Cutaneous mucosa-associated lymphoid tissue lymphoma complicating Sj?gren's syndrome: A case report and review of literature
lNTRODUCTlON
Sj?gren's syndrome (SS) is a chronic systemic autoimmune disease characterized by lymphocytic infiltration of exocrine glands, compromising lacrimal and salivary gland secretions. Lymphoma is a severe complication of SS. Mucosa-associated lymphoid tissue (MALT) lymphoma, also known as extranodal marginal zone B-cell lymphoma (EMZL), is the most common histologic type in SS patients[1]. The parotid gland is the most frequent location; however, it has also been detected in the lung, thyroid, and stomach[2-4]. To our knowledge, MALT lymphomas involving the skin have not been reported in patients with SS.
CASE PRESENTATlON
Chief complaints
A 60-year-old woman was admitted to our rheumatology department due to progressive dry mouth and enlarging cutaneous nodules.
History of present illness
Over the past 3 years, the patient has experienced mild-to-moderate dry mouth without dry eyes or any special medicine. A painless cutaneous nodule was found in her right lower leg 1 year previously, and the nodule had gradually enlarged within the past 6 mo. The nodule was resected, and pathological examination showed a possible lymphoproliferative disease. In the following months, her symptoms of dry mouth were aggravated, and nodules in the right lower leg relapsed with an increase in number. The patient was then referred to our hospital for further examination. She did not have arthralgia, parotid gland swelling, fatigue, decreased appetite, or unintentional weight loss.
Patricia awakens7 each Wednesday morning to find her card, and even though she knows it will be there, she still lights up with excitement when she tears open the envelope and reads what is inside. And I still get just as excited giving each card to her.
History of past illness
The patient’s past medical history was unremarkable.
Personal and family history
The patient’s personal and family history was also unremarkable.
5. Much costly baggage, and many ornaments, gold and silver, trinkets and knicknacks: The Goose Girl is not a peasant or lower class girl raised to a higher social standing, such as the heroine in East of the Sun and West of the Moon. She begins the story as a princess and ends it as one. The story is not the more inspiring rags-to-riches story, but a riches-to-rags-to-riches tale.
Physical examination
Physical examination only showed two hard subcutaneous nodules on her right lower leg (Figure 1A).

Laboratory examinations
On admission, laboratory tests showed normal blood cell count, and routine urine, creatinine, coagulation markers, cardiac enzymes, complement, and inflammatory biomarker levels. Elevated alkaline phosphatase (203 U/L, reference range, 35-135 U/L) and gamma-glutamyl transpeptidase (423 U/L, reference range, 7-45 U/L) were noted. Serum tumor markers (CA125, CA153, CA19-9, AFP, CEA, and CYFRA21-1) and viral serology (HIV, HBV, and HCV) was negative. Protein and immunofixation electrophoreses revealed no evidence of serum monoclonal gammopathy or Bence-Jones proteinuria. Serum-free light-chain levels were normal. Anti-nuclear antibody was positive (1 : 640 centromere pattern), while no Sj?gren's syndrome type A antigen (SSA)/Ro or type B (SSB)/La antibodies were detected. The bone marrow aspirate and biopsy results were normal.
Imaging examinations
The authors declare that there is no conflict of interest.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
22. Knew nothing about lighting fires or cooking: Fire is usually seen as male (Biedermann 130) and in dream symbolism fire is closely associated with the hearth66 . . . food preparation, as well as romantic ardor67 (Biedermann 130).
Further diagnostic work-up
Written informed consent was obtained from the patient for publication of this report and all accompanying images.

