Serum-negative Sjogren's syndrome with minimal lesion nephropathy as the initial presentation: A case report
lNTRODUCTlON
Primary Sjogren's syndrome (pSS) is a chronic autoimmune disease that is characterized by the lymphocytic infiltration of exocrine glands, resulting in the significant loss of the secretory function and the development of inflammatory and destructive lesions in the salivary glands and lacrimal glands. The most common clinical manifestations are dryness in the mouth and eyes. Extraglandular involvement may also occur, including in the kidneys (3%-5%); The main renal lesions are the infiltration of inflammatory cells into the renal tubules and interstitium, and the glomerular involvement often manifests as the development of a membranous nephropathy[1]. Herein, We report a case of Sjogren's syndrome with micropathic nephropathy as the primary presentation, and this patient was negative for anti-SSA and anti-SSB antibodies and had no symptoms of exocrine gland involvement.
Again and again he had crept to the hut, and finding some choice morsel2 put away for the little hare, had either eaten it if he thought it nice, or trampled3 it to pieces so that no one else should get it, and at last the peasant lost patience, and made up his mind he would have the Tanuki s blood
CASE PRESENTATlON
Chief complaints
A 43-year-old female patient was admitted due to recurrent systemic oedema for 5 months.
History of present illness
The patient’s lower oedema appeared five months prior to presentation, and the oedema was obvious at night and disappeared in the morning. Then, the patient’s oedema of the extremities worsened and had extended to the face, and this was accompanied by oliguria (approximately 500-800 mL/day) and the presence of foamy urine. The patient did not have a dry mouth, and the patient had no need to consume water with the ingestion of dry food, did not have dry eyes, and had flaky tooth loss, parotid gland enlargement, joint pain, hair loss, light allergy, or oral ulcers.
History of past illness
The prior history of the patient was nonspecific.
The authors declare that they have no conflicts of interest to disclose.
Personal and family history
The patient was given intravenous prednisolone (PSL) 40 mg/d for one week. The patient was discharged from the hospital on December 09, 2020. Then the patient was prescribed prednisone 40 mg/d po.
Physical examination
Kidney involvement is an important extraglandular complication of pSS and can lead to chronic kidney disease and even death. At present, it is not clear the renal involvement in patients with pSS is caused by the SS disease itself or if it coexists with other diseases. Bossini[8] and Tu[9] reported that some pSS-related renal diseases may occur before the subjective symptoms of dry mouth/eyes and joint pain. In a previous report, renal biopsies were obtained from 103 pSS patients who had renal involvement complications in order to investigate the renal pathological types. Among these types, renal tubule and interstitial involvement was the main pathological type, which was identified in 53 of the patients (51.5%), and glomerulonephritis (GN) was the main pathological type in the other 50 patients (48.5%). The pathological types of the GN lesions included membranous nephropathy (37, 35.9%), membranoproliferative glomerulonephritis (6, 5.8%), IgA nephropathy (3, 2.9%), minimal change disease (4, 3.9%), and focal segmental glomerulosclerosis (3, 2.9%). Compared with pSS patients without complications, the patients who had pSS complications, especially renal involvement, developed atypical dry mouth and dry eyes (< 0.05)[10]. In addition, the incidence of interstitial lung disease, leukopenia and elevated IgG levels were significantly lower (< 0.05) in the pSS patients who had complications[5]. A number of previous studies that have evaluated the pathological characteristics of renal biopsy samples have also showed that tubulointerstitial nephritis (TIN) is the main pathological type of renal involvement in pSS patients. The pathophysiology of acute and chronic TIN involves the infiltration of T cells, B cells, and plasma cells (among other cell types) into the renal interstitium and renal tubules, which promotes interstitial fibrosis and can lead to CKD[11-14]. In SS patients, glomerular involvement is far less common than renal tubulointerstitial involvement, which may manifest as haematuria, proteinuria or even nephrotic syndrome. The deposition of circulating immune complexes in the glomerulus and the triggering of mesangial proliferation and extracellular matrix protein synthesis are considered to be key factors in the development of glomerular diseases[8]. The pathogenesis of renal involvement in pSS is unclear. Studies have been conducted to identify the factors that are associated with the renal involvement of pSS. A meta-analysis showed that the presence of anti-SSB antibodies was closely associated with arthralgia and the renal injury secondary to pSS and concluded that the presence of SSB antibodies was positively correlated with the development of renal involvement[15]. The most common glomerular disease associated with SS is membranous proliferative glomerulonephritis (MPGN), which is associated with the activation of polyclonal B lymphocytes and can cause cryoglobulinemia, and MPGN is the second most common renal manifestation in pSS[16,17]. Many studies have reported that steroids and immunosuppressants (such as cyclophosphamide, plasma exchange therapy, rituximab, azathioprine or mycophenolate) in the treatment of MPGN can significantly improve the renal function in patients with CKD[18]. Magalianalysed 95 SS patients who had renal involvement confirmed by renal biopsy and found that TIN occurred in 93 of the SS nephritis patients (97.9%) and that glomerular lesions occurred in 22 patients (23.2%). Eighty-one patients (85.3%) received treatment, of whom 80 were treated with CSs (98.8%) and 21 were treated with immunosuppressants (primarily rituximab) (25.9%). Although significant interstitial fibrosis was found in the initial biopsy samples, the renal function of the patients improved significantly within 12 months after diagnosis (final eGFR 49.9 and 39 mL/min/1.73 mfor those treated with CSs and immunosuppressants, respectively; the baseline eGFR was 8 mL/min/1.73 m,< 0.001). In this study, no additional benefit was found when using immunosuppressant therapy compared to steroid therapy alone[1].
