Association between clustering of cardiovascular risk factors and resting heart rate in Chinese population: a cross-sectional study
Fu-Yu JING, Xiu-Ling WANG, Jia-Li SONG, Yan GAO, Jian-Lan CUI, Wei XU, Yang YANG,Li-Juan SONG, Hai-Bo ZHANG, Jia-Peng LU, Xi LI, Xin ZHENG,2,?
1. National Clinical Research Center for Cardiovascular Diseases, NHC Key Laboratory of Clinical Research for Cardiovascular Medications, State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, National Center for Cardiovascular Diseases, Beijing, China; 2. National Clinical Research Center for Cardiovascular Diseases, Shenzhen, Coronary Artery Disease Center, Fuwai Hospital Chinese Academy of Medical Sciences, Shenzhen, China
ABSTRACT
Over the past several years, the rapid development of smart wrist-worn devices has resulted in a convenient approach to monitoring resting heart rate (RHR) in daily life. RHR is becoming a promising indicator of cardiovascular health. Observational studies have shown that elevated RHR is associated with increased all-cause and cardiovascular mortality in populations with or without cardiovascular disease (CVD).[1,2]Elevated RHR has also been found to be associated with cardiovascular risk factors (CVRFs), such as hypertension, diabetes mellitus, dyslipidemia, low physical activity and smoking, indicating its potential to reflect total cardiac risk.[3-7]There is abundant epidemiologic evidence supporting the association between a single CVRF and RHR, but studies exploring associations between multiple CVRFs and RHR are limited.
CVRFs tend to cluster within individuals, and several weak risk factors combined may result in a much higher risk than that due to a single strong risk factor.According to a cross-sectional survey in China, more than 45% of Chinese adults have two or more coexisting CVRFs.[8]Thus, it is important to consider the situation of multiple CVRFs clustering. However,very few studies have analyzed the association between CVRFs clustering and RHR, and several aspects remain unknown. Firstly, prior studies mainly focused on the relation between metabolic risk factors and RHR.[9-11]Behavioral risk factors such as smoking, physical activity and alcohol use have rarely been considered, even though these risk factors also have a significant effect on heart rate.[3,5,7]Secondly, most studies merely dealt with the relation of CVRFs clustering number with RHR, while regarding each number of risk factors, different combinations of risk factors have not yet been considered before.[9,12]It is important to consider different CVRF clustering patterns since some risk factors combined may lead to a higher risk of elevated RHR than others, even if the number of CVRFs is the same. Thirdly, prior studies did not assess associations stratified by sex and age. It has been well documented that RHR levels differ by sex and age. The RHR in women was on average 2-7 beats/min higher than that in men, and there was a decrease in the RHR with age.[13,14]As such,whether the associations of CVRFs clustering with RHR varied between sex and age remains unclear.Taking advantage of the large sample size in our study, we are able to include a wider range of CVRFs(metabolic and behavioral risk factors), comprehensively evaluate the association between these CVRFs clustering and RHR, and further explore sex and age differences. This finding may inform us whether RHR can be used as a simple and efficient metric for the identification of high-risk individuals who require more intensive risk factor evaluation and earlier cardiovascular health monitoring in resource-constrained countries with substantial CVD burdens, such as China.
To bridge this knowledge gap, we used data from the China PEACE Million Persons Projects, a nationwide screening project, to explore (1) the association between the number of CVRFs clustering and elevated RHR in the overall population and populations stratified by age and sex; and (2) the associations between different CVRFs clusters and the risk of elevated RHR in the overall population and populations stratified by sex.
METHODS
Study Design and Participants
The China PEACE Million Persons Projects is a government-funded public health screening program designed to focus on CVD risk throughout China.[15]In brief, from September 2015 to August 2020, a total of 294 sites in 31 provinces in mainland China were selected to provide diversity in geographic distribution, socioeconomic status, and exposure to risk factors and diseases. Participants aged 35-75 years who had lived in the region for at least six months of the preceding twelve months were invited by local staff from primary health care institutions or via extensive media campaigns. Among the 3.7 million people screened in the China PEACE Million Persons Projects, participants with serial project identification numbers ending with 1, 3, 5, or 7 were selected to provide detailed information about CVRFs, and these participants were included in our study (Figure 1).We excluded those receiving heart rate-lowering drugs (including beta-blockers, calcium channel blockers and ivabradine), those with a history of CVD or other major chronic diseases (including cancer and chronic obstructive pulmonary disease), and those with missing data regarding age, sex, heart rate, blood pressure(BP), body mass index (BMI), lipid profile, smoking status, alcohol use, physical activity, education status,and annual household income. The Central Ethics Committee of Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing, China approved this project. All enrolled participants provided written informed consent.
