Development and validation of a novel nomogram for predicting overall survival in gastric cancer based on inflammatory markers
Pan-Quan Luo,En-Dong Song,Fei Liu,Abigail N Rankine,Li-Xiang Zhang,Zhi-Jian Wei,Wen-Xiu Han,A-Man Xu
Pan-Quan Luo,En-Dong Song,Li-Xiang Zhang,Zhi-Jian Wei,Wen-Xiu Han,A-Man Xu,Department of General Surgery,The First Affiliated Hospital of Anhui Medical University,Hefei 230022,Anhui Province,China
Fei Liu,Faculty of Medical Technology,Ophthalmology Laboratory,Anhui Medical College,Hefei 230601,Anhui Province,China
Abigail N Rankine,Department of Clinical Medicine,Anhui Medical University,Hefei 230032,Anhui Province,China
Abstract BACKGROUND Nearly 66% of occurrences of gastric cancer(GC),which has the second-highest death rate of all cancers,arise in developing countries.In several cancers,the predictive significance of inflammatory markers has been established.AIM To identify clinical characteristics and develop a specific nomogram to determine overall survival for GC patients.METHODS Nine hundred and four GC patients treated at the First Affiliated Hospital of Anhui Medical University between January 2010 and January 2013 were recruited.Prognostic risk variables were screened for Cox analysis.The C index,receiver operator characteristic(ROC)curve,and decision curve analysis were used to evaluate the nomogram.RESULTS Tumor node metastasis stage,carcinoembryonic antigen,systemic immuneinflammation index,and age were identified as independent predictive variables by multivariate analysis.Systemic immune-inflammation index value was superior to that of other inflammatory indicators.The ROC indicated the nomogram had a higher area under the curve than other factors,and its C-index for assessing the validation and training groups of GC patients was extremely reliable.CONCLUSION We created a novel nomogram to forecast the prognosis of GC patients following curative gastrectomy based on blood markers and other characteristics.Both surgeons and patients can benefit significantly from this new scoring system.
Key Words:Gastric cancer;Nomogram;Neutrophil-to-lymphocyte ratio;Platelet-to-lymphocyte ratio;Systemic immune-inflammation index
lNTRODUCTlON
Nearly 66% of gastric cancer(GC)diagnoses,which has the second-highest death rate of all cancers[1],occur in developing countries[1,2].The only curative treatment for patients is radical surgery,which increases the likelihood of a successful cure and lengthens patient survival.The high likelihood of cancer recurrence,however,means that the 5-year overall survival(OS)is still poor even after surgery[3].The tumor node metastasis(TNM)stage is correlated with the prognosis of GC patients,but it is difficult to determine prior to surgery.Carcinoembryonic antigen(CEA)is one of the most utilized serum indicators in relation to stomach cancer according to recent research[4-6].In order to diagnose cancer and predict recurrence following surgery,CEA has been employed[4].The neutrophil-tolymphocyte ratio(NLR)and the platelet-to-lymphocyte ratio(PLR)are two additional blood indices that can be used to assess the prognosis of malignancy[5-7].Additionally,the level of hemoglobin is related to a patient’s prognosis[8].The purpose of this study was to identify additional clinical blood indicators that may be used to evaluate GC patient prognosis and create a trustworthy scoring system.
There has been much research on the connection between cancers and inflammation.Cancer caused by inflammation has been shown to damage DNA and create microscopic metastases[9].The body’s immune system may become less effective,and tumor growth may be accelerated by the systemic inflammatory response.According to a related study,lymphocytes(LY),platelets(PLT),and neutrophils(NE)have a great impact on the systemic inflammatory response,which is linked to tumor formation[10,11].The predictive usefulness of many systemic inflammation factors,such as NLR-PLR[12],PLT-NLR[13],and systemic immune-inflammation index(SII),has been well established in various malignancies[14,15].There has not been any clinical research published comparing the prognostic significance of different scoring systems.In this study,we investigated additional clinical blood indicators and created a strong nomogram for predicting OS following gastrectomy.
MATERlALS AND METHODS
Patients
From January 2010 to January 2013,904 GC patients were admitted to the First Affiliated Hospital of Anhui Medical University and provided blood samples and clinical data.All chosen participants were randomly divided into training(n= 543)and validation(n= 361)cohorts for the study’s final analysis.Our hospital’s Institutional Review Board and Ethical Committee approved this study.
Inclusion and exclusion criteria
The criteria for admission included:(1)A histological diagnosis indicated GC;(2)The malignancy was definitively and entirely removed after surgery;(3)All of the patients’ peripheral blood tests were completed within 2 d after the operation;and(4)Multiple organ failure was not present.Patients were excluded if they met any of the following criteria:(1)They had other primary tumors;(2)They had undergone radiotherapy and chemotherapy prior to surgery;(3)They had any diseases that could interfere with peripheral blood cells,such as infections;and(4)They had passed away within 1 mo after operation.Finally,a cohort of 904 GC patients was examined.
