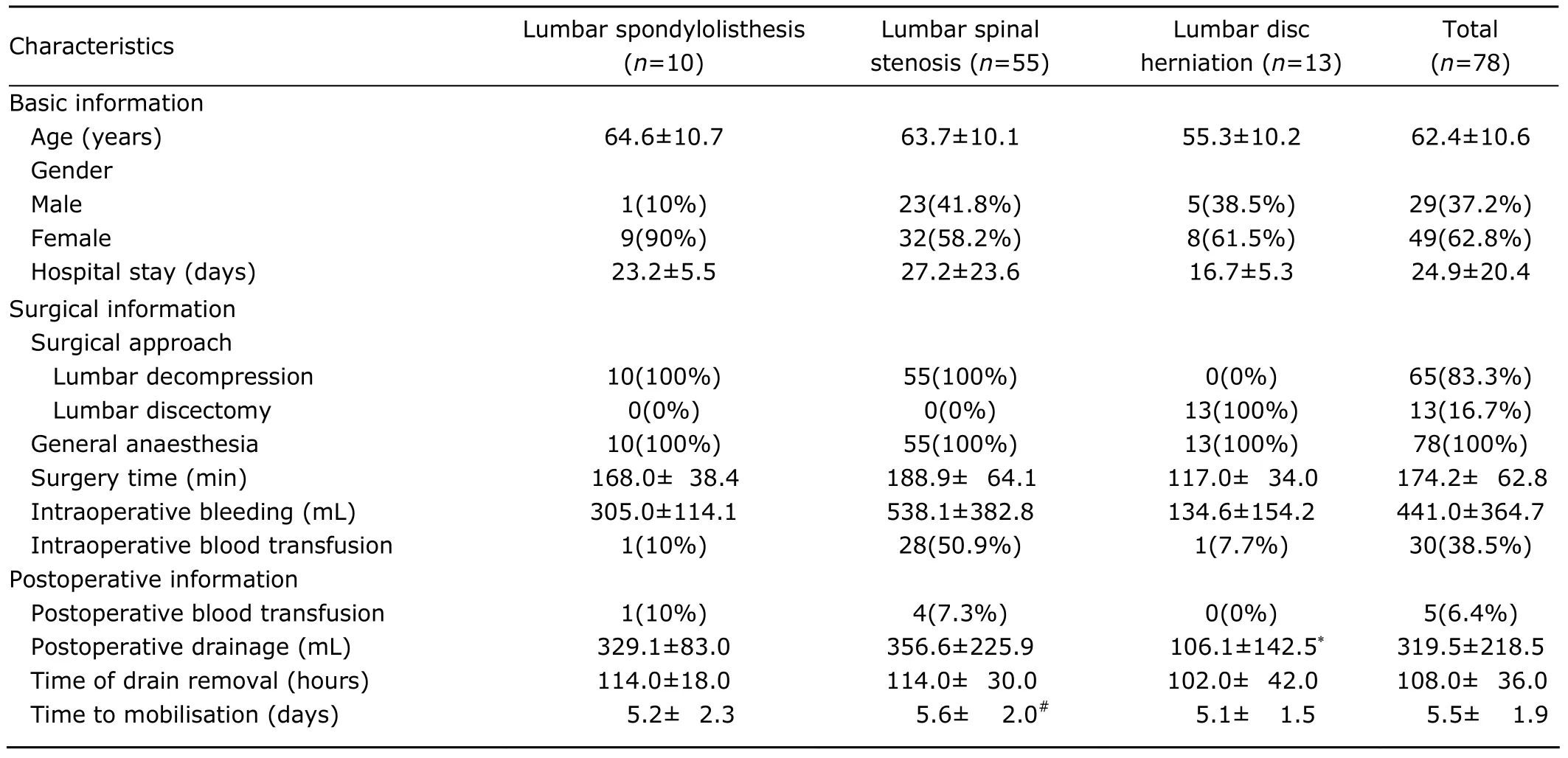
Table 2.Baseline,surgical,and postoperative characteristics of the enrolled cases
No major haemorrhagic events were encountered in this study.One case developed wound ecchymosis and another had wound oozing.Four cases showed mild elevation in aminotransferase level,but none had decreased platelet count or severe heparin-induced thrombocytopenia.One patient developed a suspicious allergic reaction,presenting with red skin rash over the abdomen and both lower limbs without other positive physical signs such as heart rate or blood pressure changes,which recovered with medication (Table 3).LMWH was continued in all the cases.