Data Collection and Variables
BP, RHR, height, weight, and serum lipid were measured with standardized devices and procedures for each participant. BP was measured twice on the right upper arm after 5 min of rest in a seated position with a standardized electronic BP monitor (Omron HEM-7430). If the difference between two systolic BP readings was greater than 10 mmHg, a third measurement was obtained, and the average of the last two readings was used. Heart rate readings were also collected using the electronic BP monitor, and the mean value of the two readings was calculated as RHR. BMI was defined as weight in kilograms divided by height in square meters. In addition, trained personnel conducted standardized in-person interviews to collect information about sociodemographic status (ethnicity, education level, occupation, annual household income, and medical insurance status), lifestyle (smoking, alcohol use, and physical activity), medical history, and medication use.
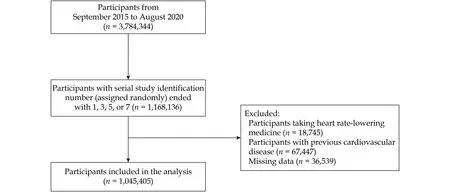
Figure 1 Participant flow diagram.
We focused on seven CVRFs in our study: hypertension, diabetes mellitus, obesity, dyslipidemia,smoking, alcohol use, and low physical activity. Hypertension was defined as a systolic BP of 140 mmHg or higher, a diastolic BP of 90 mmHg or higher, antihypertensive medication use, or a self-reported history of hypertension according to Chinese guidelines.[16]Diabetes mellitus was defined as a self-reported history of diabetes mellitus or current treatment with antidiabetic medication. Obesity was defined as a BMI ≥ 28.0 kg/m2based on the working group’s recommendation on obesity in China.[17]Dyslipidemia was defined as a self-reported history of lipid disorder, current treatment with cholesterollowering medication or the presence of one or more of the following: total cholesterol ≥ 5.2 mmol/L, triglyceride ≥ 1.7 mmol/L, high-density lipoprotein cholesterol < 1.0 mmol/L, or low-density lipoprotein cholesterol ≥ 3.4 mmol/L.[18]Participants who reported their frequency of smoking as ranging from“occasionally” to “daily” in the questionnaire were classified as smoking. Participants who consumed alcohol more than four times per week and more than“one unit or two units” during a typical day were defined as alcohol use. We added up the hours of varied sports per day spent on leisure time for calculating physical activity level. Low physical activity was defined as less than 150 min of moderate activity or less than 75 min of vigorous activity per week.[19]Metabolic risk factors included hypertension, diabetes mellitus, dyslipidemia and obesity. Behavioral risk factors included smoking, alcohol use and low physical activity. According to prior studies and expert consensus, the study outcome was elevated RHR,defined as RHR > 80 beats/min.[20-24]
Statistical Analysis
Characteristics of the study participants were described by the CVRFs clustering number. Continuous variables were presented as mean ± SD, and categorical variables were presented as counts (percentages). Differences between groups were tested using Kruskal-Wallis tests for continuous data and Mantel-Haenszel chi-squared tests for categorical data.
The odds ratios (OR) for elevated RHR association with CVRFs clustering numbers were calculated using multivariate logistic regression analysis in total population and different sex (male, female) and age(35-44 years, 45-54 years, 55-64 years, 65-75 years)subgroups. We adjusted for age (except in age-stratified model), gender (except in gender-stratified model), education status, and annual household income in all models.[25]We used the Cochran-Armitage trend test to assess the trend of elevated RHR across CVRFs clustering number groups.