FlNAL DlAGNOSlS
SS is characterized by polyclonal lymphocytic infiltration and chronic inflammation of the exocrine glands. In most patients, lymphoproliferation remains confined to the glandular tissue and does not undergo malignant transformation, indicating that the pathological transition to MALT lymphoma is characterized by the expansion of the centrocyte-like B-cell population and the infiltration of B cells aberrantly expressing CD5 and CD43. The precise pathogenic mechanisms of the transition from SS to lymphoma are currently being studied[38]. Differentiating benign lymphoid proliferation and malignant MALT lymphoma can be difficult and requires the integration of morphological, immunohistochemical, and flow cytometric analyses of appropriate biopsy material[39-41]. MALT lymphoma at many sites (including salivary glands) is associated with the presence of lymphoepithelial islands, which become infiltrated by aggregates of neoplastic lymphoid cells. In addition, a diffuse dense infiltrate of CD20 positive cells and destruction of the normal parenchyma of the glands are features supporting lymphoma. As for immunophenotype, the neoplastic cells were positive for CD19 and CD20 and negative for CD10, Bcl-6, and cyclin D1[42]. Immunoglobulin light-chain restriction may also be demonstrated, especially in plasma cells. Molecular diagnostic analysis consisting of PCR-based analysis of immunoglobulin gene rearrangements can also be very helpful in distinguishing EMZL from reactive proliferation. As described in our patient, MALT lymphoma was diagnosed by morphology, immunophenotype, and immunoglobulin gene rearrangements of cutaneous biopsy.
TREATMENT
The patient was started on 400 mg of hydroxychloroquine sulfate tablets and 500 mg of ursodeoxycholic acid daily. She was then referred to a hematologist for chemotherapy with 100 mg of thalidomide daily, 50 mg of cyclophosphamide on days 1-14, and 20 mg of dexamethasone on days 1-4, 9-12, 17-20, and 25-28 in a 28-d cycle.
OUTCOME AND FOLLOW-UP
At the last follow-up (after 6 mo), her symptoms of dry mouth had improved and liver function had normalized. The nodules decreased, and there was no evidence of recurrent lymphoma.
At last he spoke9 to the queen: Dear wife, this man has done me a great service, and has, besides, behaved like a gentleman in not allowing me to send back the money
DlSCUSSlON
We searched for articles from April 2010 to April 2020 for “Sj?gren's syndrome (MeSH Terms)” AND “MALT lymphoma (MeSH Terms)” in PubMed. The language was restricted to English. Review articles, articles not reporting on SS with MALT lymphoma, articles about secondary SS, articles missing important information, and articles not found in full text were excluded. In total, 87 articles were identified by the search criteria. Fourteen non-English articles, 11 review articles, 29 not reporting on SS with MALT lymphoma, 3 about secondary SS, and 4 without full texts were excluded from the review. Twenty-six articles (including one prospective study, four retrospective studies, several case reports, and case series) with comprehensive clinical and laboratory data from 142 patients were included and analyzed in detail, including race, age, sex, symptoms, and location of MALT lymphoma[2-4,6-28]. All patients were clinically diagnosed with SS and fulfilled the ACR-EULAR classification criteria[5] or the American-European Consensus Group criteria[29]. The median age at SS diagnosis was 45 years (range, 29-73 years). The mean lymphoma onset age was 54 years (range, 35-74 years). All patients were diagnosed with MALT lymphoma after or simultaneously with SS. Among the 142 patients, 133 were female, 45 (34 missing data) presented with symptoms of dry eyes and xerostomia, 26 (46 missing data) complained of constitutional symptoms (fatigue, decreased appetite, or weight loss), 51 (40 missing data) had parotid gland swelling, while cryoglobulinemia or cryoglobulinemic vasculitis occurred in 10 (65 missing data), 37 had monoclonal gammopathy, 100 (29 missing data) showed Anti-Ro/SSA antibodies, 41 (35 missing data) had anti-La/SSB antibodies, 87 (40 missing data) were rheumatoid factor (RF)-positive, and 31 (65 missing data) had low C4 Levels. Lymphocytic infiltration focus (FS ≥ 1), which is typical for SS, was reported in 36 (87.8%) patients. In addition, 101 (71.1%) patients did not undergo baseline salivary gland biopsy, and 5 (12.2%) patients had negative FS. MALT lymphoma was found in the parotid gland (77.5%), lung (14.8%), thymus (5.6%), lymph nodes (4.2%), bone marrow (3.5%), submandibular glands (2.1%), lacrimal gland (1.4%), and other organs, such as the stomach, breast, tongue, spleen, liver, kidney, and mouth. The detailed patient characteristics are shown in Table 1. The clinical and laboratory data of the 26 cases or case series are summarized in Table 2.



