Augmentation cystoplasty in children with stages III and IV chronic kidney disease secondary to neurogenic bladder
Sanjay Sinha *,Mehul Shah
a Department of Urology,Apollo Hospitals,Hyderabad,India
b Department of Nephrology,Apollo Hospitals,Hyderabad,India
KEYWORDS Neurogenic bladder;Chronic kidney disease;Augmentation cystoplasty;Vesicoureteric reflux;Urodynamics
Abstract Objective:This study examines the outcome of augmentation cystoplasty(AC)in children with stages III and IV chronic kidney disease(CKD)secondary to neurogenic bladder in which transplantation was not imminent.
1.Introduction
Good renal function has been considered important for handling the additional metabolic load that occurs following incorporation of bowel segment into the urinary tract at augmentation cystoplasty(AC)[1].Unfortunately,we continue to see children with preventable secondary kidney damage due to a delay in institution of therapy for congenital neurogenic bladder.This poses a dilemma since uncorrected bladder storage abnormalities might potentially accelerate kidney damage.
Patients with neurogenic bladder can be at risk for damage to the upper urinary tracts and children with congenital neurogenic bladder due to spina bifida or anorectal malformation are particularly vulnerable[2].Primary goals of therapy include ensuring safe storage and safe emptying function of the lower urinary tract with the avoidance of infection.Safe storage often entails use of antimuscarinics or botulinum toxin injections into the bladder.However,some children especially those with poorly compliant bladders refractory to more conservative measures might require AC.Many children require intermittent catheterization for safe emptying[3].
Few studies have specifically examined the hypothesis that AC can be performed in select children with stages III and IV chronic kidney disease(CKD)[4]secondary to neurogenic bladder although such children can occasionally be found within reported cohorts[5,6].Accordingly,there remains a paucity of evidence.A large study from the United States in patients with spina bifida showed an 8%admission rate for chronic renal failure with an increasing temporal trend and inverse relationship between surgical reconstruction,chiefly AC,and the incidence of chronic renal failure with time[7].
This retrospective study examined the hypothesis that AC can be performed in select children with stages III and IV CKD secondary to neurogenic bladder with preservation of renal function,improved growth,and acceptable morbidity.
2.Methods
Hospital records of all children with CKD stages III and IV who underwent AC between January 2008 and December 2017 were retrieved to study outcomes and complications including kidney function(estimated glomerular filtration rate[eGFR],National Kidney Foundation Calculator)[8],somatic growth(percentiles,compared with population data using the Indian Academy of Pediatrics App[9]),and number of febrile urinary tract infections(fUTIs)requiring admission.Height-independent eGFR estimate was used for one girl with severe kyphoscoliosis[10].Urodynamics data were retrieved for all patients.Bladder capacity was expressed as a percentage of expected bladder capacity for age[11].Expected bladder capacity beyond a capacity of 300 mL was recorded as 300 mL.Compliance was calculated using data points as the final pressure at capacity and the pressure at the start of filling.The detrusor leak point pressure(or end fill pressure in those children who failed to leak)was recorded.
Institutional ethics committee approval was taken(JBH-127/10-15).Descriptive statistics and Mann Whitney U test were calculated using R(ver 3.1.3).
As part of departmental policy,all children presenting with renal dysfunction undergo aggressive conservative management with initial indwelling catheter and subsequent urodynamics-based management with antimuscarinics and clean intermittent catheterization.AC is offered as a last resort typically in those with unresponsive poorly compliant bladders.Regardless of any secondary vesicoureteral reflux,history of fUTIs or sphincteric incompetence,children are not offered ureteric reimplantation or continence procedures at AC.All augmentations are carried out using de-tubularised ileum fashioned into a cup.
3.Results
AC was performed on 79 children with neurogenic bladder of which 13(10 spinal dysraphism and 3 anorectal malformation)were in children with secondary CKD stages III and IV(10 girls;range 3.0-14.9 years;median 8.0 years at surgery).Data on all 13 patients(median follow-up 51 months;inter-quartile range[IQR]47 months)were available for evaluation.On presentation for surgery incontinence episodes were experienced by 10 of the 13 children despite maximum dose of antimuscarinics and intermittent catheterization.Bilateral hydroureteronephrosis was noted in all.Vesicoureteral reflux was recorded in seven children.On urodynamics,median bladder capacity was 74%of expected capacity for age(IQR 36%);median detrusor leak point pressure(or end fill pressure as surrogate)was 40 cmH2O(IQR 19 cmH2O)and median compliance was 5 mL/cm H20(IQR 4 mL/cm H2O).One girl had a vesicostomy 4 years prior to presentation.This was occluded during evaluation.In all patients,the indication for augmentation was upper tract damage with unsafe storage on urodynamics evaluation despite maximum dose of antimuscarinics and clean intermittent catheterization.All patients underwent ileocystoplasty and the median length of bowel used was 25 cm(IQR 5 cm).One had simultaneous nephrectomy and one a mitrofanoff conduit.