To investigate the associations between different CVRF clusters and elevated RHR, we created 128 CVRF clusters, covering all possible combinations of the seven CVRFs included in our study; we excluded 49 clusters with less than 500 participants. Finally, we retained 79 clusters, each comprising at least 500 participants. The ORs for elevated RHR associated with different CVRFs clusters were calculated using multivariate logistic regression analysis. We further explored the association by sex. However, we did not further explore the associations by age due to limited numbers of participants, because this would lead to a large number of subgroups with very few people to analyze, even in a study as large as ours. In all the statistical models, we adjusted for age,gender (except in the gender-stratified model), education status, and annual household income.
AllP-values were two-sided, andP-value < 0.05 was considered statistically significant. All analyses were carried out using SAS 9.4 (SAS Institute, Cary,NC, USA).
RESULTS
Characteristics of the Study Population
Of 1,168,136 enrolled participants, 18,745 participants were excluded due to heart rate-lowering drug use, 67,447 participants were excluded due to previous CVD or major chronic disease, and 36,539 participants were excluded due to missing data (Figure 1).Among the remaining 1,045,405 participants, 631,459 participants (60.4%) were women, and the mean age was 55.67 ± 9.86 years. Characteristics of these participants were shown by the number of risk factors(Table 1).
Overall, 4.4% of the participants did not have any of the seven CVRFs. By comparison, 23.8%, 33.1%,24.9%, 10.8%, and 3.1% of the participants had 1, 2,3, 4, and ≥ 5 risk factors, respectively. At the same time, we also summarize the distribution of CVRFs clustering number by sex and age (supplemental material, Figure 1S).
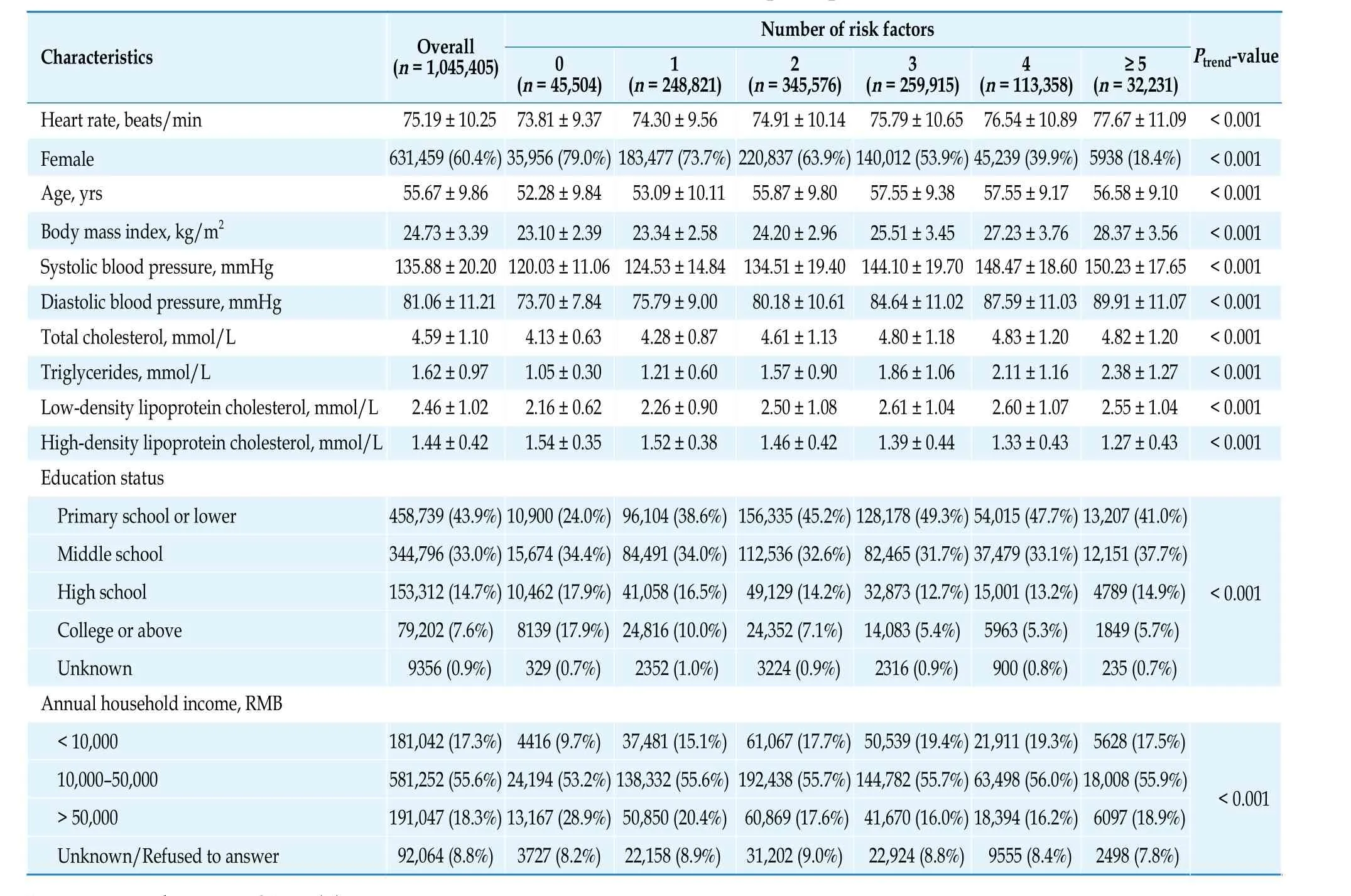
Table 1 Baseline characteristics of participants.