28. Crumb17: Note that just as bread provides life sustaining sustenance85, the children are now depending on it to save their lives beyond it s true purpose.
In a flash I knew -- she had made it for her mother, a mother she would never see again, a mother who would never hold her or brush her hair or share a funny story, a mother who would never again hear her childish joys or sorrows
Laboratory examinations
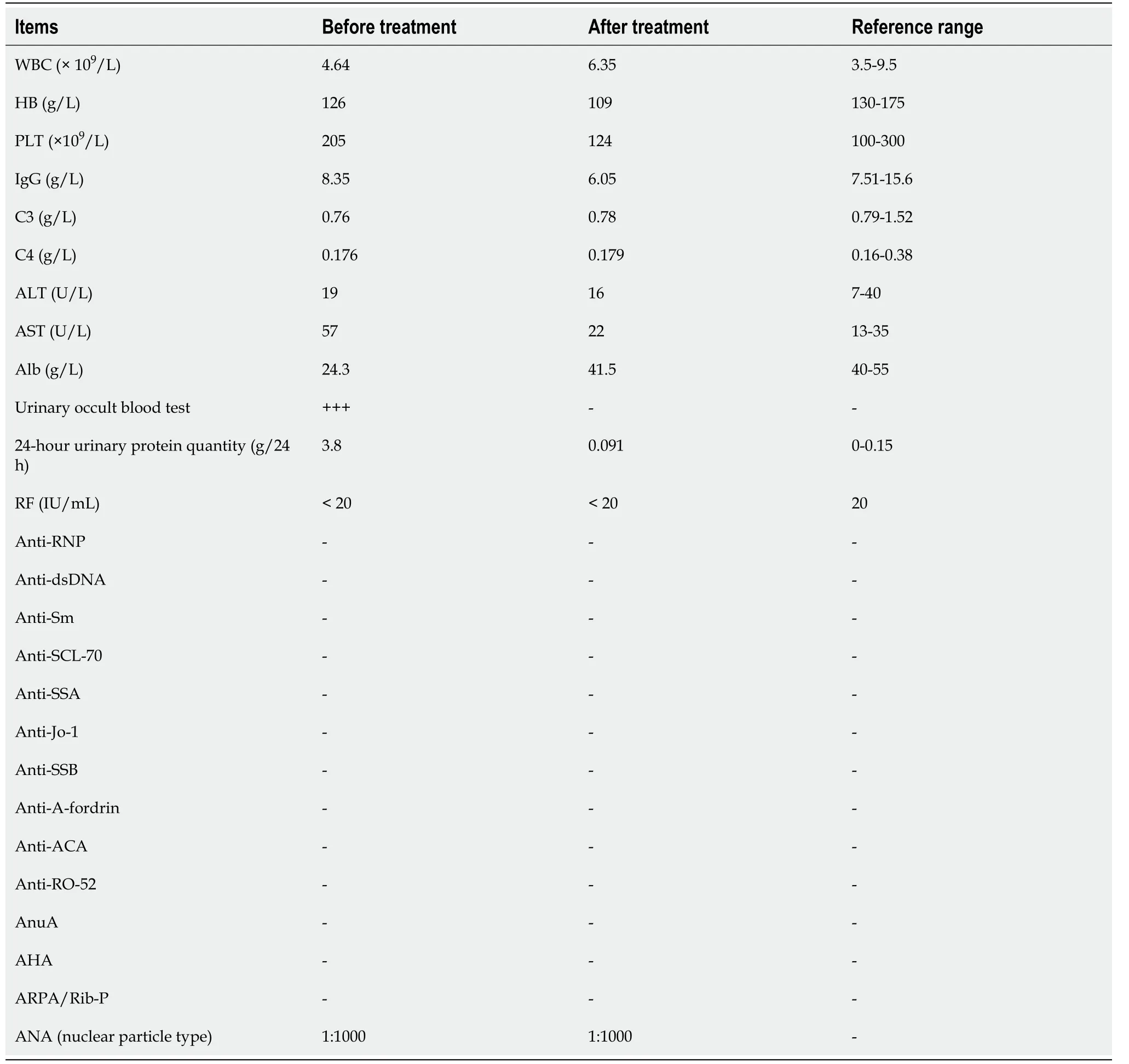
The results of the patient’s laboratory examinations are shown in Table 1.