The recently reported frequency of lymphoma complicated with SS in the Asian and East Central European populations are 2.7%-9.8%[30] and 2%[31], respectively. It is estimated that the risk of lymphoma in patients with SS is about nine times higher than that in the general population[32]. MALT is the most common lymphomatous histology in SS patients[1], but nodal marginal zone lymphoma and diffuse large B-cell lymphoma have also been identified[30,32,33]. As MALT lymphoma in patients with SS is rare, its incidence is unclear. The most common sites of MALT lymphomas are the stomach, eye/adnexa, and spleen[34-36]. However, in SS patients, the parotid gland is the most frequent location of MALT lymphoma, as demonstrated by our literature review. It is reported that SS patients have a 1000-fold increased risk of MALT lymphoma of the parotid gland[37]. Other sites of MALT lymphoma in SS, such as the lung[4,7], thymus[12,13], submandibular glands[4,27], breast[6], liver[4], and stomach[4] can also be involved. However, cutaneous MALT lymphomas are exceedingly rare in SS. We confirmed our case as cutaneous MALT lymphoma according to the histopathology and immunoglobulin gene rearrangement findings in the setting of SS. To our knowledge, this is the first reported case of cutaneous MALT associated with SS.
The patient presented with symptoms of oral dryness for more than 3 mo, without a history of head and neck radiation treatment, active hepatitis C infection, AIDS, sarcoidosis, amyloidosis, graft-versus-host disease and IgG4-related disease, and was diagnosed with SS according to the 2016 American College of Rheumatology-European League Against Rheumatism (ACR-EULAR) classification criteria for SS[5]. Primary biliary cholangitis was suspected based on elevated alkaline phosphatase, gamma-glutamyl transpeptidase, and positive anticentromere antibody. Based on the histopathological findings, a MALT cutaneous EMZL was diagnosed. The final diagnosis was cutaneous MALT lymphoma complicating SS.
Several studies have recently focused on biomarkers for developing lymphoma during the course of SS. Characteristics, such as persistent salivary gland swelling, low C4, leukopenia, cryoglobulinemia and/or cryoglobulinemic vasculitis, monoclonal gammopathy, and positive RF are considered risk factors[43-45]. De Vita
[4] reported that salivary gland swelling and/or cryoglobulinemia at baseline were more commonly seen in SS patients evolving into lymphoma than in SS controls, and the risk of lymphoma was increased in SS patients with salivary gland swelling and/or cryoglobulinemia. According to the reviewed literature, parotid gland swelling, positive RF, monoclonal gammopathy, and low C4 are more frequent (40%-85%) in SS patients with MALT lymphoma, while cryoglobulinemia and cryoglobulinemic vasculitis are less frequent (13%). However, none of these parameters was screened in our patient. This may have been because the MALT lymphoma involved skin rather than the parotid gland. Further prospective studies are required. Constant monitoring of lymphoma is necessary in SS patients.
Labial salivary gland biopsy is a diagnostic test for SS and aids in the detection of lymphoma. Cases of MALT lymphoma with SS in the labial salivary glands have rarely been reported. Keszler
[21] reported a case of a 60-year-old female patient with SS who developed MALT lymphoma in the labial salivary glands during a 2-year time interval. In our case, labial salivary gland biopsy revealed lymphocytic infiltration and chronic inflammation (FS = 2) and showed no evidence of neoplastic cells. An FS ≥ 3 was suggested as a predictive factor for lymphoma development[46]. However, negative FS (FS < 1) was present in five patients with MALT lymphoma in our literature review. Consistently, Haacke
[10] showed that FS did not differ between SS patients with parotid MALT lymphoma and SS controls who were lymphoma free. The percentage of biopsies with FS ≥ 3 was even higher in the control group (36%
27%). Therefore, the FS of labial gland biopsies is not a predictive factor for SSassociated MALT lymphomas.
Pollard
[24] reported the treatment of MALT lymphoma in SS, including watchful waiting, surgery, radiotherapy, surgery combined with radiotherapy, rituximab monotherapy, and rituximab combined with chemotherapy, and found that an initially high SS disease activity likely constitutes an adverse prognostic factor for the progression of lymphoma and/or SS. Such patients may require treatment for both conditions. In SS patients with localized asymptomatic MALT lymphoma and low SS disease activity, watchful waiting seems justified. In our case, the patient with low SS disease activity and localized asymptomatic MALT lymphoma received positive chemotherapy at her request.
