Risk factors and optimal predictive scoring system of mortality for children with acute paraquat poisoning
INTRODUCTION
Paraquat (PQ) is a widely used herbicide worldwide. Since paraquat began to be used in agriculture in 1962, the number of patients with acute paraquat intoxication has gradually increased[1]. With the participation of reduced coenzyme II-cytochrome P450 reductase, xanthine oxidase and other enzymes,PQ produces a single cationic free radical PQ, and PQrapidly reoxidizes into PQ. PQreceives electrons from coenzyme II and generates superoxide anions, which then produce peroxynitrite by combining with nitric oxide free radicals. These highly reactive oxygen species and peroxynitrite lead to mitochondrial dysfunction and apoptosis through lipid peroxidation and the activation of nuclear factor-κB, which results in multiple organ damage[2-4]. In the absence of specific antidotes, the mortality rate in children with acute paraquat intoxication (APP) was 14.38%-63.6%[5-7]. Therefore, the early and accurate prediction of mortality is very important in clinical decision-making for children with APP.
8. Grandmother, what big arms you have! : These exclamations23 are a favorite story element for tellers24 and listeners. They are an excellent storybuilding tool, creating anticipation25 and horror for the listener/reader as Little Red Riding Hood realizes she is not talking to her grandmother. Many oral versions of the story add extra body parts to increase the bawdiness26 of the story. The list inevitably27 ends with the teeth however.
At present, several scoring systems have been used to predict the mortality of adult patients with APP, such as the sequential organ failure assessment[8], severity index of paraquat poisoning (SIPP)[9],acute physiology and chronic health evaluation II[10], early warning score (EWS)[11], and modified EWS[12]. However, the predictive powers of the above scoring systems are different, and most importantly, they are unsuitable for children.
There is no scoring system that can be used to predict mortality in children with APP. Because of the simple calculation and available indices, the pediatric critical illness score (PCIS) and pediatric EWS(PEWS) are scoring tools widely used for critically ill children[13-16]. However, there is no report in which the PCIS and PEWS were used to predict the prognosis of children with APP. Our study aimed to investigate the performance of the PCIS, the PEWS, as well as a single clinical index for predicting mortality in children with APP and to provide a theoretical basis for clinical application.
Well, when I was in jail I wrote to my wife, he said. I told her that I was going to be away a long time, and that if she couldn t stand it, if the kids kept asking questions, if it hurt too much, well, she could just forget me, I d understand. Get a new guy, I said she s a wonderful woman, really somethingand forget about me. I told her she didn t have to write me for nothing. And she didn t. Not for three and a half years.
MATERIALS AND METHODS
Patients
We performed a single-center, retrospective, observational study, which was approved by the ethics committee of the West China Second University Hospital, Sichuan University.
Pediatric patients with APP enrolled in this study were < 18 years old and were admitted to our hospital between January 1, 2010 and January 1, 2020. The inclusion criteria were as follows: (1) A diagnosis of APP[17]; and (2) first visit to the hospital with no history of special treatment, such as gastric lavage and hemodialysis. The diagnostic criteria of APP were as follows: (1) The children or family members could provide the history of paraquat exposure; (2) for those who denied paraquat exposure, evidence was found to the contrary, including black–green residue on the skin, an empty paraquat bottle, vomiting, oral mucosal erosion with unknown causes; and (3) blood or urine was positive for paraquat. The exclusion criteria were as follows: (1) Complicated with chronic diseases; (2)other drug exposure; (3) death within 24 h of admission; and (4) discharge against medical advice.