DISCUSSION
The risk of VTE increases in patients after lumbar decompression surgery,especially in those with additional risk factors.8Chemical prophylaxis in these patients was considered appropriate.In spite of that,bleeding complications,especially subdural haematoma,was the major concern of spine surgeons during chemoprophylaxis due to the exposure of spinal dural mater during surgery.
Regarding complications after anticoagulation treatment following spine surgery,Cheng et al16reported that the incidence of anticoagulation-induced haemorrhagic complications was low,with a 0%-4.3% incidence of major bleeding.Gerlach et al17analysed 1949 post-spine-surgery patients treated with LMWH,and found only 8 cases of postoperative haematoma,with an incidence of 0.4%.In the present study,there was no occurrence of major haemorrhagic complications,and only one case of wound bruising and another of wound oozing,suggesting that administration of LMWH is quite safe.Previous reports have indicated that adverse reactions of LMWH are low,18,19and no serious adverse reactions were observed in this study.Four cases had elevated aminotransferase level and one had a suspicious allergic reaction,but LMWH was not discontinued in any of these cases.For the patient with a suspicious allergic reaction,no further examinations were taken since the red skin rash disappeared after topical drug treatment.Care should be taken,however,to monitor patients for adverse drug reactions,as indicated by various LMWH pharmacology reports and articles.20,21
This study included patients at high risk and the highest risk of VTE,who received regular LMWH administration along with adjunct mechanical therapy measures.The first dose of LMWH was administered 6 hours after surgery.Postoperative administration protects against interactions with anaesthetic drugs and against increased intraoperative bleeding.This 6-hour postoperative timing has been demonstrated to effectively prevent VTE following major lower limb procedures without increasing bleeding risks.22Drain removal was 2 hours prior to LMWH administration,when blood levels were at their lowest,thus reducing the risk of bleeding during the removal process.The 2-hour interval before LMWH administration allowed for clotting within the wound,thus decreasing internal wound bleeding and preventing haematoma formation and compression of the spinal cord.23None of the patients in this study bled during the drain removal process.
DVT and PE diagnosis during anticoagulation treatment were made strictly in accordance with Wells’ scoring system and D-dimer test results,with suspicious cases undergoing lower-limb VCUS or CTPA.The studies by Wells et al12,13demonstrated that the Wells’ analysis together with D-dimer test could efficiently detect VTE,greatly reducing the costs by decreasing the requirements for more expensive VCUS and CTPA.
Voth et al24compared the efficacy of LMWH versus heparin for VTE prophylaxis in spine surgery.Postoperative treatment time was 8.0 days with LMWH and 7.6 days with heparin.There were only 2 cases (2/92) of symptomatic DVT in the heparin group,and 1 case (1/87) in the LMWH group,with no PE detected in either group.Otero-Fernández et al25reported the application of LMWH prophylaxis for VTE in 231 spine surgery patients,observing no cases of DVT or PE.The present study also indicates that LMWH is effective for VTE prophylaxis;there were no cases of DVT or PE among the 78 enrolled patients.
Apart from LMWH treatment,early ambulation was encouraged for all patients to prevent VTE in this study.The mean time of mobilization in this group of patients was 5.5±1.9 days.However,two cases with lumbar spinal stenosis complicated by hemiplegia did not mobilise prior to discharge.
The present study has limitations.For instance,we did not undertake routine test for VTE during the anticoagulation period,which may have allowed asymptomatic VTE to go undetected.6,7In conclusion,the present study results show that LMWH could prevent VTE in patients at high risk and the highest risk who underwent lumbar spine surgery,with a low incidence of hemorrhagic complications.
1.Liew NC,Moissinac K,Gul Y.Postoperative venous thromboembolism in Asia:a critical appraisal of its incidence.Asian J Surg 2003;26:154-8.
2.Cordell-Smith JA,Williams SC,Harper WM,et al.Lower limb arthroplasty complicated by deep venous thrombosis:prevalence and subjective outcome.J Bone Joint Surg Br 2004;86:99-101.
3.Geerts WH,Bergqvist D,Pineo GF,et al.Prevention of venous thromboembolism:American College of Chest Physicians Evidence-Based Clinical Practice Guidelines(8th Edition).Chest 2008;133:381S-453S.
4.Haas SB,Barrack RL,Westrich G,et al.Venous thromboembolic disease after total hip and knee arthroplasty.J Bone Joint Surg Am 2008;90:2764-80.