Data collection and follow-up
Through the medical records department,information on the patient’s age,sex,differentiation grade,tumor size,and other characteristics as well as clinical pathology was acquired.NE,LY,and PLT,etc.were obtained 3 d before the operation,and peripheral blood was analyzed.The CEA and hemoglobin cutoff values were obtained based on normal levels,and the median was used to determine the NE,LY,and PLT cutoff values.SII was calculated by PLT count × NE count/LY count.According to the ideal cutoff values,which were determined using the Youden index[maximum(sensitivity + specificity - 1)][16],patients were divided into low and high groups.Patients were assigned to groups based on NLR-PLR as follows:(high NLR)+(high PLR)= 2;(only one high group)= 1;(low NLR)+(low PLR)= 0.The assignment of NLR-PLT was similar.
Statistical analysis
The categorical values were analyzed by theχ2test or the Fisher exact test,and continuous variables were analyzed by the Student’sttest.The Cox appropriate hazard model was used to perform both multivariate and univariate survival analyses.In order to assess the accuracy of the prognostic model,the C-index and receiver operator characteristic(ROC)were utilized.R Studio and the SPSS program(version 19.0)were used for the full data analysis process.
RESULTS
ROC curve of SII,NLR,and PLR
By using the ROC curve of the greatest Youden index,we calculated the preoperative NLR,PLR,and SII value.Based on the Youden index,the optimal cutoff value of NLR,PLR,SII was calculated to be 2.0,160.0,and 475.6,respectively.
Clinical characteristics of the training and validation groups
Table 1 showed the clinical data of the 904 GC patients(training group = 543,validation group = 361).The training group and validation group had no statistically significant differences(P> 0.05).
Univariate and multivariate analysis of the training cohort
Prognostic factors identified by univariate analysis were sex,hemoglobin,age,TNM,NLR,tumor size,PLR,SII,and CEA(Table 2).Multivariate analysis revealed that age,CEA,SII,and TNM were independent predictive factors for GC patients(Table 3).
The ROC curve of inflammatory markers
We used the ROC curve to compare the utility of all the inflammatory indicators in GC patients(Figure 1).The area under the curve(AUC)for SII was bigger than that of NLR,NLR-PLT,PLR,and NLR-PLR.
Nomogram for OS
A novel nomogram was created to predict the OS of GC based on the multivariate analysis result(Figure 2).Table 4 revealed the nomogram scoring method.
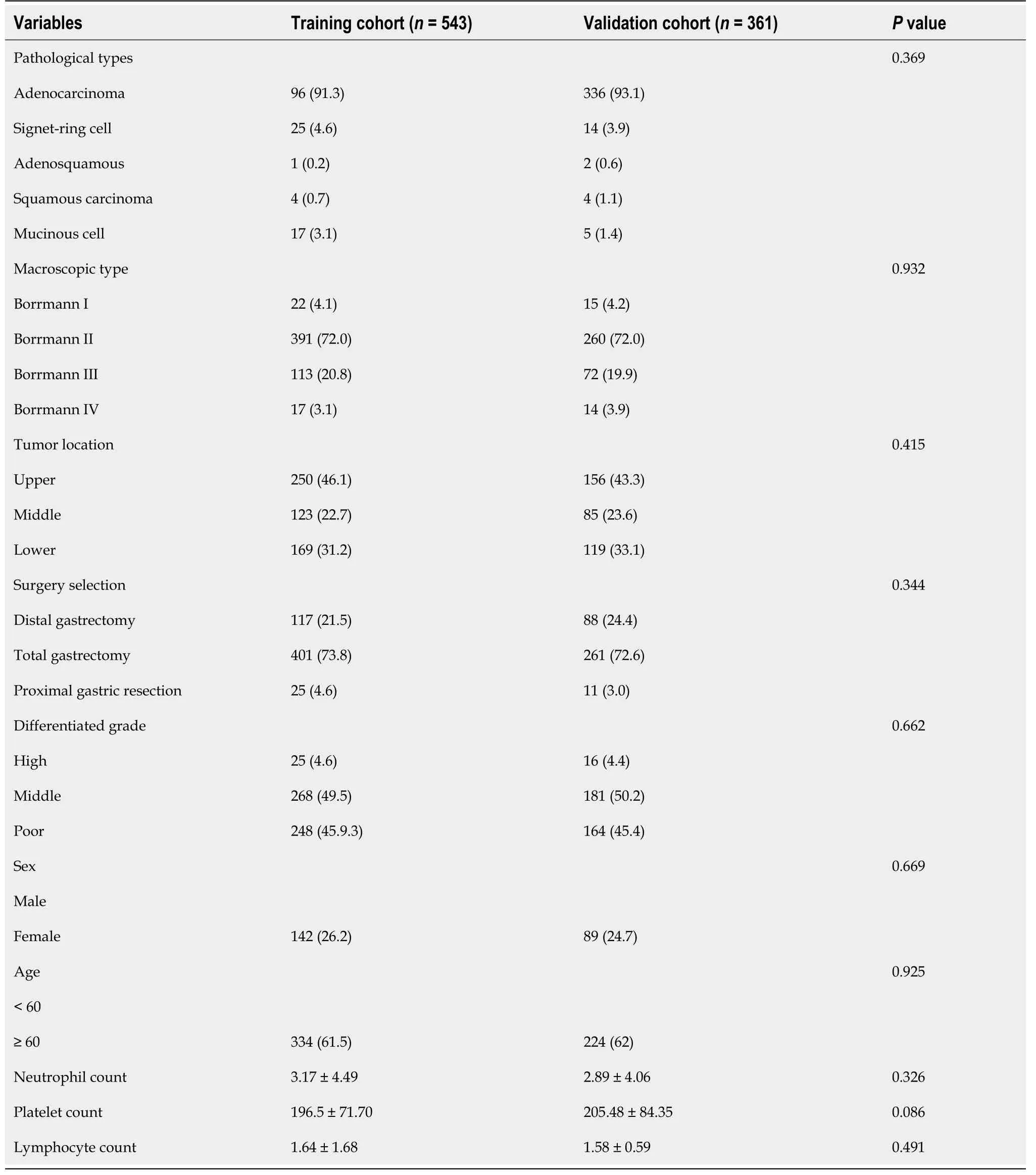