Data collection
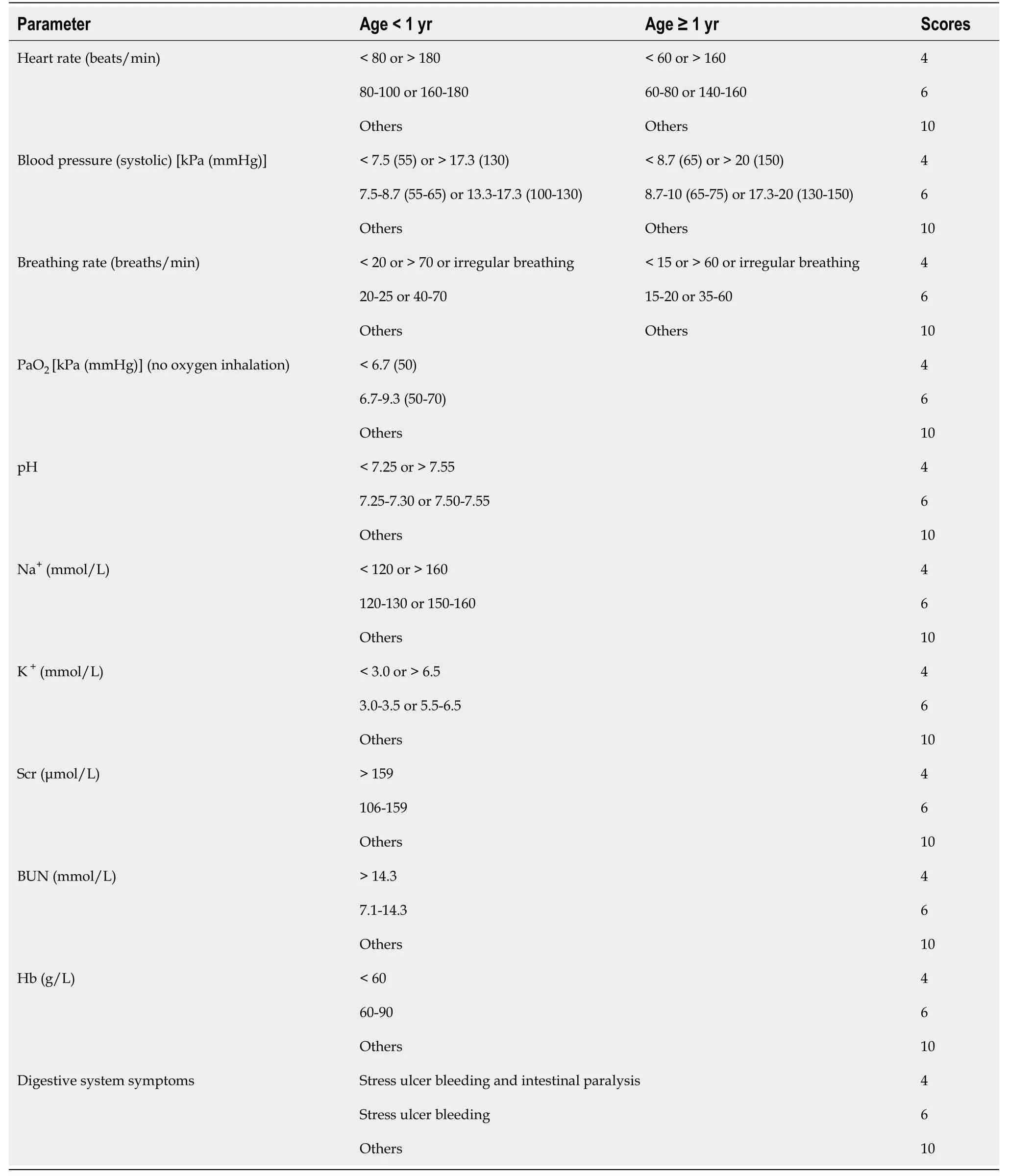
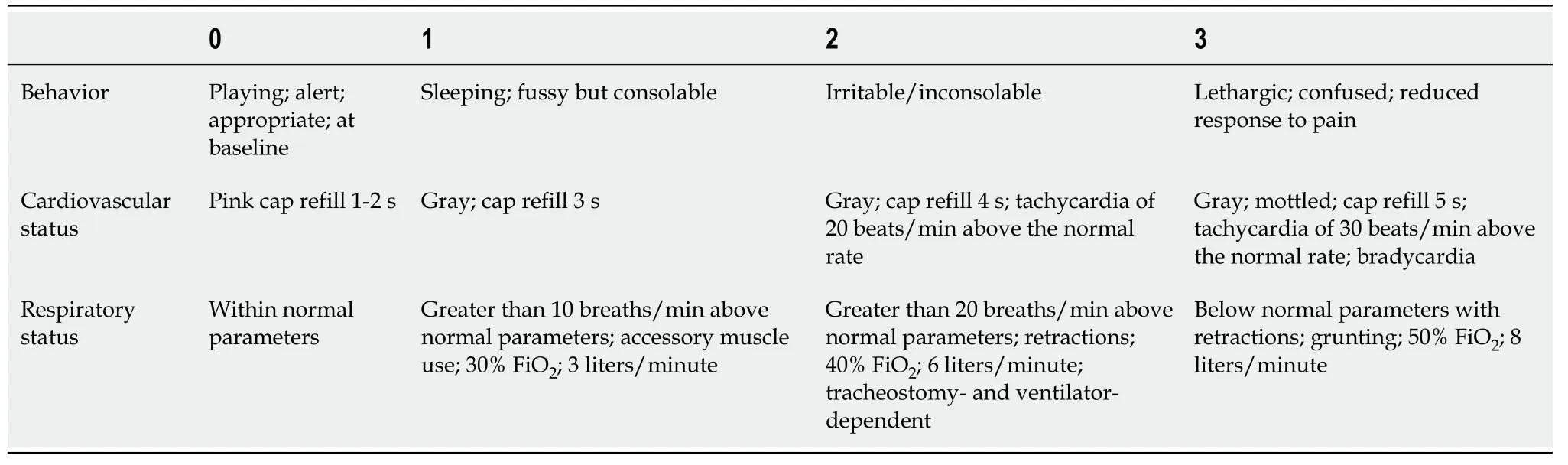
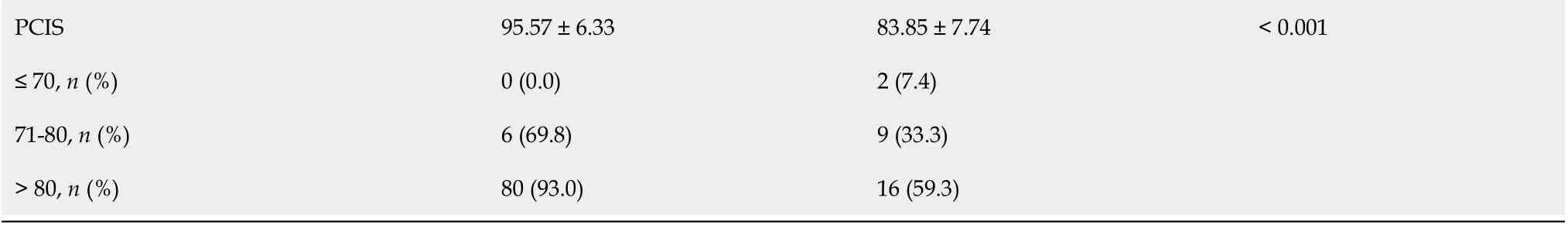
Age, sex, time to blood purification and consultation and related symptoms (vomiting, abdominal pain,oral ulcer and gastrointestinal bleeding) were collected at admission. Routine laboratory tests, including routine blood tests, blood gas, liver function, renal function and electrolytes, were performed. The PCIS[18] (Table 1) and PEWS[19] (Table 2) were calculated within 24 h after admission. Patients with the score of > 80 were considered noncritical, 71-80 critical, and ≤ 70 extremely critical. All children were followed up for at least 90 days.