There was resolution of incontinence in all children.Age-appropriate bladder capacity as noted on the IC diary record was attained by all patients at last follow-up(median 320 mL;IQR 50 mL).One patient each had a Clavien I(wound infection),III(bladder stone),and IV complication.The latter was an 8-year-old girl who underwent AC with simultaneous appendiceal mitrofanoff(her urethral meatus was recessed)and needed re-hospitalization at 2 weeks for dyselectrolytemia and acute on CKD that resolved.One girl required cystolithotripsy at 4 years.One boy had urethral trauma at 11 months due to IC with a false passage near the verumontanum that healed uneventfully following cystoscopy and a short period of indwelling catheterization.Since this boy was on long-term IC prior to AC,this was not deemed to be a complication of AC.All patients were on long-term alkali supplementation with a satisfactory correction of acidosis.
The median eGFR was 24 mL/min/1.73 m2(IQR 24 mL/min/1.73 m2)at initial presentation to the department,which improved significantly to 52 mL/min/1.73 m2(IQR 12 mL/min/1.73 m2;p=0.004)with conservative management alone.This improved further to 61 mL/min/1.73 m2(IQR 23 mL/min/m2)1 year following AC(p=0.036).No further improvement was noted at any subsequent followup with median eGFRs of 61,57,60,58,68,and 59 mL/min/1.73 m2after 2,3,4,5,6,and 7 years following surgery,respectively(Fig.1).Three children had an eGFR at last follow-up that was numerically below the preoperative eGFR(-1,-4,and-12 mL/min/1.73 m2).Four children were hypertensive at surgery and continued using the same dose of medication at last follow-up.
Somatic growth impairment was noted in a majority of children at presentation for surgery with improvements in most children by the last follow-up(Fig.2).Reduction in hydronephrosis was noted in all.There was a reduction in fUTIs requiring admission from 0.72 per patient-year to 0.04 per patient-year following surgery.
4.Discussion
The concerns regarding risk of complication,metabolic abnormalities,and long-term mortality following AC are heightened in patients with CKD[5,12,13].The precise renal function threshold at which metabolic problems become a problem has never been well established.It has also been suggested that augmentation in a setting of CKD might lead to accelerated kidney damage[14].However,these potential complications must be balanced against the well-established risk to the upper tracts from an unsafe lower urinary tract[2,15,16].
This study shows that AC in select children is safe and leads to modest improvements in renal function and somatic growth.The procedure also prepares the lower urinary tract for a possible future renal transplantation.We believe the acceptable morbidity in our high-risk group was owing to a standardized protocol with short augmentation segment and the avoidance of additional procedures such as continence surgery,mitrofanoff conduit,or ureteric reimplantation.