Association Between CVRFs Clustering Number and Elevated RHR
The risk of elevated RHR increased with the number of CVRFs clustering (Figure 2). In the multivariate-adjusted analysis, the OR for the 1, 2, 3, 4, and ≥5 risk factors relative to the group with no risk factors ranged from 1.10 (95% CI: 1.08-1.13) to 2.58 (95% CI:2.50-2.67), independent of age, sex, education status and annual household income (Ptrend< 0.001).
The relation between CVRFs clustering number and elevated RHR differed by sex and age (Table 2).The risk of elevated RHR was more strongly influenced by the CVRFs clustering number in the younger age group than in the elderly age group (Pinteraction<0.001), especially when ≥ 5 risk factors were combined; the OR was 3.59 (95% CI: 3.31-3.90) in the group aged 35-44 years and 1.85 (1.71-2.01) in the group aged ≥ 65 years. The effect of CVRFs clustering number on the risk of elevated RHR was more pronounced in males than in females (Pinteraction< 0.001).The associations were similar in the sex-age subgroups (Table 3), and the risk of elevated RHR was the most strongly influenced by the CVRFs clustering number in the young male group.
Association Between Different CVRFs Clusters and Elevated RHR
Among the 79 clusters of CVRFs, the OR for an elevated RHR relative to the no risk factor group varied across different clusters, even though the number of CVRFs was the same (Figure 3). Metabolic risk factors contributed most to the risk of elevated RHR.In the group with only one CVRF, “Diabetes mellitus” was associated with the highest risk of elevated RHR (OR = 1.82, 95% CI: 1.65-2.00), followed by “Hypertension” (OR = 1.52, 95% CI: 1.47-1.57) and “Dyslipidemia” (OR = 1.11, 95% CI: 1.07-1.14), while “Obesity” and “Alcohol use” were not significantly associated with elevated RHR. When multiple risk factors were combined, clusters comprising more metabolic risk factors were associated with a higher risk of an elevated RHR than clusters comprising more behavioral risk factors. For example, the ORs for an elevated RHR were 2.42 (95% CI: 2.29-2.53) in the cluster with three metabolic risk factors (Hypertension-Diabetes mellitus-Dyslipidemia), 1.86 (95% CI:1.81-1.91) in the cluster with two metabolic risk factors plus one behavioral risk factor (Hypertension-Dyslipidemia-Low physical activity), and 1.13 (95%CI: 1.06-1.20) in the cluster with three behavioral risk factors (Smoking-Low physical activity-Alcohol use).This associations between clusters with elevated RHR were similar in men and women (supplemental material, Figures 2S & 3S).