Imaging examinations
Cases of Serum antibody-negative Sjogren's syndrome, where there are no symptoms of exocrine gland involvement and no hyperglobulinemia, where kidney is the first manifestation and where renal pathology is seen as minimal lesion nephropathy, are clinically rare. Therefore, the case analysis here aims to remind clinicians to consider the possibility of pSS in patients with a high titre positive antinuclear antibody combined with the presence of interstitial inflammatory cell focal aggregation in the kidney, even if the patients do not have the typical serological changes. MSGB plays an important role in the diagnosis of atypical pSS.

FlNAL DlAGNOSlS
The maiden50 did as he told her, and then the wolf breathed over the flowery grave, and, lo and behold51! the Prince lay there sleeping as peacefully as a child
TREATMENT
The patient’s personal and family history was nonspecific.
OUTCOME AND FOLLOW-UP
After 3 weeks of treatment, the patient’s systemic oedema had disappeared. A re-examination of the routine urine test revealed the following: urinary protein (-), serum albumin: 41.9 g/L, and urinary protein quantitation: 0.091 g/24 h (Table 1). Therefore, the treatment was effective.
And as she drank thus, and leaned right over the water, the rag containing the three drops of blood fell from her bosom12 and floated down the stream, and she in her anxiety never even noticed her loss.21 But the waiting-maid had observed it with delight, as she knew it gave her power over the bride, for in losing the drops of blood the Princess had become weak and powerless.22 When she wished to get on her horse Falada again, the waiting- maid called out: I mean to ride Falada: you must mount my beast ; and this too she had to submit to. Then the waiting-maid commanded her harshly to take off her royal robes, and to put on her common ones,23 and finally she made her swear by heaven not to say a word about the matter24 when they reached the palace; and if she hadn t taken this oath she would have been killed on the spot. But Falada observed everything, and laid it all to heart.
DlSCUSSlON
Currently, there is no gold standard for diagnosing pSS. The diagnosis of pSS has been based on the presence of typical clinical symptoms such as dry mouth, dry eyes, the results of the minor salivary gland biopsy (MSGB) and autoantibodies the presence of autoantibodies. According to the 2016 ACR/EULAR pSS classification criteria, the following are used for a diagnosis: (1) Focal lymph infiltration of labial glands with a focal index ≥ 1 Lesion /4 mm); and (2) A filter paper test (Schirmer test ≤ 5mm/5 min); pSS is diagnosed when the total score is ≥ 4[2]. The final diagnosis in this patient was pSS with nephrotic syndrome. Li[3] summarized 161 pSS patients and found that only 86 patients (53.42%) were positive for both anti-SSA and anti-SSB antibodies. Another study found that 37 (35.6%) of 104 pSS patients were negative for both anti-SSA and anti-SSB antibodies[4]. This suggests that pSS cases with negative anti-SSA and SSB antibodies are common in the clinic. Serologically negative SS-A and SS-B antibodies were more common in patients with late-onset pSS (age > 35 years) than in patients with early-onset pSS who had significant clinical manifestations and enhanced cellular immune system activation[5]. According to the classification, the patient in this case report had a late-onset, therefore, MSGB should be considered if pSS is suspected in the patients without the typical pSS symptoms or without the presence of the specific autoantibodies[6]. The value of MSGS is important in the pSS diagnosis. In addition, the detection of autoantibodies in this patient indicated a high titer positive anti-ANA antibody titre, indicating the possibility of an autoimmune diseases, and a positive anti-ANA titre is important for the diagnosis and differentiation of rheumatoid diseases. However, it should be noted that a positive ANA test is also common in healthy individuals[7].
What I remember most about those weddings is that all the girls were at least five years older than I was, and they all had beautiful eyes that sparkled when they laughed. Those weddings taught me to imagine what it would be like to find my soul mate one day and to be sure that I would know her by her beautiful eyes.
The physical examination showed that the patient had oedema in her lower extremities, which was not specific.