Table 1 Baseline demographics and clinical characteristics of patients in the training and validation cohorts,n(%)
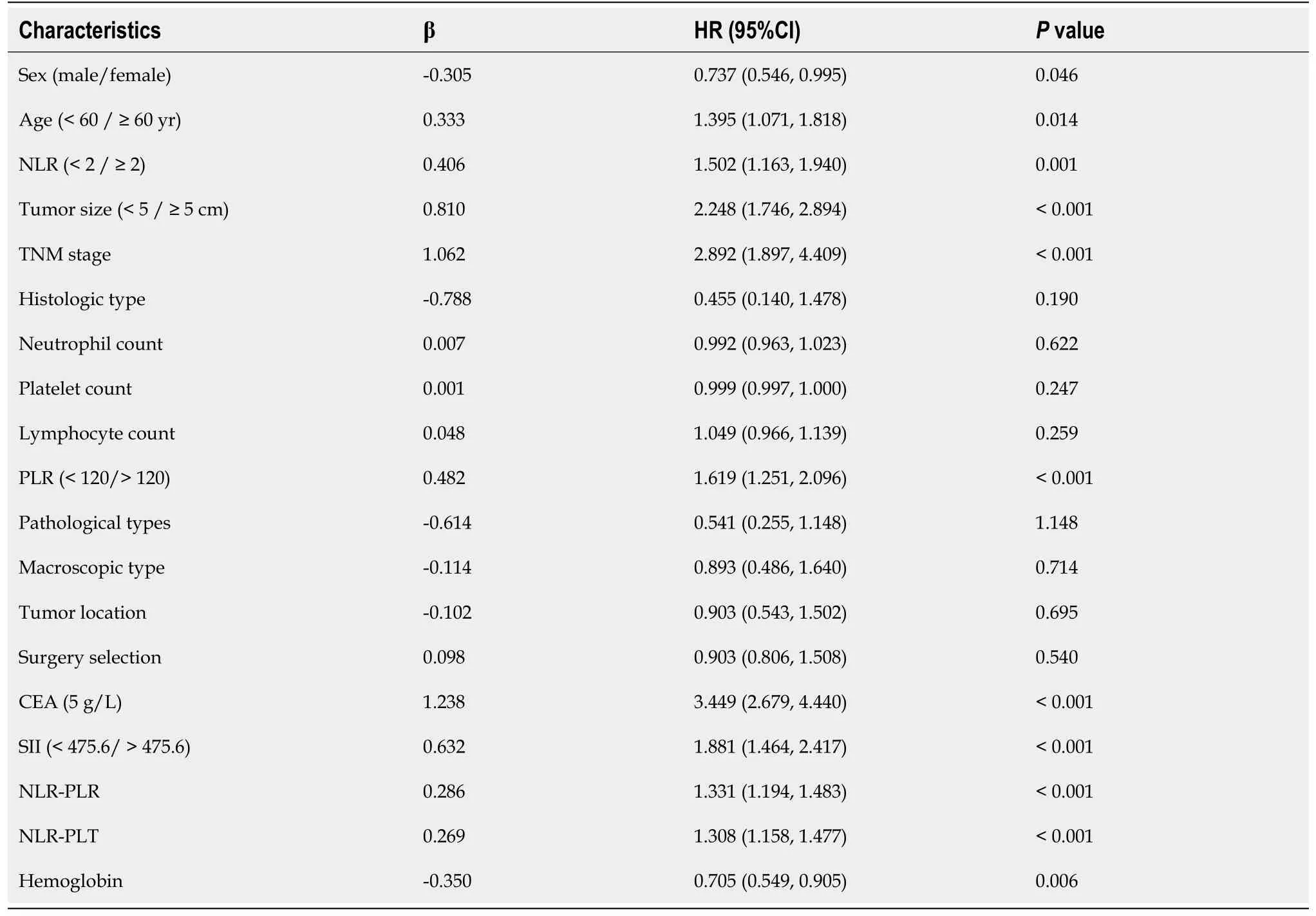
Table 2 Univariate analysis of the training cohort
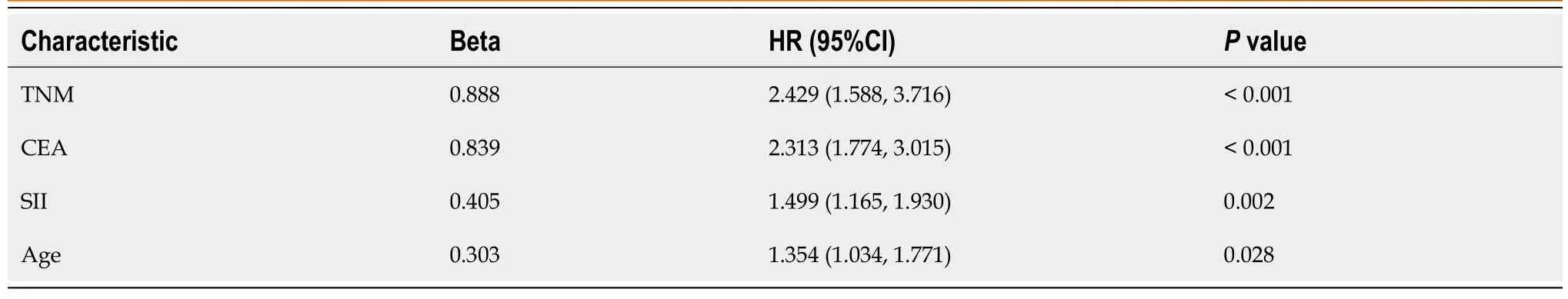
Table 3 Multivariate analysis of the training cohort
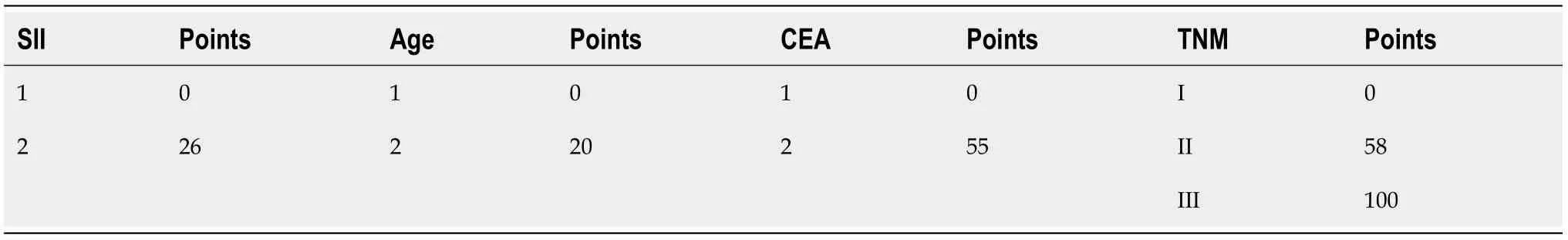
Table 4 Nomogram scoring system
Validation of the nomogram model in the training group and validation groups
We applied calibration curves to verify the model in the training and validation groups(Figure 3).In the training group,the nomogram’s C-index was 0.736,whereas in the validation group,it was 0.651.In order to further demonstrate the nomogram performance,we displayed the ROC of the nomogram(Figure 4).In addition,the AUC of the nomogram was large,showing that nomogram is dependable.
Decision curve analysis of the nomogram in the training and validation groups
Decision curve analysis results indicated the clinical use of the novel model for estimating 3-year and 5-year survival in GC patients in the training group and validation group(Figure 5).
The Kaplan-Meier curves in training group
The training group was then separated into three subgroups depending on the cutoff value(< 60 was low risk;60-120 was medium risk;> 120 was high risk).The Kaplan-Meier curve demonstrated the good outcomes(Figure 6).