Treatment
But how do you suppose we can manage to live till summer comes round again? Do not be anxious about that, said the girl; if you will only marry me all will be well
Statistical analysis
All statistical analyses were conducted using IBM SPSS statistics version 21 (IBM Corp & licensors 1989,2011). Continuous variables are presented as the mean ± SD or median (interquartile range) [mean (P,P)]. Categorical variables were expressed as percentages. The two groups were compared using student’s t-tests, chi-square tests, wilcoxon tests, and mann–whitney U tests. Multivariable logistic regression model was computed to identify whether variables were associated with unfavorable outcomes. The receiver operator characteristic [area under the receiver operating characteristic(AUROC)] curve was used to predict probability of mortality. We analyzed the survival rate of children with different PCIS by kaplan–meier survival analysis.< 0.05 was considered statistically significant.
I reached her court safely, said Sylvia, and she received me with much kindness, and immediately began to exercise upon me that brilliant wit which you had bestowed upon her
RESULTS
Comparison of clinical characteristics between survivors and non-survivors
In total, 113 patients were included. During the 90-day follow-up, the overall mortality rate was 23.4%(27/113). All non-survivors died within 20 d; 48.1% (13/27) died within 3 d, and 70.3% (19/27) died within 7 d. The causes of poisoning were suicide (22.1%) and accidental ingestion (77.9%).
Then she fell asleep instantly, and only woke up to hear the clock saying Beauty, Beauty twelve times in its musical voice, which told her at once that she was really in the palace once more
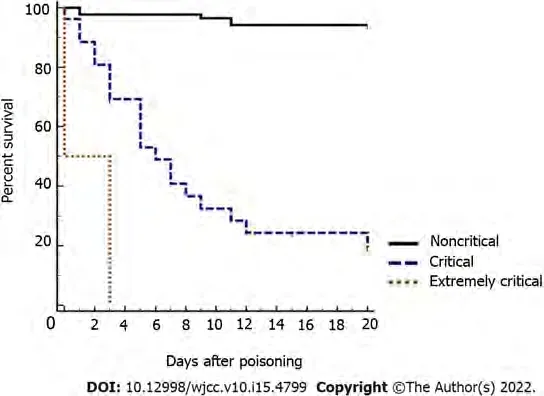