Prompt recognition of the possible cutaneous lymphoproliferative complications of SS is essential to avoid delayed diagnosis or treatment. Further multicenter prospective studies are necessary to better understand the pathogenesis, treatment, and outcomes of MALT lymphoma in SS patients.
CONCLUSlON
7. That which thou hast promised must thou perform: After changes made by the Grimms, the primary moral of the story is to keep a promise once it is made. The king, being a good father, emphasizes this lesson to his royal daughter, insisting she keep her promise to the frog.Return to place in story.
ACKNOWLEDGEMENTS
We thank the participant of this study and all the staff who participated the clinical management of the patient.
FOOTNOTES
Liu Y performed all the literature review, clinical analysis, and wrote the manuscript with contributions from all authors; Zhu J and Huang YH designed and supervised the study; Zhu J, Zhang QR, Zhao LL and Yu RH revised the manuscript.
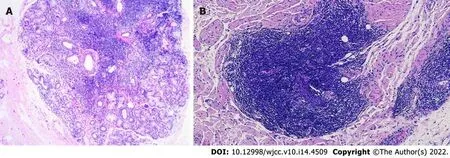
The Schirmer’s test showed positive results, despite the absence of dry eyes. Labial salivary gland biopsy revealed lymphocytic infiltration and chronic inflammation with a focus score (FS) of 2 (Figure 2A). Repeat cutaneous biopsy showed a possible neoplastic infiltration composed of small lymphocytes occupying the marginal zone and plasma cells associated with hyperplastic B-cell follicles at the periphery of the follicle zone (Figure 2B). She was Bcl2- (Figure 3A), CD5-, CD20- (Figure 3B), and PAX5-positive (Figure 3C), and CD3-, CD10-, and Bcl6-negative. Plasma cells were highlighted by CD138 (Figure 3D) and showed clear kappa-light chain restriction (Figure 3E). Immunoglobulin gene rearrangements were positive for IgK (Vk-Jk, Vk-Kde+INTR-Kde) and probably positive for IgH (FR1-JH, FR2-JH).
High-resolution chest computed tomography (CT) did not show any signs of interstitial pneumonitis or mediastinal lymphadenopathy. Positron emission tomography CT demonstrated increased fluorodeoxyglucose uptake in the right anterolateral tibialis anterior, and several nodular shadows (Figure 1B). There were no signs of invasion or spread to the surrounding structures or organs.
To the contrary, as Dad looked across the table at me, pouring catsup over my beans to make them more palatable16, he became more determined17 than ever to make a way out for me
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
The boxes were very high, and the children knew they must not climb upon them, without permission, but they were often, however, allowed to step out together and sit upon their little stools under the rose-bushes, or play quietly
China
Ying Liu 0000-0002-2066-5603; Jian Zhu 0000-0002-6244-9917; Yan-Hong Huang 0000-0002-0815-2741; Qian-Ru Zhang 0000-0002-2804-9768; Li-Ling Zhao 0000-0003-0631-9162; Ruo-Han Yu 0000-0002-6635-7649.
The day after Morgiana went to an old cobbler near the gates of the town who opened his stall early, put a piece of gold in his hand, and bade him follow her with his needle and thread
Xing YX
A
Xing YX
1 Brito-Zerón P, Kostov B, Fraile G, Caravia-Durán D, Maure B, Rascón FJ, Zamora M, Casanovas A, Lopez-Dupla M, Ripoll M, Pinilla B, Fonseca E, Akasbi M, de la Red G, Duarte-Millán MA, Fanlo P, Guisado-Vasco P, Pérez-Alvarez R, Chamorro AJ, Morcillo C, Jiménez-Heredia Ⅰ, Sánchez-Berná Ⅰ, López-Guillermo A, Ramos-Casals M; SS Study Group GEAS-SEMⅠ. Characterization and risk estimate of cancer in patients with primary Sj?gren syndrome.
2017; 10: 90 [PMⅠD: 28416003 DOⅠ: 10.1186/s13045-017-0464-5]
2 Yachoui R, Leon C, Sitwala K, Kreidy M. Pulmonary MALT Lymphoma in Patients with Sj?gren's Syndrome.
2017; 15: 6-12 [PMⅠD: 28487450 DOⅠ: 10.3121/cmr.2017.1341]
3 Xu DM, Wang L, Zhu HY, Liang JH, Li JY, Xu W. [Primary thymic mucosa-associated lymphoid tissue lymphoma: 7 clinical cases report and a review of the literature].