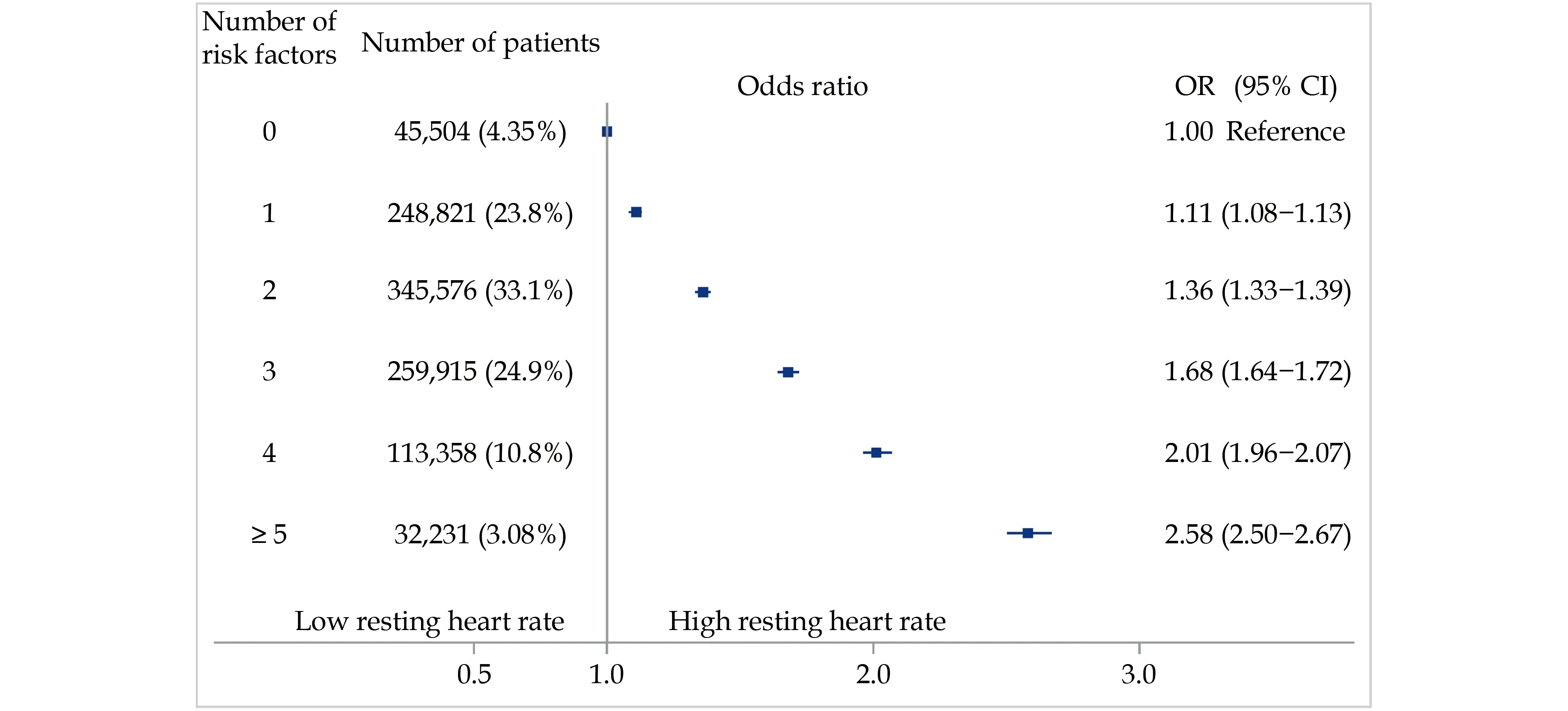
Figure 2 Association between the number of risk factors and elevated resting heart rate. The model was adjusted for age, sex, income, and education. OR: odds ratios.