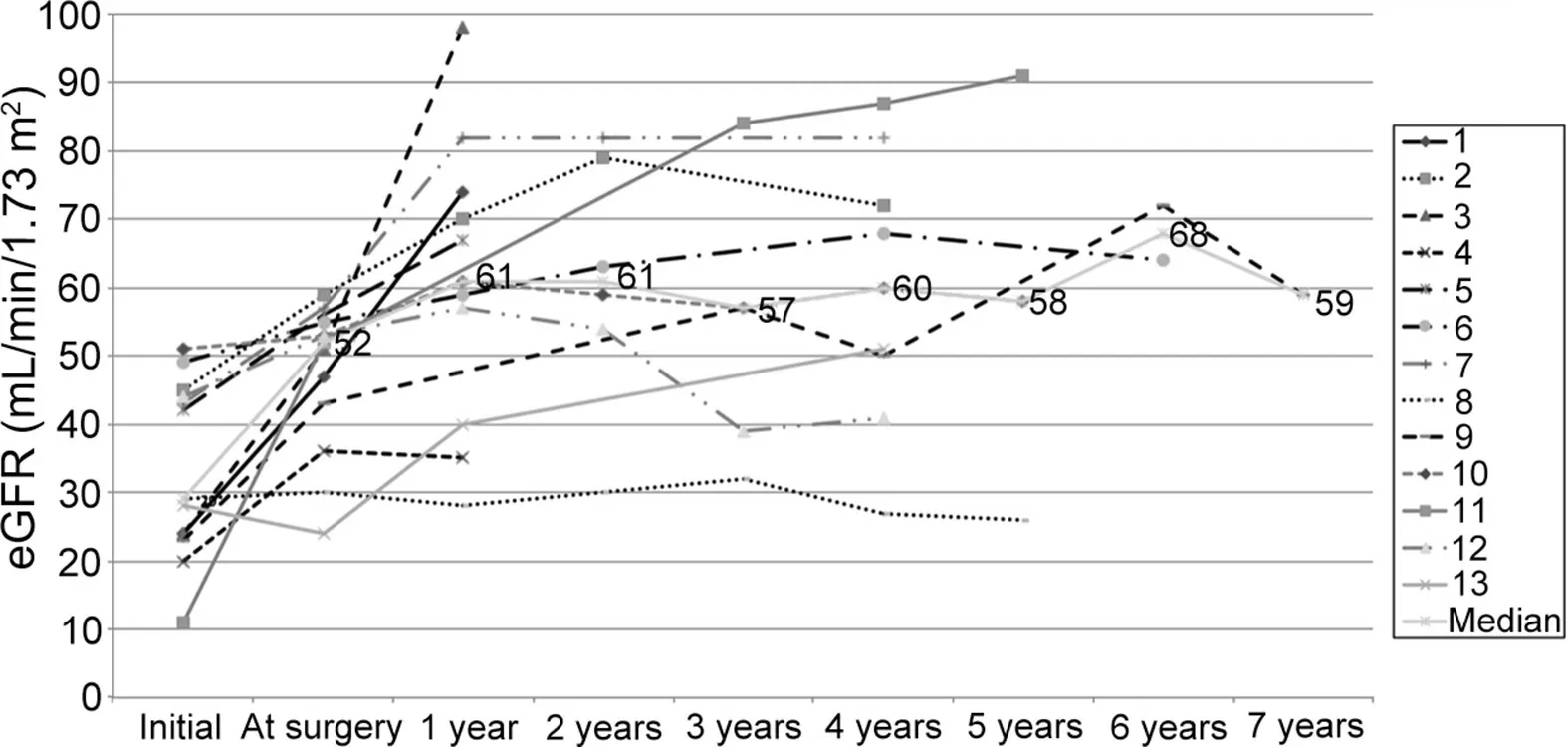
Figure 1 eGFR estimates for each of the 13 patients along with the median eGFR line.Initial eGFR is that noted at first presentation to the department.Estimates were made using the National Kidney Foundation Calculator.eGFR,estimated glomerular filtration rate.
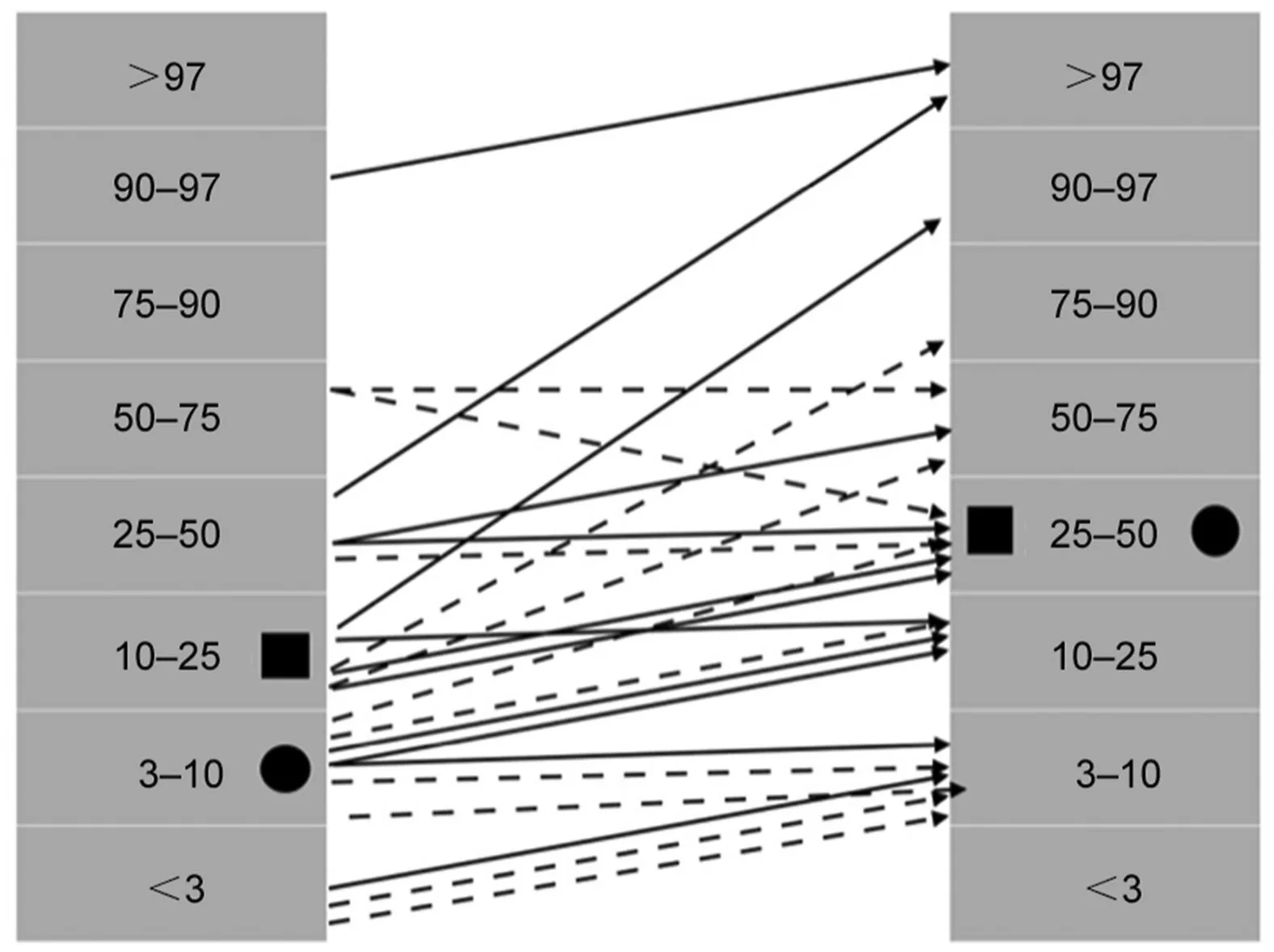
Figure 2 Height(solid arrows;black square)and weight(broken arrows;black circle)before and at last follow-up after augmentation cystoplasty.Preoperative values are depicted to the left.Percentiles class is based on population data from the Indian Academy of Pediatrics Calculator.The black square and circle depict median values for height and weight respectively.
Our patients were able to handle the metabolic challenges of AC with a short 25 cm length of ileum.Patients became continent and upper tract changes showed resolution.Although these patients had unsafe bladders,the capacity might not always be low.Our patients had a median compliance of 5 cmH2O but a median capacity equivalent to 74% of expected capacity for age.Consequently,a long length of bowel might neither be necessary nor desirable in most of these patients.
Deferring continence surgery has several advantages.First,as we have shown,not all patients need a continence procedure.Deferring the continence procedure allows the patient to“earn”the surgery.All our patients became socially dry.Possibly poor compliance that endangered the upper tracts was a marker for a relatively robust sphincter mechanism in this select group.Second,it reduces the extent of surgical reconstruction.Third,it avoids the potential handling bowel and prosthetic material in the same reconstruction reducing the risk of contamination.Others have also reported that AC is often sufficient irrespective of preoperative continence status[17].
We did not re-implant any of the ureters regardless of reflux.Other authors have recommended routine reimplantation[18]or consideration in case of severe reflux[3].However,reflux has been found to improve or resolve in most patients following AC alone[19].It appears that managing intravesical pressures is sufficient for managing secondary reflux[20].None of our patients underwent reimplantation and while we did not perform formal reassessment for postoperative reflux or bladder pressures,the sharp reduction in fUTIs and improvement in the upper urinary tract appears to support the validity of this approach.Routine urodynamics may not be necessary unless there is progressive upper tract dilatation or unresolved incontinence,which we did not encounter[21].