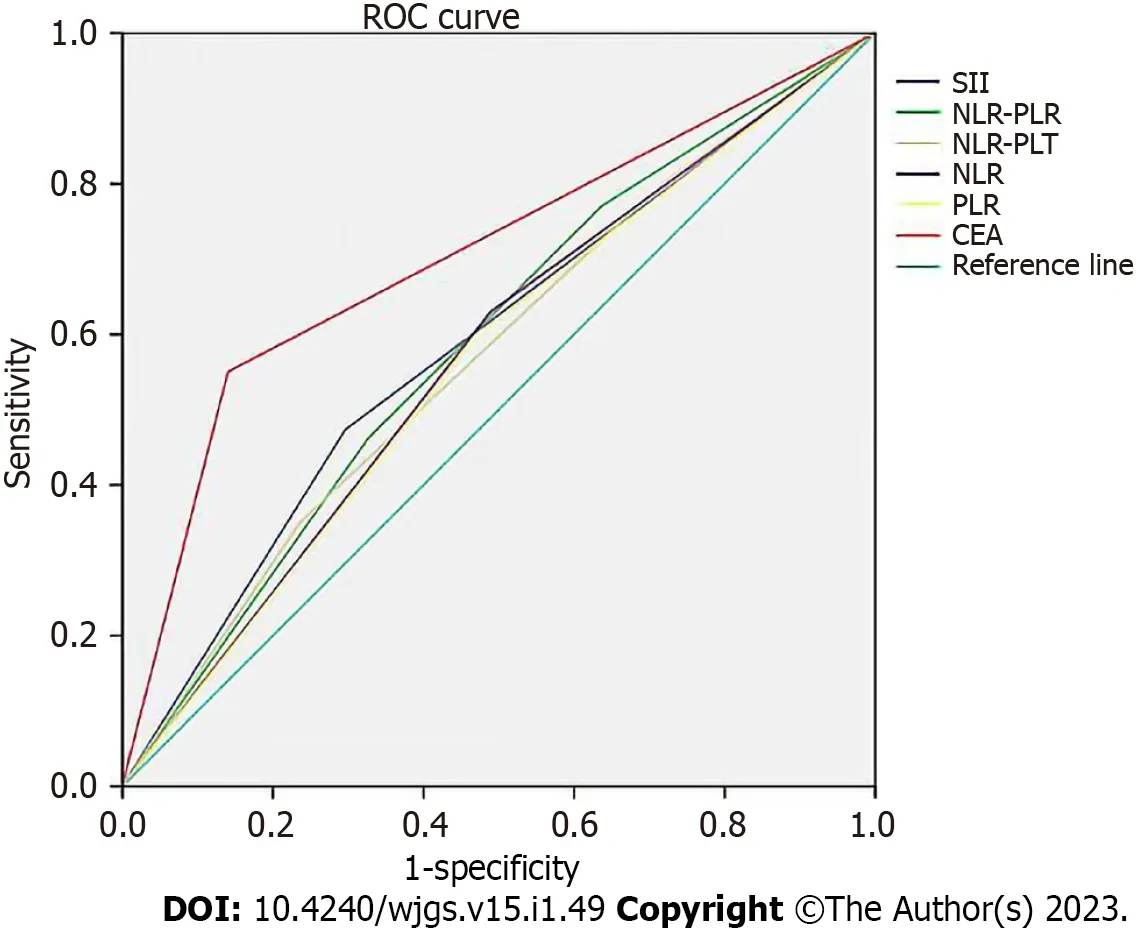
Figure 1 The receiver operator characteristic curve of the blood markers.CEA:Carcinoembryonic antigen;NLR:Neutrophil-to-lymphocyte ratio;PLR:Platelet-to-lymphocyte ratio;PLT:Platelet;ROC:Receiver operator characteristic;SII:Systemic immune-inflammation index.

Figure 2 Nomogram for predicting overall survival after curative resection of gastric cancer.CEA:Carcinoembryonic antigen;OS:Overall survival;SII:Systemic immune-inflammation index;TNM:Tumor node metastasis.
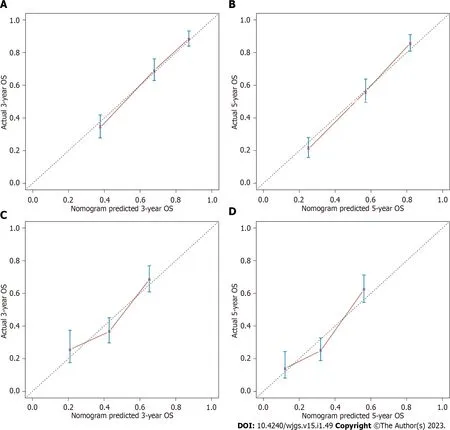
Figure 3 Calibration curves.A:The prognostic nomogram for 3-year overall survival(OS)the training set;B:The prognostic nomogram for 5-year OS in the training set;C:The prognostic nomogram for 3-year OS in the validation set;D:The prognostic nomogram for 5-year OS in the validation set.OS:Overall survival.