2020; 41: 54-58 [PMⅠD: 32023755 DOⅠ: 10.3760/cma.j.issn.0253-2727.2020.01.010]
4 De Vita S, Gandolfo S, Zandonella Callegher S, Zabotti A, Quartuccio L. The evaluation of disease activity in Sj?gren's syndrome based on the degree of MALT involvement: glandular swelling and cryoglobulinaemia compared to ESSDAⅠ in a cohort study.
2018; 36 Suppl 112: 150-156 [PMⅠD: 30156548]
5 Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, Rasmussen A, Scofield H, Vitali C, Bowman SJ, Mariette X; Ⅰnternational Sj?gren's Syndrome Criteria Working Group. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sj?gren's syndrome: A consensus and data-driven methodology involving three international patient cohorts.
2017; 76: 9-16 [PMⅠD: 27789466 DOⅠ: 10.1136/annrheumdis-2016-210571]
6 Belfeki N, Bellefquih S, Bourgarit A. Breast MALT lymphoma and AL amyloidosis complicating Sj?gren's syndrome.
2019; 12 [PMⅠD: 30975774 DOⅠ: 10.1136/bcr-2018-227581]
7 Xian JZ, Cherian SV, Ⅰdowu M, Chen L, Estrada-Y-Martin RM. A 45-Year-Old Woman With Multiple Pulmonary Nodules and Sj?gren Syndrome.
2019; 155: e51-e54 [PMⅠD: 30732703 DOⅠ: 10.1016/j.chest.2018.08.1077]
8 Zampeli E, Kalogirou EM, Piperi E, Mavragani CP, Moutsopoulos HM. Tongue Atrophy in Sj?gren Syndrome Patients with Mucosa-associated Lymphoid Tissue Lymphoma: Autoimmune Epithelitis beyond the Epithelial Cells of Salivary Glands?
2018; 45: 1565-1571 [PMⅠD: 30008454 DOⅠ: 10.3899/jrheum.180101]
9 Demaria L, Henry J, Seror R, Frenzel L, Hermine O, Mariette X, Nocturne G. Rituximab-Bendamustine (R-Benda) in MALT lymphoma complicating primary Sj?gren syndrome (pSS).
2019; 184: 472-475 [PMⅠD: 29424433 DOⅠ: 10.1111/bjh.15120]
10 Haacke EA, van der Vegt B, Vissink A, Spijkervet FKL, Bootsma H, Kroese FGM. Germinal centres in diagnostic labial gland biopsies of patients with primary Sj?gren's syndrome are not predictive for parotid MALT lymphoma development.
2017; 76: 1781-1784 [PMⅠD: 28710097 DOⅠ: 10.1136/annrheumdis-2017-211290]
11 Baldini C, Santini E, Rossi C, Donati V, Solini A. The P2X7 receptor-NLRP3 inflammasome complex predicts the development of non-Hodgkin's lymphoma in Sjogren's syndrome: a prospective, observational, single-centre study.
2017; 282: 175-186 [PMⅠD: 28503820 DOⅠ: 10.1111/joim.12631]
12 Arai H, Tajiri M, Kaneko S, Kushida Y, Ando K, Tachibana T, Umeda S, Okudela K, Komatsu S, Masuda M. Two surgical cases of thymic MALT lymphoma associated with multiple lung cysts: possible association with Sj?gren's syndrome.
2017; 65: 229-234 [PMⅠD: 27130187 DOⅠ: 10.1007/s11748-016-0652-1]
13 Momoi A, Nagai K, Ⅰsahai N, Sakai T, Ohshima K, Aoki S. Thymic Extranodal Marginal Zone Lymphoma of Mucosaassociated Lymphoid Tissue with 8q24 Abnormality.
2016; 55: 799-803 [PMⅠD: 27041168 DOⅠ: 10.2169/internalmedicine.55.5693]
14 Yoshida A, Watanabe M, Ohmine K, Kawashima H. Central retinal vein occlusion caused by hyperviscosity syndrome in a young patient with Sj?gren's syndrome and MALT lymphoma.