Renal function showed modest improvements at 1 year.These small gains in renal function can confer significant long-term benefit.In another series of eleven patients with a mean eGFR of 34 mL/min/1.73 m2undergoing AC,renal function stabilized in all but one at a mean follow-up of 1.9 years[4].It has been suggested that patients with aneGFR under 50 mL/min/1.73 m2are more likely to deteriorate[22].Ultimately,all patients with established CKD are likely to show decline in renal function owing to the natural history of disease.A long-term study found decline in GFR of 18 mL/min for patients with congenital disease and 34 mL/min in those with acquired lower urinary tract dysfunction undergoing augmentation[23].The authors speculated that younger age at augmentation might have conferred an advantage on the congenital group.
The reason for modest improvement in renal function early after AC is uncertain.It is conceivable that AC is more effective at reducing intravesical pressure than indwelling catheters or antimuscarinics in patients with unsafe storage.The assumption that indwelling catheters are universally effective at lowering intravesical pressures has been questioned[24].In the long-term,patients with CKD can be expected to have a progressive loss of renal function as a part of their natural history of disease.This natural history is likely to assert itself;the longer these patients are followed up.Additionally,eGFR estimates based on serum creatinine and height have limitations when applied to patients with atypical body morphology such as some children with spina bifida[25,26].Abnormally low muscle mass and height that are common in children with spina bifida confound eGFR measurement.Several approaches have been used to circumvent this problem including estimates based on cystatin-C,arm span length,or sitting height,These are not commonly in use and there is need for a universal global standard[26].
Alternative forms of augmentation suggested for patients with CKD are gastrocystoplasty and ureterocystoplasty.Although the gastric segment has a lower theoretical propensity for causing metabolic abnormalities,progressive renal insufficiency has been noted[6].Ureterocystoplasty,which is contingent on the availability of a grossly dilated non-functioning renal unit is prone to underaugmentation[27].
Our patients showed an encouraging improvement in somatic growth with catch up in height and weight.However,despite this they remained behind their age-matched peers.Timely augmentation at a young age might be important.In a series of 42 patients(which included nonneurogenic diagnoses)height and weight did not improve despite improvements in renal function possibly because the children were older[28].
This study shows that patients with CKD secondary to neurogenic bladder often benefit from aggressive urodynamics-based conservative management even when they present late.Initial renal function was more than doubled with conservative management alone.In fact,an important message from this work might be that it is never too late to attempt conservative therapy with an indwelling catheter followed by aggressive bladder management.
Bladder capacity is not a reliable surrogate for safety in this patient population.Several of our patients had“adequate”or normal bladder capacity.However,intravesical pressures were dangerously high.Other authors have also reported deceptively“adequate”bladder capacity.In one series of adults undergoing AC,the median preoperative cystometric capacity was 240 mL with a quarter of patients having capacity above 385 mL[29].Safe intravesical pressure is crucial to the upper urinary tract.Data suggest that long-term storage pressures of over 20 cmH2O could be associated with renal damage[30].Further,in patients with neurogenic bladder,capacity and pressure estimates can be confounded by the presence of reflux or bladder diverticuli.While high intravesical storage pressures are clearly unsafe,low pressures cannot be assumed to indicate safety.Safety in these patients must be surmised from a range of clinical and urodynamic data and not by any one parameter alone.
Our study has significant limitations besides the small number of patients studied.We did not routinely perform postoperative urodynamics or evaluation for reflux.There was no comparator group of patients who underwent reimplantation.In the context of the young age of these patients,follow-up is short and is unlikely to capture remote complications and long-term functional deterioration.
5.Conclusion
This study shows that AC can be carried out with acceptable morbidity in children with CKD stages III and IV secondary to neurogenic bladder.Surgery is effective with improvements in continence,renal function,somatic growth,and propensity for fUTIs.Ureteric re-implantation might not be necessary.
Author contributions
Study design:Sanjay Sinha,Mehul Shah.
Data acquisition:Sanjay Sinha.
Data analysis:Sanjay Sinha.
Drafting of manuscript:Sanjay Sinha,Mehul Shah.
Critical revision of the manuscript:Sanjay Sinha,Mehul Shah.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年3期
Asian Journal of Urology2022年3期
- Asian Journal of Urology的其它文章
- Burned-out testicular seminoma with retroperitoneal metastasis and contralateral sertoli cell-only syndrome
- Endoscopic management of adolescent closed Cowper’s gland syringocele with holmium:YAG laser
- Transcutaneous dorsal penile nerve stimulation for the treatment of premature ejaculation:A novel technique
- Bilateral calcified Macroplastique? after 12 years
- Culture-positive urinary tract infection following micturating cystourethrogram in children
- A phase II study of neoadjuvant chemotherapy followed by organ preservation in patients with muscle-invasive bladder cancer