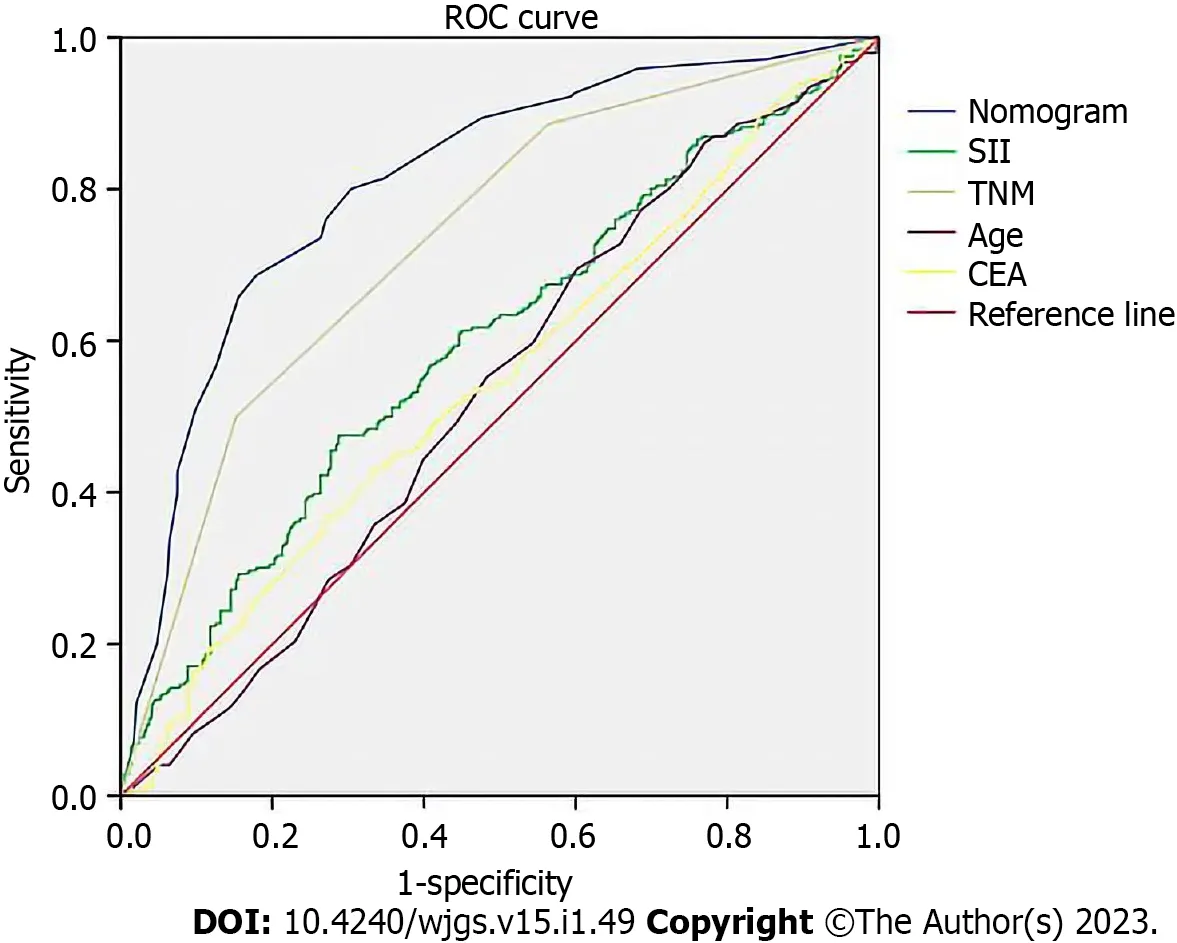
Figure 4 The receiver operating characteristic curve of the prognostic nomogram in the training set.CEA:Carcinoembryonic antigen;SII:Systemic immune-inflammation index;TNM:Tumor node metastasis;ROC:Receiver operator characteristic.
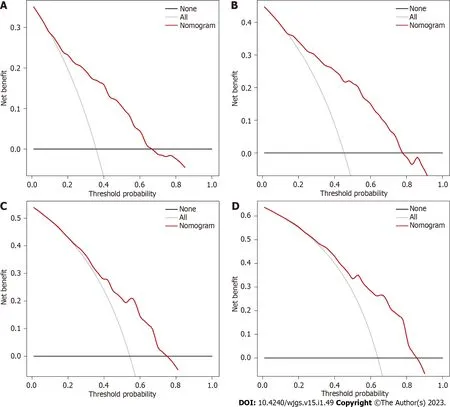
Figure 5 Decision curve analysis.A:The decision curve analysis of the prognostic nomogram for predicting 3-year overall survival in the training set;B:The decision curve analysis of the prognostic nomogram for 5-year overall survival in the training set;C:The decision curve analysis of the prognostic nomogram for 3-year overall survival in the validation set;D:The decision curve analysis of the prognostic nomogram for 5-year overall survival in the validation set.