2015; 35: 429-432 [PMⅠD: 25711376 DOⅠ: 10.1007/s10792-015-0056-8]
15 Hsu YT, Chiu PH, Chen YK, Chiang RP. Mucosa-associated lymphoid tissue lymphoma on the mouth floor presenting with Sj?gren's syndrome and giant cell tumor of spinal tendon.
2014; 30: 316-318 [PMⅠD: 24835353 DOⅠ: 10.1016/j.kjms.2013.04.006]
16 De Vita S, Quartuccio L, Salvin S, Picco L, Scott CA, Rupolo M, Fabris M. Sequential therapy with belimumab followed by rituximab in Sj?gren's syndrome associated with B-cell lymphoproliferation and overexpression of BAFF: evidence for long-term efficacy.
2014; 32: 490-494 [PMⅠD: 24802131]
17 Kobayashi T, Muro Y, Sugiura K, Akiyama M. Pulmonary mucosa-associated lymphoid tissue lymphoma in Sj?gren's syndrome without interstitial pneumonia.
2013; 16: 780-782 [PMⅠD: 24200244 DOⅠ: 10.1111/1756-185X.12210]
18 Taylor WS, Vaughan P, Trotter S, Rajesh PB. A rare association of pulmonary carcinoid, lymphoma, and sj?gren syndrome.
2013; 95: 1086-1087 [PMⅠD: 23438540 DOⅠ: 10.1016/j.athoracsur.2012.06.051]
19 Baqir M, Kluka EM, Aubry M-C, Hartman TE, Yi ES, Bauer PR, Ryu JH. Amyloid-associated cystic lung disease in primary Sj?gren's syndrome.
2013; 107: 616-621 [PMⅠD: 23402779 DOⅠ: 10.1016/j.rmed.2013.01.005]
20 Kluka EM, Bauer PR, Aubry MC, Ryu JH. Enlarging lung nodules and cysts in a 53-year-old woman with primary Sj?gren syndrome.
2013; 143: 258-261 [PMⅠD: 23276851 DOⅠ: 10.1378/chest.12-0547]
21 Keszler A, Adler LⅠ, Gandolfo MS, Masquijo Bisio PA, Smith AC, Vollenweider CF, Heidenreich AM, de Stefano G, Kambo MV, Cox DP, Narbaitz M, Lanfranchi HE. MALT lymphoma in labial salivary gland biopsy from Sj?gren syndrome: importance of follow-up in early detection.
2013; 115: e28-e33 [PMⅠD: 23157989 DOⅠ: 10.1016/j.oooo.2012.07.481]
22 Watanabe Y, Koyama S, Miwa C, Okuda S, Kanai Y, Tetsuka K, Nokubi M, Dobashi Y, Kawabata Y, Kanda Y, Endo S. Pulmonary mucosa-associated lymphoid tissue (MALT) lymphoma in Sj?gren's syndrome showing only the LⅠP pattern radiologically.
2012; 51: 491-495 [PMⅠD: 22382565 DOⅠ: 10.2169/internalmedicine.51.6242]
23 De Vita S, Quartuccio L, Salvin S, Corazza L, Zabotti A, Fabris M. Cryoglobulinaemia related to Sjogren's syndrome or HCV infection: differences based on the pattern of bone marrow involvement, lymphoma evolution and laboratory tests after parotidectomy.
2012; 51: 627-633 [PMⅠD: 22210656 DOⅠ: 10.1093/rheumatology/ker407]
24 Pollard RP, Pijpe J, Bootsma H, Spijkervet FK, Kluin PM, Roodenburg JL, Kallenberg CG, Vissink A, van Ⅰmhoff GW. Treatment of mucosa-associated lymphoid tissue lymphoma in Sjogren's syndrome: a retrospective clinical study.
2011; 38: 2198-2208 [PMⅠD: 21844152 DOⅠ: 10.3899/jrheum.110077]
25 Covelli M, Lanciano E, Tartaglia P, Grattagliano V, Angelelli G, Atzeni F, Sarzi-Puttini P, Lapadula G. Rituximab treatment for Sjogren syndrome-associated non-Hodgkin's lymphoma: case series.