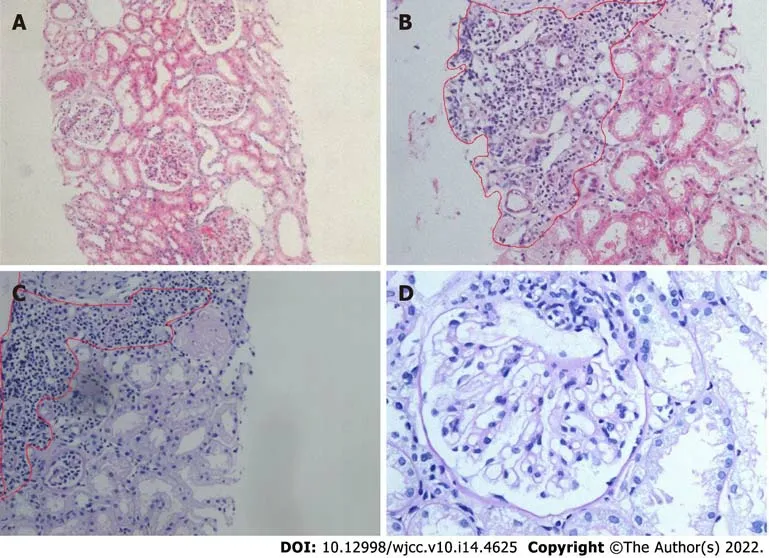
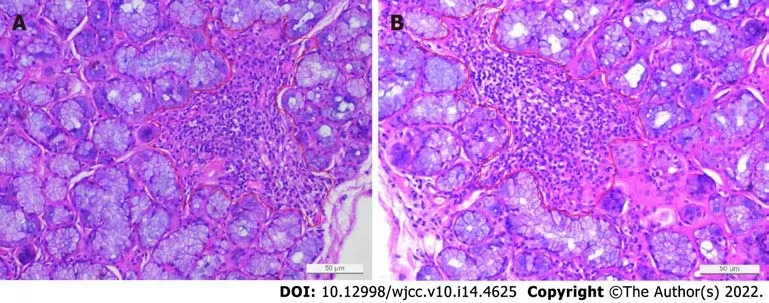
In this case, renal tubular atrophy and interstitial fibrosis were occasionally observed in the samples under light microscopy. Interstitial inflammatory cell focal aggregation is a common pathological manifestation of the renal damage in pSS patients. In addition, pathological manifestations similar to lupus nephritis combined with secondary membranous nephropathy can be seen in pSS patients. Also, several immune complex deposits can be seen in the mesangial glomerulus and capillary walls, but this was not the case in this patient[19]. On the basis of these findings and the patient's clinical manifestations and laboratory examination results, atypical lupus nephritis was excluded. The electron microscopic analysis of the kidney biopsy samples from this patient revealed diffuse foot process effacement, and the patient was diagnosed with minimal lesion nephropathy.
CONCLUSlON
The patient underwent a renal biopsy on December 1, 2020 under ultrasonography guidance to assess the etiology of the nephrotic syndrome. The light microscopic analysis of the kidney biopsy samples identified thirteen glomeruli, and no abnormalities were observed. Tubular atrophy, interstitial fibrosis, focal vacuolar degeneration in the tubular epithelial cells, and focal aggregation of interstitial inflammatory cells were occasionally present (Figure 1). An immunofluorescence analysis of the kidney biopsy sample revealed that the kidney samples were negative for IgG, IgM, IgA, C1q and C3. An electron microscopic analysis of the kidney biopsy sample revealed that there was a diffuse effacement of the foot processes. Electron-dense deposits were not observed (Figure 2). An ophthalmic examination revealed a Schirmer test score of 3 mm/5 min and a tear breakup time of 4 s. An analysis of a labial gland biopsy sample analysis identified the presence of level IV lesions (Figure 3).
FOOTNOTES
Li CY and Li YM wrote the manuscript; all authors have given final approval to the version to be submitted.
The final diagnosis was pSS with nephrotic syndrome.
Informed written consent was obtained from the patient for publication of this case report in accordance with institutional guidelines.
So she learnt by this how the evil spell might be broken, and she carefully sprinkled every stone till there was not one left--only a great company of youths and girls who followed her down the mountain
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Chun-Yan Li 0000-0003-0510-782X; Yi-Man Li 0000-0003-4081-2487; Mei Tian 0000-0002-1633-2988.
Ma YJ
A
Ma YJ
 World Journal of Clinical Cases2022年14期
World Journal of Clinical Cases2022年14期
- World Journal of Clinical Cases的其它文章
- Perfectionism and mental health problems: Limitations and directions for future research
- Ovarian growing teratoma syndrome with multiple metastases in the abdominal cavity and liver: A case report
- Development of plasma cell dyscrasias in a patient with chronic myeloid leukemia: A case report
- Suprasellar cistern tuberculoma presenting as unilateral ocular motility disorder and ptosis: A case report
- Rare pattern of Maisonneuve fracture: A case report
- PD-1 inhibitor in combination with fruquintinib therapy for initial unresectable colorectal cancer: A case report