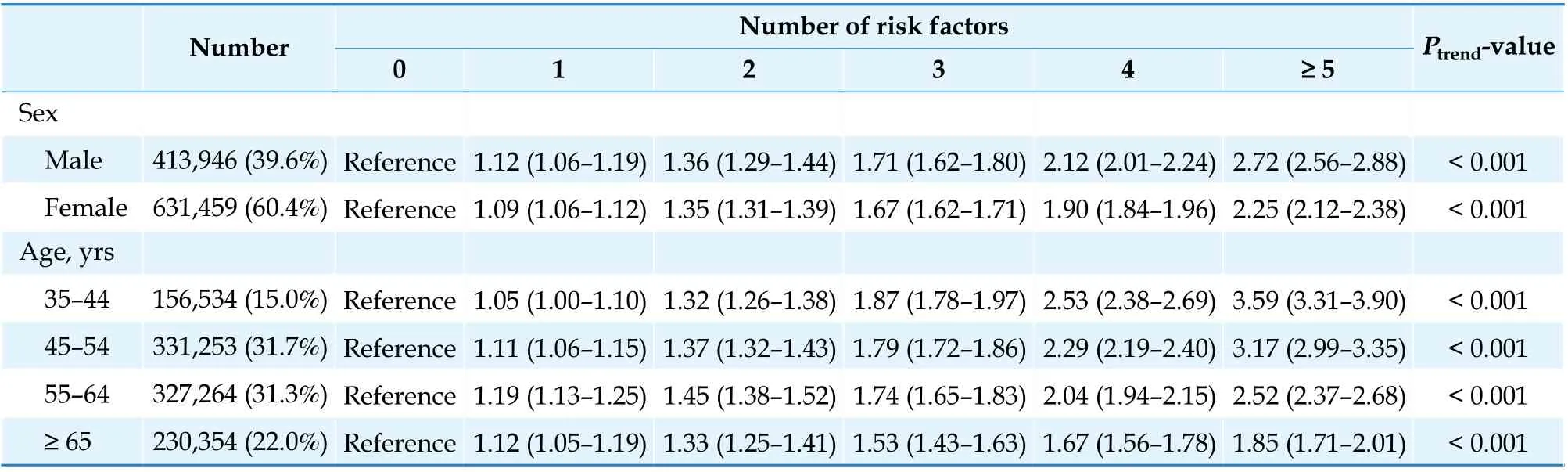
Table 2 Association between the number of risk factors and elevated resting heart rate by sex and age.

Table 3 Association between the number of risk factors and elevated resting heart rate in gender-age subgroups.
DISCUSSION
This study demonstrated that the risk of elevated RHR increased remarkably with an increasing number of CVRFs, and the association was much more pronounced in young men. Clusters comprising more metabolic risk factors had a stronger association with elevated RHR than clusters comprising more behavioral risk factors. These findings highlight the valuable use of RHR, a simple clinical measure, which may help the early detection of cardiovascular risk to identify high-risk individuals among relatively healthy population.
To our knowledge, this is the first comprehensive assessment of the associations between CVRFs clustering and elevated RHR across a wide variety of subgroups. Prior studies have reported a positive association between the metabolic risk factor number and the risk of elevated RHR.[9,11]In addition to confirming this finding, our study extends the existing literature with a wider range of CVRFs, including behavioral risk factors, which have rarely been considered previously. The novel finding in our study is that clusters comprising more metabolic risk factors were associated with a higher risk of elevated RHR than those comprising more behavioral risk factors.This is consistent with previous studies, supporting the close connection between metabolic risk factors and elevated heart rate. Elevated heart rate is a common feature among individuals with metabolic risk factors, such as hypertension, diabetes mellitus and metabolic syndrome.[23,26]Moreover, a higher heart rate is predictive of new-onset hypertension, diabetes mellitus, obesity or metabolic syndrome.[24,27,28]Besides, prior studies demonstrated that the relations of behavioral risk factors with RHR were generally weaker than those of hypertension and diabetes mellitus with RHR, which is in line with our findings.[4,6,9]Our observation further extends this finding in the context of CVRF clustering, the association between several behavioral risk factors combined and the risk of elevated RHR was much weaker than that between several metabolic risk factors combined and elevated RHR. Thus, more emphasis should be placed on modifying metabolic risk factors,which can markedly reduce the risk of an elevated RHR and may further reduce the risk of cardiovascular outcomes. However, behavioral risk factors may induce long-term sympathetic overactivity, increasing the heart rate over time. Therefore, promoting a healthy lifestyle should not be neglected in the general population.