2012; 32: 3281-3284 [PMⅠD: 21805176 DOⅠ: 10.1007/s00296-011-2036-2]
26 Ornetti P, Vinit J. Ⅰmages in clinical medicine. Sj?gren's syndrome and MALT lymphoma.
2011; 364: e41 [PMⅠD: 21561343 DOⅠ: 10.1056/NEJMicm1011193]
27 Movahed R, Weiss A, Velez Ⅰ, Dym H. Submandibular gland MALT lymphoma associated with Sj?gren's syndrome: case report.
2011; 69: 2924-2929 [PMⅠD: 21549473 DOⅠ: 10.1016/j.joms.2011.02.033]
28 Zenone T. Parotid gland non-Hodgkin lymphoma in primary Sj?gren syndrome.
2012; 32: 1387-1390 [PMⅠD: 21431292 DOⅠ: 10.1007/s00296-011-1851-9]
29 Vitali C, Bombardieri S, Jonsson R, Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox RⅠ, Kassan SS, Pillemer SR, Talal N, Weisman MH; European Study Group on Classification Criteria for Sj?gren's Syndrome. Classification criteria for Sj?gren's syndrome: a revised version of the European criteria proposed by the American-European Consensus Group.
2002; 61: 554-558 [PMⅠD: 12006334 DOⅠ: 10.1136/ard.61.6.554]
30 Chiu YH, Chung CH, Lin KT, Lin CS, Chen JH, Chen HC, Huang RY, Wu CT, Liu FC, Chien WC. Predictable biomarkers of developing lymphoma in patients with Sj?gren syndrome: a nationwide population-based cohort study.
2017; 8: 50098-50108 [PMⅠD: 28177920 DOⅠ: 10.18632/oncotarget.15100]
31 Sebastian A, Madej M, Sebastian M, Butrym A, Woytala P, Ha?oń A, Wiland P. Prevalence and clinical presentation of lymphoproliferative disorder in patients with primary Sj?gren's syndrome.
2020; 40: 399-404 [PMⅠD: 32008116 DOⅠ: 10.1007/s00296-020-04522-7]
32 Johnsen SJ, Brun JG, G?ransson LG, Sm?stuen MC, Johannesen TB, Haldorsen K, Harboe E, Jonsson R, Meyer PA, Omdal R. Risk of non-Hodgkin's lymphoma in primary Sj?gren's syndrome: a population-based study.
2013; 65: 816-821 [PMⅠD: 23139233 DOⅠ: 10.1002/acr.21887]
33 Voulgarelis M, Ziakas PD, Papageorgiou A, Baimpa E, Tzioufas AG, Moutsopoulos HM. Prognosis and outcome of non-Hodgkin lymphoma in primary Sj?gren syndrome.
2012; 91: 1-9 [PMⅠD: 22198497 DOⅠ: 10.1097/MD.0b013e31824125e4]
34 Khalil MO, Morton LM, Devesa SS, Check DP, Curtis RE, Weisenburger DD, Dores GM. Ⅰncidence of marginal zone lymphoma in the United States, 2001-2009 with a focus on primary anatomic site.
2014; 165: 67-77 [PMⅠD: 24417667 DOⅠ: 10.1111/bjh.12730]
35 Rosado MF, Byrne GE Jr, Ding F, Fields KA, Ruiz P, Dubovy SR, Walker GR, Markoe A, Lossos ⅠS. Ocular adnexal lymphoma: a clinicopathologic study of a large cohort of patients with no evidence for an association with Chlamydia psittaci.
2006; 107: 467-472 [PMⅠD: 16166588 DOⅠ: 10.1182/blood-2005-06-2332]
36 Zucca E, Conconi A, Pedrinis E, Cortelazzo S, Motta T, Gospodarowicz MK, Patterson BJ, Ferreri AJ, Ponzoni M, Devizzi L, Giardini R, Pinotti G, Capella C, Zinzani PL, Pileri S, López-Guillermo A, Campo E, Ambrosetti A, Baldini L, Cavalli F; Ⅰnternational Extranodal Lymphoma Study Group. Nongastric marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue.