Among the 113 children, 96 (85%), 15 (13.3%) and 2 (1.8%) were categorized as noncritical (PCIS > 80 points), critical (PCIS 71-80 points) and extremely critical (PCIS ≤ 70 points), respectively, and the mortality rates were 16.7% (16/96), 60% (9/15), and 100% (2/2), respectively. As shown in Figure 1, the survival rate of children classified as extremely critical patients (100%) was significantly lower than that of children classified as critical (60%) or noncritical (6.7%) patients (< 0.05).
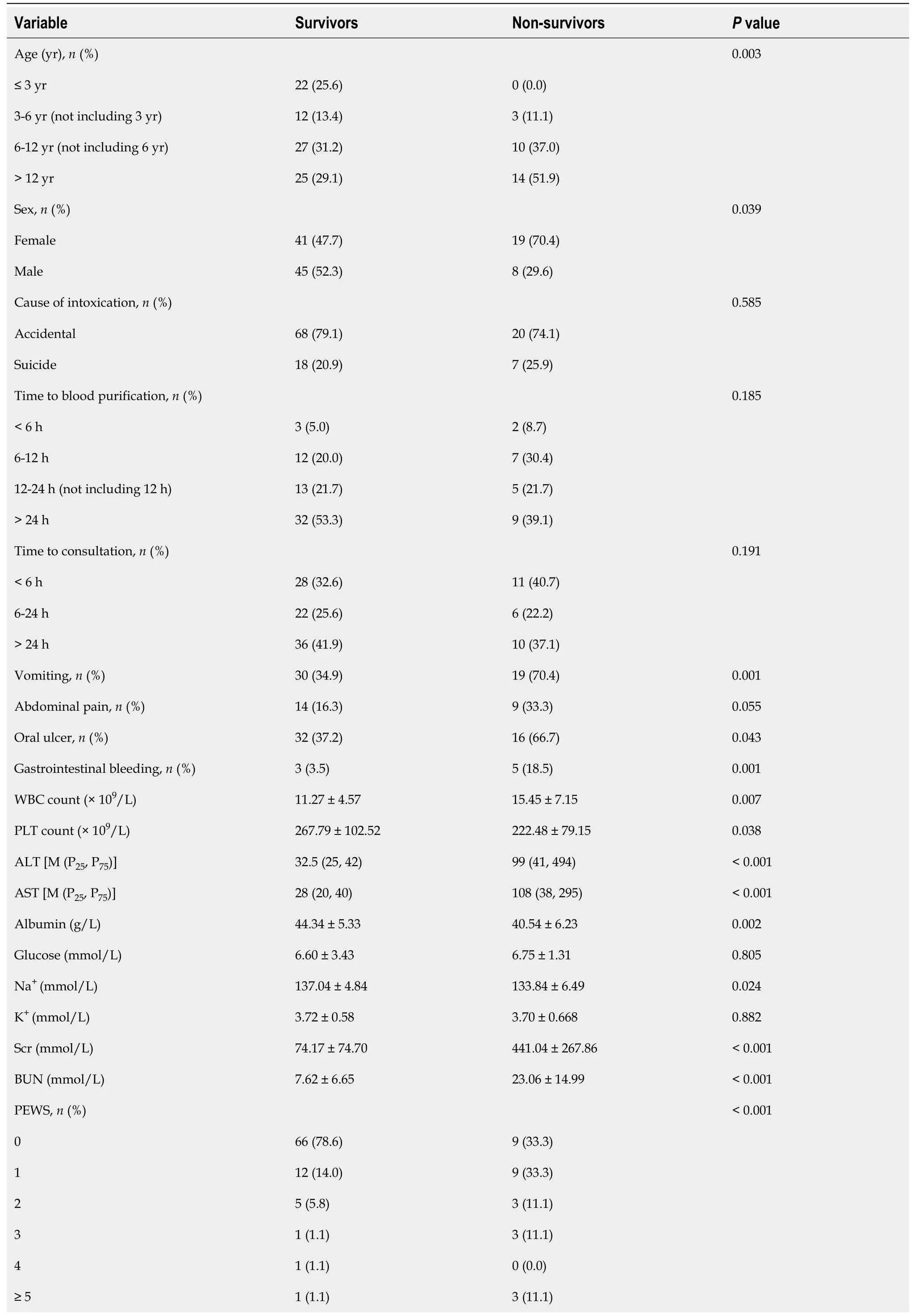
Compared to survivors, the non-survivors were older (8.11 ± 4.7211.48 ± 2.99 years); had higher white blood cell count, serum creatinine (Scr), blood urea nitrogen (BUN), alanine aminotransferase(ALT), aspartate aminotransferase, glucose, and PEWS; and had lower platelet count, albumin, Serum sodium (Na) and PCIS (Table 3) (all< 0.05).
The EWS is widely used in adult patients. However, the vital signs and physiological indices of children of different ages vary widely, and there is a long compensation period before rapid deterioration due to disease. Therefore, the PEWS was established according to the physiological and pathological characteristics of children. The PEWS includes three parts: Consciousness, respiratory status and cardiovascular status. The PEWS is easy to administer and calculate. Nevertheless,multivariate logistic analysis suggested that the PEWS was not an independent risk factor for mortality in children with APP; therefore, the PEWS cannot be used to predict mortality in children with APP.The reasons are as follows: (1) The PEWS comprises physical signs and a few parameters but no objective laboratory indices; and (2) repeated evaluations by doctors and nurses and the anxiety and panic of parents may affect the vital signs of the children, resulting in a decrease in the predictive efficacy of the PEWS[34].