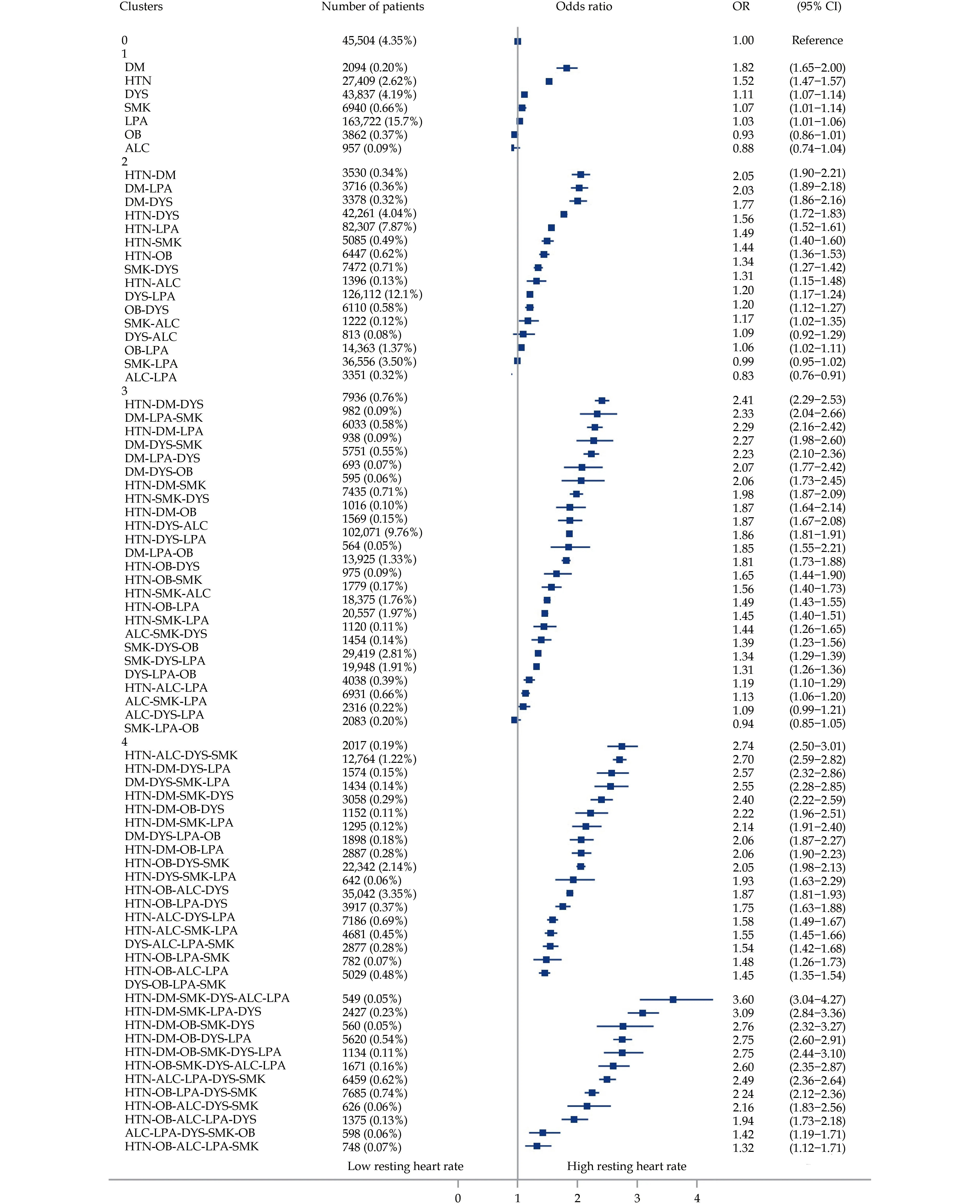
Figure 3 Association between the clusters of risk factors and elevated resting heart rate. The models were adjusted for age, sex, income and education. ALC: alcohol use; DM: diabetes mellitus; DYS: dyslipidemia; HTN: hypertension; LPA: low physical activity; OB:obesity; OR: odds ratios; SMK: smoking.
The relationship between obesity and elevated RHR was quite weak in our study. This observation was consistent with the findings of prior studies suggesting no or a minor influence of BMI on the RHR.[11,24]A possible mechanism is that sympathetic outflow to the heart is reduced in obese people with normotension, which explains why heart rates can remain normal in obese patients.[29]In contrast, cardiac sympathetic outflow is increased in obesity-related hypertension, resulting in a higher RHR. In our study,the differential risk of an elevated RHR between the two clusters partially supported this theory; the “Hypertension-Obesity” cluster was associated with a significantly higher risk of an elevated RHR than the “Obesity” cluster. Sympathetic activity becomes complicated when obesity is accompanied by other CVRFs,and the mechanism is not well understood. Further exploration of sympathetic tone in population of obesity and other concomitant CVRFs is needed.