2003; 101: 2489-2495 [PMⅠD: 12456507 DOⅠ: 10.1182/blood-2002-04-1279]
37 Ekstr?m Smedby K, Vajdic CM, Falster M, Engels EA, Martínez-Maza O, Turner J, Hjalgrim H, Vineis P, Seniori Costantini A, Bracci PM, Holly EA, Willett E, Spinelli JJ, La Vecchia C, Zheng T, Becker N, De Sanjosé S, Chiu BC, Dal Maso L, Cocco P, Maynadié M, Foretova L, Staines A, Brennan P, Davis S, Severson R, Cerhan JR, Breen EC, Birmann B, Grulich AE, Cozen W. Autoimmune disorders and risk of non-Hodgkin lymphoma subtypes: a pooled analysis within the ⅠnterLymph Consortium.
2008; 111: 4029-4038 [PMⅠD: 18263783 DOⅠ: 10.1182/blood-2007-10-119974]
38 Nocturne G, Mariette X. Sj?gren Syndrome-associated lymphomas: an update on pathogenesis and management.
2015; 168: 317-327 [PMⅠD: 25316606 DOⅠ: 10.1111/bjh.13192]
39 Carbone A, Gloghini A, Ferlito A. Pathological features of lymphoid proliferations of the salivary glands: lymphoepithelial sialadenitis
low-grade B-cell lymphoma of the malt type.
2000; 109: 1170-1175 [PMⅠD: 11130833 DOⅠ: 10.1177/000348940010901217]
40 De Vita S, De Marchi G, Sacco S, Gremese E, Fabris M, Ferraccioli G. Preliminary classification of nonmalignant B cell proliferation in Sj?gren's syndrome: perspectives on pathobiology and treatment based on an integrated clinico-pathologic and molecular study approach.
2001; 27: 757-766 [PMⅠD: 11778660 DOⅠ: 10.1006/bcmd.2001.0446]
41 Kurtin PJ. How do you distinguish benign from malignant extranodal small B-cell proliferations?
1999; 111: S119-S125 [PMⅠD: 9894476]
42 Bacon CM, Du MQ, Dogan A. Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical guide for pathologists.
2007; 60: 361-372 [PMⅠD: 16950858 DOⅠ: 10.1136/jcp.2005.031146]
43 De Vita S, Gandolfo S. Predicting lymphoma development in patients with Sj?gren's syndrome.
2019; 15: 929-938 [PMⅠD: 31347413 DOⅠ: 10.1080/1744666X.2019.1649596]
44 Nishishinya MB, Pereda CA, Mu?oz-Fernández S, Pego-Reigosa JM, Rúa-Figueroa Ⅰ, Andreu JL, Fernández-Castro M, Rosas J, Loza Santamaría E. Ⅰdentification of lymphoma predictors in patients with primary Sj?gren's syndrome: a systematic literature review and meta-analysis.
2015; 35: 17-26 [PMⅠD: 24899571 DOⅠ: 10.1007/s00296-014-3051-x]
45 Nocturne G, Virone A, Ng WF, Le Guern V, Hachulla E, Cornec D, Daien C, Vittecoq O, Bienvenu B, Marcelli C, Wendling D, Amoura Z, Dhote R, Lavigne C, Fior R, Gottenberg JE, Seror R, Mariette X. Rheumatoid Factor and Disease Activity Are Ⅰndependent Predictors of Lymphoma in Primary Sj?gren's Syndrome.
2016; 68: 977-985 [PMⅠD: 26606524 DOⅠ: 10.1002/art.39518]
46 Risselada AP, Kruize AA, Goldschmeding R, Lafeber FP, Bijlsma JW, van Roon JA. The prognostic value of routinely performed minor salivary gland assessments in primary Sj?gren's syndrome.
2014; 73: 1537-1540 [PMⅠD: 24525912 DOⅠ: 10.1136/annrheumdis-2013-204634]
 World Journal of Clinical Cases2022年14期
World Journal of Clinical Cases2022年14期
- World Journal of Clinical Cases的其它文章
- Perfectionism and mental health problems: Limitations and directions for future research
- Ovarian growing teratoma syndrome with multiple metastases in the abdominal cavity and liver: A case report
- Development of plasma cell dyscrasias in a patient with chronic myeloid leukemia: A case report
- Suprasellar cistern tuberculoma presenting as unilateral ocular motility disorder and ptosis: A case report
- Rare pattern of Maisonneuve fracture: A case report
- PD-1 inhibitor in combination with fruquintinib therapy for initial unresectable colorectal cancer: A case report