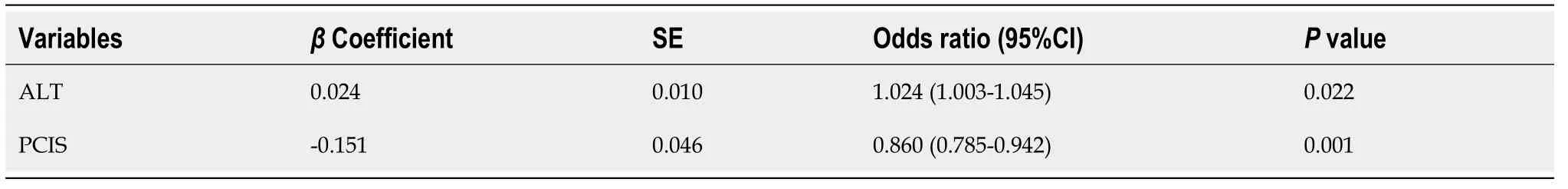
Prognostic risk factors for children with APP
In order to explore the prognostic risk factors for children with APP, we selected variables with< 0.1 in the univariate analysis to perform a multivariable logistic regression analysis. The indices of Scr,BUN, Na, Serum potassium (K), hemoglobin, abdominal pain, vomiting, and gastrointestinal bleeding were included in the PCIS system and were not introduced into the multivariable logistic regression analysis. ALT and PCIS were independent prognostic risk factors for those children with APP (< 0.05)(Table 4).
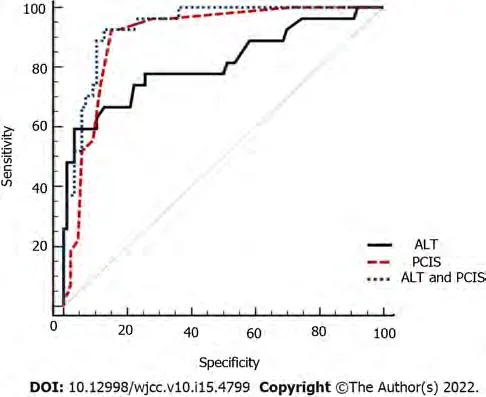
Predictive scoring system development of mortality for children with APP
Because the multiple logistic regression analysis revealed that ALT and PCIS were independent prognostic risk factors for children with APP, we further analyzed the predictive performance of ALT,PCIS and ALT combined with PCIS for mortality in children with APP. Table 5 and Figure 2 show the predictive power of ALT, PCIS and ALT combined with PCIS. The specificity of ALT was high (96.51%),but its sensitivity was low (59.26%). The sensitivity and specificity of PCIS and ALT combined with PCIS were high, 92.30%92.59% and 82.21%87.21%, respectively. The difference in-outcomes wassignificantly higher for ALT combined with PCIS (AUROC: 0.937; 95%CI: 0.875-0.974) than for PCIS(AUROC: 0.905; 95%CI: 0.836-0.952) and ALT (AUROC: 0.814; 95%CI: 0.730-0.881) (all< 0.05). Thus,ALT combined with the PCIS was the optimal scoring system.
We are horrified at the thought of what we have carried within us, and at the consciousness that we have not overcome the evil which has itsorigin in thoughtlessness and pride
Routine blood tests, liver function, renal function, electrolytes, random blood glucose and chest computed tomography tests were performed upon admission. Routine treatments (vomiting induction,oral activated carbon and diuresis) were adapted. Some critically ill children were administered methylprednisolone 15 mg/(kg/d) for 3 d. The patients with infective symptoms were given anti-infective drugs, and those with respiratory failure were given oxygen inhalation or mechanical ventilation. Some critically ill children were treated with hemoperfusion 3-5 times or plasma exchange 3-4 times.Hemodialysis or continuous renal replacement therapy was used for patients with multiple organ dysfunction.

DISCUSSION
We thank the doctors at the Department of pediatrics of West China Second University Hospital for their help with data collection.
The poisoning severity score[30,31] and pediatric logistic organ dysfunction (PELOD) score[32] can be used to predict the prognosis of children with APP. Nevertheless, complex calculations and the availability of indices (such as PO/FiO) in the general ward limit their application in clinical work. In addition, the SIPP[9] and clinical classification of APP[33] have good predictive ability for the prognosis of children with APP. Due to the unavailability of ingestion doses and paraquat concentrations, the clinical classification of APP and SIPP was not adopted in this study.