5.Glotzbecker MP,Bono CM,Harris MB,et al.Surgeon practices regarding postoperative thromboembolic prophylaxis after high-risk spinal surgery.Spine (Phila Pa 1976) 2008;33:2915-21.
6.Glotzbecker MP,Bono CM,Wood KB,et al.Thromboembolic disease in spinal surgery:a systematic review.Spine(Phila Pa 1976)2009;34:291-303.
7.Sansone JM,del Rio AM,Anderson PA.The prevalence of and specific risk factors for venous thromboembolic disease following elective spine surgery.J Bone Joint Surg Am 2010;92:304-13.
8.Anderson FA Jr,Spencer FA.Risk factors for venous thromboembolism.Circulation2003;107:I9-16.
9.Brambilla S,Ruosi C,La Maida GA,et al.Prevention of venous thromboembolism in spinal surgery.Eur Spine J 2004;13:1-8.
10.Samama CM,Albaladejo P,Benhamou D,et al.Venous thromboembolism prevention in surgery and obstetrics:clinical practice guidelines.Eur J Anaesthesiol 2006;23:95-116.
11.Geerts WH,Heit JA,Clagett GP.Prevention of venous thromboembolism.Chest2001;119:132S-75S.
12.Wells PS,Anderson DR,Rodger M,et al.Derivation of a simple clinical model to categorize patients probability of pulmonary embolism:increasing the models utility with the SimpliRED D-dimer.Thromb Haemost 2000;83:416-20.
13.Wells PS,Anderson DR,Rodger M,et al.Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis.N Engl J Med 2003;349:1227-35.
14.Schulman S,Kearon C,Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis.Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients.J Thromb Haemost2005;3:692-4.
15.Lassen MR,Gallus A,Raskob GE,et al.Apixaban versus enoxaparin for thromboprophylaxis after hip replacement.N Engl J Med.2010;363:2487-98.
16.Cheng JS,Arnold PM,Anderson PA,et al.Anticoagulation risk in spine surgery.Spine (Phila Pa 1976) 2010;35:S117-24.
17.Gerlach R,Raabe A,Beck J,et al.Postoperative nadroparin administration for prophylaxis of thromboembolic events is not associated with an increased risk of hemorrhage after spinal surgery.Eur Spine J 2004;13:9-13.
18.Testroote M,Stigter W,de Visser DC,et al.Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization.Cochrane Database Syst Rev 2008;(4):CD006681.
19.Salazar CA,Malaga G,Malasquez G.Direct thrombin inhibitors versus vitamin K antagonists or low molecular weight heparins for prevention of venous thromboembolism following total hip or knee replacement.Cochrane Database Syst Rev 2010;(4):CD005981.
20.Liebman HA.Heparin-induced thrombocytopenia:diagnosis and management.Vascular 2008;16 Suppl 1:S71-6.
21.Jappe U.Allergy to heparins and anticoagulants with a similar pharmacological profile:an update.Blood Coagul Fibrinolysis 2006;17:605-13.
22.Raskob GE,Hirsh J.Controversies in timing of the first dose of anticoagulant prophylaxis against venous thromboembolism after major orthopedic surgery.Chest 2003;124:379S-85S.
23.Horlocker TT,Wedel DJ,Rowlingson JC,et al.Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy:American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines(Third Edition).Reg Anesth Pain Med 2010;35:64-101.
24.Voth D,Schwarz M,Hahn K,et al.Prevention of deep vein thrombosis in neurosurgical patients:a prospective double-blind comparison of two prophylactic regimens.Neurosurg Rev 1992;15:289-94.
25.Otero-Fernández R,Gómez-Outes A,Martínez-González J,et al.Evaluation of the effectiveness and safety of bemiparin in a large population of orthopedic patients in a normal clinical practice.Clin Appl Thromb Hemost 2008;14:75-83.
 Chinese Medical Sciences Journal2011年4期
Chinese Medical Sciences Journal2011年4期
- Chinese Medical Sciences Journal的其它文章
- Efficacy of Surgical Therapy for Carotid Body Tumors
- Neurological Manifestations of Takayasu Arteritis
- Contrary Regulation of TIMP-1 and MMP-9 by Hepatocyte Growth Factor Antibody after Lung Injury
- Atypical Chronic Myeloid Leukaemia with Trisomy 13:a Case Report
- Surgical Removal of a Giant Vegetation on Permanent Endocavitary Pacemaker Wire and Lead
- Open Partial Nephrectomy in Solitary Kidney with Multiple Renal Cell Carcinoma:a Case Report