In the age- and sex-stratified analyses, we found that the association of CVRFs clustering number with elevated RHR was more prominent in men aged 35-45 years than in the other sex-age subgroups. Prior studies in adolescents also showed such sex differences, but studies in adults are scarce.[12]The possible mechanism for the sex and age differences is that the increased RHR in men primarily reflects a heightened sympathetic tone related to the existence of risk factors. However, modest elevation of RHR would merely the normal situation in women,which is not represent sympathetic overactivity.[30]Moreover, fibrosis of the sinus node with increasing age decreases responsiveness to sympathetic overactivity, resulting in a decrease in the RHR with age.[31]This explains the remarkable increase in the trend of the association between elevated RHR and an increased CVRFs number in younger adults (aged 35-44 years) and the gradual increase in the trend in the elderly subgroup (≥ 65 years). Therefore, it might be reasonable to use RHR to assess the risk of multiple CVRFs in the younger male population, particularly in those aged 35-44 years.
Our findings have important clinical implications.Over the past several years, the rapid development of smart wrist-worn devices in the field of medical health has offered a convenient approach to monitoring heart rate in daily life.[32]Heart rate is becoming a promising parameter to provide more clinical information for cardiac health with the development of wearable technology. Our study demonstrated that an elevated RHR was related to the number and pattern of risk factors clustering. RHR would be a feasible clinical parameter for the identification of highrisk individuals who require more intensive risk factor evaluation and earlier intervention regarding their cardiovascular health.
LIMITATIONS
Our study should be interpreted in the context of several limitations. Firstly, as in other large-scale studies, some risk factors, including physical activities, tobacco smoking, and alcohol use, were collected through self-reports, which might have been influenced by recall bias and social desirability. Secondly, the study cohort was not established on the basis of a random sampling design, so it does not represent the entire Chinese population. However, this limitation may have little influence on our findings because we focused on the associations rather than the prevalence of risk factors. Thirdly, participants were invited to the screening center during the daytime.Although the impact of circadian rhythm might be minor, we cannot entirely eliminate its effect. Last but not least, due to the cross-sectional design, we were unable to infer the causality of the associations between CVRFs clustering and RHR.
CONCLUSIONS
In conclusion, there was a markedly positive association between the CVRF number and the risk of elevated RHR, particularly in young males. Moreover,clusters comprising more metabolic risk factors were associated with a higher risk of elevated RHR than those comprising more behavioral risk factors. These findings indicate that the RHR reflects the number and pattern of multiple risk factors clustering. As a simple clinical measure, RHR may help identify individuals who require further risk factor evaluation,particularly in primary healthcare settings with limited resources.
ACKNOWLEDGMENTS
This study was supported by the National Key Research and Development Program from the Ministry of Science and Technology of China (2018YFC1311 205). All authors had no conflicts of interest to disclose. The authors thank the contributions that have been made by the China PEACE Million Persons Projects group at the Chinese National Center for Cardiovascular Diseases, and the local sites in the collaborative network in the realms of study design and operations, particularly data collection by Bo GU, Xi LI,Chao-Qun WU, Hao DAI, Hui ZHONG, and Ming-Hui ZHANG.
 Journal of Geriatric Cardiology2022年6期
Journal of Geriatric Cardiology2022年6期
- Journal of Geriatric Cardiology的其它文章
- Transplant-associated thrombotic microangiopathy: a rare but deadly complication post orthotopic heart transplantation
- Prognostic significance of multiple triglycerides-derived metabolic indices in patients with acute coronary syndrome
- Establishment of a diagnostic model of coronary heart disease in elderly patients with diabetes mellitus based on machine learning algorithms
- Simultaneous interventional therapy for coarctation of the aorta combined with intracristal ventricular septal defect in older age adult
- Acute myocardial infarction complicated with takotsubo syndrome in an elderly patient: case report and literature review
- Normalizing the dementia status in cardiovascular diseases:a perspective