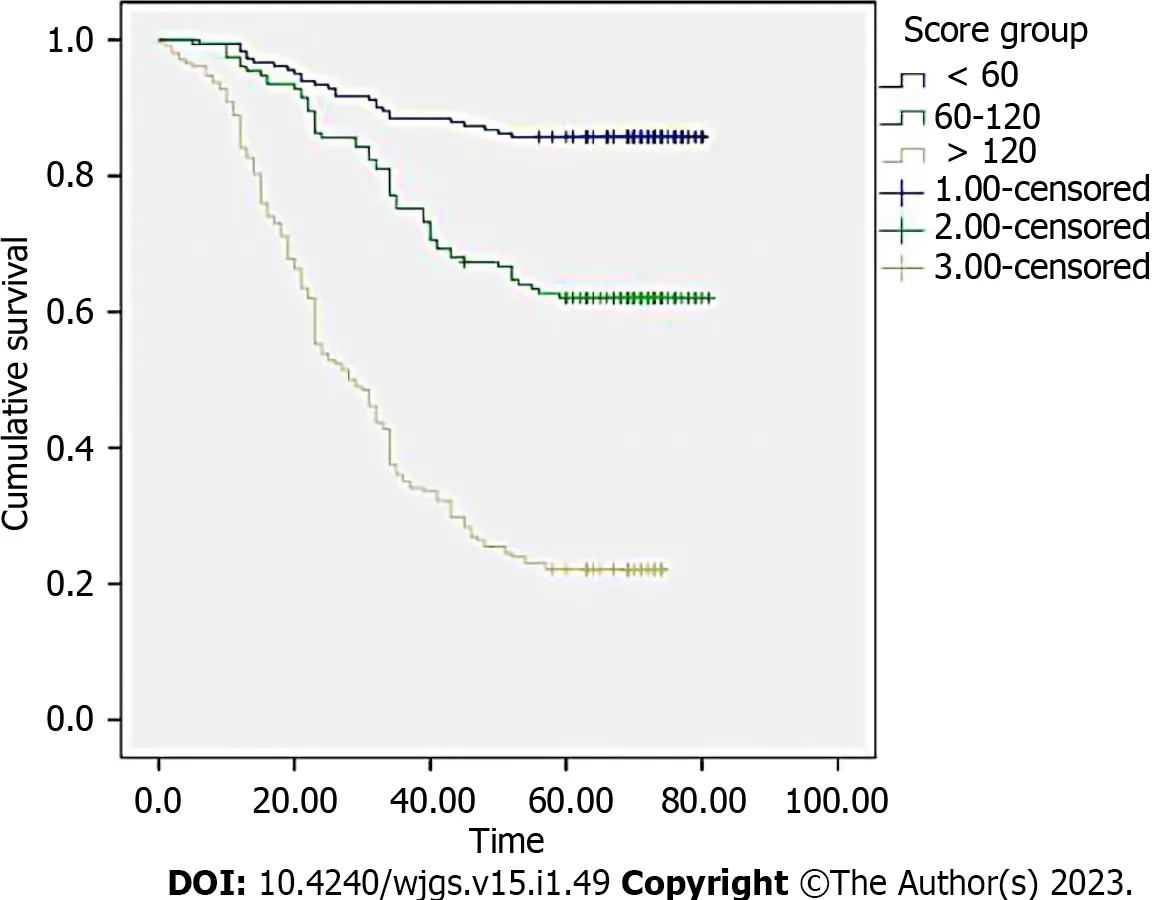
Figure 6 Survival curves stratified by the score calculated by the nomogram in the training cohort(low risk:< 60;intermediate risk:60-120;and high risk:> 120).
DlSCUSSlON
The only curative form of treatment for GC is generally believed to be surgery.Early GC is typically difficult to diagnose due to the limitations of available procedures.The 5-year survival rate at the moment is quite poor.As a result,several researchers have worked to enhance the prognosis for GC patients.TNM stage and lymph node metastases were identified as important independent risk factors.However,because it is challenging to evaluate these prognostic factors prior to surgery,substantial research has been done recently on serum markers.This study,to the best of our knowledge,is the first to compare the serum score system and then create a novel nomogram that combines peripheral blood markers and clinical factors to predict OS at 1 year,3 years,and 5 years.
The results demonstrated that age,SII,TNM stage,and CEA were each independent predictors of survival in GC patients.SII was a more effective indicator to predict OS based on the fact that its AUC was higher than that of NLR-PLR and NLR-PLT.The C-index of our newly constructed nomogram,which was based on independent prognostic variables,was 0.736,indicating that it is quite accurate in predicting GC patients’ prognoses.This nomogram is an accurate score system because the decision curve analysis and calibration curve both supported its clinical use.Nomograms are more valuable than TNM stages for predicting prognosis in several cancers[17,18].Since the nomogram’s AUC in this study was higher than other elements,surgeons may use this scoring system to accurately assess a patient’s prognosis and choose the most beneficial course of action in the clinic.