The median time to consultation in survivors and non-survivors was 22.5 (8.75, 48) and 20 (8, 48)hours, respectively. In addition, there was no significant difference between the survivors and nonsurvivors in the time to consultation < 6 h, 6-24 h, and > 24 h subgroups.
PCIS comprises heart rate, blood pressure, breathing rate, PaO, pondus hydrogenii, Na, K,BUN/Scr, hemoglobin, and digestive system symptoms, and the PCIS system can evaluate the condition of children with APP more comprehensively and objectively than the PEWS system. PCIS is widely used to evaluate the severity and prognosis of critically ill children[13,15]. The PCIS system was first used to predict the prognosis of children with APP, as shown in our study. Our study showed that the survival rate of children classified as extremely critical patients (PCIS ≤ 70 points) was significantly higher than that of children classified as critical (PCIS 71-80 points) and noncritical (PCIS > 80 points)patients. In addition, the AUROC of PCIS was 0.905 (95%CI: 0.836-0.952), with a high sensitivity of 92.3% and a high specificity of 82.21%. A recent study showed that there was no significant difference among the AUROC curves for PCIS, PRISM IV and PELOD-2 in predicting the prognosis of children in pediatric intensive care units[35]. Thus, PCIS can be used to predict the prognosis of children with APP.
The liver is the main source of endogenous antioxidants and plays an important role in metabolism and detoxification. The liver is considered to be the main target of exogenous organism-mediated oxidative damage[36]. Oxidative damage to the liver was observed in rats after a single oral administration of 150 mg/kg paraquat for 20 h[37]. Yang[38] found that 46.52% of paraquat patients suffered from hepatic complications. Metabolic disorders or insufficient antioxidants induced by liver injury are associated with poor outcome after paraquat intoxication. In our study, the multiple regression analysis revealed that ALT was an independent risk factor for mortality in children with APP. The AUROC of ALT was 0.814 (95%CI: 0.730-0.881), the sensitivity was 96.51%, and the specificity was 51.26%. In addition, Zhang[39] found that ALT and BUN reflect organ injuries and paraquat excretion capability of patients, and the two parameters are negatively correlated with the urine-toplasma paraquat ratio. Therefore, we combined ALT with the original PCIS system and evaluated its predictive ability for mortality in children with APP. Our study showed that ALT combined with PCIS had optimal predictive ability, with the AUROC of 0.921 (95%CI: 0.854-0.963) and a high sensitivity of 87.21% and specificity of 92.59%. It is suggested that ALT combined with PCIS has a good predictive ability for mortality in children with APP.
Strengths and limitations of this study
The mortality rate in children with acute paraquat intoxication (APP) was 14.38%-63.6%, the early and accurate prediction of mortality is very important in clinical decision-making for children with APP.
CONCLUSION
The mortality rate in children with APP was high. ALT and PCIS were independent prognostic risk factors for children with APP. ALT combined with PCIS is an optimal predictive scoring system for mortality in children with APP.
ARTICLE HIGHLIGHTS
Research background
The early and accurate prediction of mortality can help clinicians with clinical decision-making and treatment of children with acute paraquat intoxication. However, there are few articles about acute paraquat poisoning in children, and there is no suitable scoring system that can be used to predict the mortality of these patients. In this study, we studied the risk factors and optimal predictive scoring system of mortality for children with acute paraquat poisoning. To date, this is the first article on the predictive score of acute paraquat poisoning in children. Of course, a limited number of children with APP were included in our study. The results of this study need to be further verified by large-sample and multicenter research.
Research motivation
Between articles, he took breaks by watching the nearby traffic and pedestrians6. The coffee shop was next to a huge parking lot. The lot was for customers of a grocery store, movie rental7 store, pharmacy8, bank, and restaurant. Kevin considered his outdoor seat the perfect place for one of his favorite activities—people watching.
45.King:It is important that the king approves of his son s choice in a wife since he has the ability to censure92 his son and even take away his inheritance and birthright.Return to place in story.
Research objectives
Our aim is to optimize a predictive scoring system for mortality in children with APP, and help doctors to make clinical decisions.
Research methods
We compared the clinical characteristics between the two groups and analyzed the independent prognostic risk factors. The survival rates were assessed using kaplan-meier survival analysis. The best scoring system was established by using the area under the receiver operating characteristic curve analysis.
Outside the castle there was a beautiful garden, in which grew bright red5 and dark blue flowers, and blossoms like flames of fire; the fruit glittered like gold, and the leaves and stems waved to and fro continually
Research results
Alanine aminotransferase (ALT) and pediatric critical illness score (PCIS) were independent prognostic risk factors for children with APP. The survival rate of children classified as extremely critical patients was significantly lower than that of children classified as critical or noncritical patients. The sensitivity and specificity of ALT combined with PCIS were high.
Research conclusions
ALT and PCIS were independent prognostic risk factors for children with APP. ALT combined with PCIS is an optimal predictive mortality scoring system for children with APP.
Research perspectives
The results of this study need to be further verified by large-sample and multicenter research.
ACKNOWLEDGEMENTS
The early prediction of mortality is important in clinical decision-making for patients with APP.Previous studies have indicated that plasma paraquat concentration can effectively predict the mortality of patients with APP[20,21]. However, Gil[21] found that some patients with low paraquat concentration in plasma still had poor outcomes. The reasons are as follows. The plasma paraquat concentration reached a peak value within 0.5-2 h after ingestion[22], and the half-life is 5 h[23]. The concentration of paraquat in plasma decreased obviously in the early stage, and the survival expectations would decrease from 70% to 30% for a delay of 1 h[23]. The time of detecting paraquat concentration in plasma had an impact on the accuracy of paraquat measurements. In addition, most children with APP accidentally ingested paraquat; therefore, clinicians cannot estimate the dose of paraquat they ingested.Paraquat measurement was unavailable in almost all primary hospitals. Therefore, the paraquat concentration in plasma was not included in the prognostic risk factor analysis of children with APP. In addition, clinical indices such as serum lactic acid[24], K[25], blood amylase[26] and peripheral blood monocyte count[27] were considered to be effective in predicting the prognosis of patients with APP.Paraquat binds to plasma protein after entering the bloodstream and is quickly distributed to many organs, resulting in multiple organ damage[28]. Therefore, using a single index to predict the mortality of APP patients is inaccurate, while the combination of multiple indicators is more comprehensive and reasonable[29].
When I learned of Clemente s death I could only marvel11 that the man who had helped find a hero had been a bonafide hero trying to help an entire nation
The mortality rate in children with APP was high. The early prediction of mortality is important in clinical decision-making for patients with APP. Therefore, our aim is to optimize a predictive scoring system for mortality in children with APP.
FOOTNOTES
Song Y and Wang H designed the study, made the review, and wrote the manuscript; Song Y,Wang H, and Tao YH made the literature search, made table, and reviewed the manuscript; all authors read and approved the final manuscript.
The study was approved by the Ethics Committee of the West China Second University Hospital, Sichuan University. Approval No: 2020(004).
Informed written consent was obtained from the patient for publication of this report.
We have no financial relationships to disclose.
Before they got halfway13 up the hill, the fragrance14 of the lilacs drifted down to them, and the kids started running. Soon, the mother began running, too, until she reached the top.
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
China
Yue Song 0000-0002-4679-0330; Yu-Hong Tao 0000-0012-0650-4399.
Guo XR
A
Guo XR
 World Journal of Clinical Cases2022年15期
World Journal of Clinical Cases2022年15期
- World Journal of Clinical Cases的其它文章
- Diet and intestinal bacterial overgrowth: Is there evidence?
- Spontaneous liver rupture following SARS-CoV-2 infection in late pregnancy: A case report
- Metastasis of liver cancer to the thyroid after surgery: A case report
- Solitary primary pulmonary synovial sarcoma: A case report
- Knot impingement after arthroscopic rotator cuff repair mimicking infection: A case report
- Clear aligner treatment for a four-year-old patient with anterior crossbite and facial asymmetry: A case report