Four factors in our nomogram were significantly influenced by SII.According to recent studies,inflammation may have an impact on the development of cancer and long-term survival of patients[19].SII,which may include NE count,PLT count,and LY count,was among them but was less frequently reported.NLR-PLT and NLR-PLR were associated with GC patient prognosis,whereas SII was an independent prognostic factor and had higher value.Our study proved that CEA was a reliable prognostic factor and that it may be used to screen for cancer recurrence.As a result,we need to pay more attention to patients who have elevated levels of CEA.Age was another important prognostic factor,and this result was consistent with earlier research[20].With the increase of age,the immunity of elderly patients decreases significantly,which leads to recurrence and metastasis of cancer,thus elderly patients with GC typically have a worse outcome.As a result,these important factors need to be given more emphasis in order to improve patient outcomes,and the nomogram may be used more frequently in clinics.
CONCLUSlON
In conclusion,our research showed that age,SII,TNM stage,and CEA were major predictive factors of the prognosis of GC patients,and the new nomogram was a valid prognostic tool for them.
ARTlCLE HlGHLlGHTS
Research background
Nearly 66% of instances of gastric cancer(GC),which has the second-highest death rate of all cancers,occur in developing countries.The only curative treatment for patients is considered to be a radical surgery,which increases the likelihood of a successful cure and lengthens patient survival.
Research motivation
The high likelihood of cancer recurrence means that the 5-year overall survival(OS)is still poor even after surgery.The tumor node metastasis(TNM)stage is connected with the prognosis of GC patients,but it is difficult to determine prior to surgery.
Research objectives
To investigate more clinical characteristics and develop a specific nomogram to forecast OS for GC patients.
Research methods
Nine hundred and four GC patients treated at the First Affiliated Hospital of Anhui Medical University between January 2010 and January 2013 were recruited.Prognostic risk variables were screened using the Cox analysis.The C-index and receiver operator characteristic(ROC)curve were used to construct and evaluate the nomogram.
Research results
TNM stage,carcinoembryonic antigen,systemic immune-inflammation index,and age were identified as independent predictive variables by multivariate analysis.The systemic immune-inflammation index value was superior to that of other inflammatory indicators.The ROC indicated the nomogram had a higher area under the curve than other factors,and its C-index for assessing the validation and training groups of GC patients was extremely reliable.
Research conclusions
We created a novel nomogram to predict the prognosis of GC patients following curative gastrectomy based on the blood markers and other characteristics.
Research perspectives
Both surgeons and patients can benefit significantly from this new scoring system.The nomogram may be used more frequently in clinics.
FOOTNOTES
Author contributions:Luo PQ collected the clinical information of patients,performed the statistical analysis,and completed the writing of the manuscript;Song ED and Liu F participated in collecting the clinical information of patients and revising the statistical methods of the investigation;Luo PQ,Song ED,and Liu F contributed equally to this work;Rankine AN helped perform the statistical analysis;Zhang LX,Wei ZJ,Han WX,and Xu AM designed the main study and critically revised the manuscript,and they contributed equally to this work;All authors read and approved the final manuscript.
Supported byNatural Science Foundation of Anhui Province,No.2108085QH337.
lnstitutional review board statement:The First Affiliated Hospital of Anhui Medical University Institutional Review Board and Ethical Committee approved this study.
lnformed consent statement:All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
Conflict-of-interest statement:All authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Pan-Quan Luo 0000-0002-2828-7061;Abigail N Rankine 0000-0001-6641-9910;Zhi-Jian Wei 0000-0003-
1094 -1894;A-Man Xu 0000-0002-4060-4576.
S-Editor:Fan JR
L-Editor:Filipodia
P-Editor:Zhao S
 World Journal of Gastrointestinal Surgery2023年1期
World Journal of Gastrointestinal Surgery2023年1期
- World Journal of Gastrointestinal Surgery的其它文章
- lntestinal erosion caused by meshoma displacement:A case report
- Short-term efficacy assessment of transarterial chemoembolization combined with radioactive iodine therapy in primary hepatocellular carcinoma
- Associate factors for endoscopic submucosal dissection operation time and postoperative delayed hemorrhage of early gastric cancer
- Effects of postoperative use of proton pump inhibitors on gastrointestinal bleeding after endoscopic variceal treatment during hospitalization
- lmpact of body mass index in elderly patients treated with laparoscopic liver resection for hepatocellular carcinoma
- New perspectives on robotic pancreaticoduodenectomy:An analysis of the National Cancer Database
