Spontaneous liver rupture following SARS-CoV-2 infection in late pregnancy: A case report
INTRODUCTION
Coronavirus disease-2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2), is characterized by systemic inflammatory response syndrome (SIRS), vascular damage,microangiopathy, angiogenesis, and thrombosis[1]. High mortality rates are associated with SARS-CoV-2 (2%-6%), especially among the elderly and individuals with underlying comorbidities such as diabetes, hypertension, and heart disease[2]. In the current pandemic, hepatic dysfunction was observed in 14%-53% of SARS-CoV-2-infection cases, especially in severe cases. Moreover, acute liver injury has a higher mortality rate[2]. Studies related to liver disease and involvements during pregnancy seem to be limited.
The mechanisms causing potential liver damage include direct viral cytotoxicity[3], immune-related damage due to SIRS[4], respiratory failure-related hypoxic changes, pro-coagulation intravascular state with endotheliitis, drug-induced liver injury and in severe cases of cardiac congestion. The exacerbation of hidden/pre-existing liver disease should also be considered.
In direct hepatic damage, angiotensin-converting enzyme 2 (ACE2) appears to be the key receptor for viral entry into the cell[5]. The virus attaches to the host cellthe viral S protein connection to the host transmembrane serine protease 2[6]. Subsequently, the virus is incorporated into the cell by endocytosis and the viral genome is released from the endosome[7,8]. The viral genome is replicated in the replicasetranscriptase complex[9,10]. The assembly of mature SARS-CoV-2 virions occurs within the endoplasmic reticulum-to-Golgi intermediate compartment[11,12] with subsequent exocytosis[13].
Cases of spontaneous liver rupture during pregnancy with SARS-CoV-2 infection have not been reported yet.
CASE PRESENTATION
Chief complaints
A 32-year-old woman with a gestational age of 32 wk + 4 d experienced epigastric pain. She was asymptomatic for COVID-19.
In good faith, cried the mother, I must send my child thither6.22 Come hither, Fanny;23 look what comes out of thy sister s mouth when she speaks. Wouldst not thou be glad, my dear, to have the same gift given thee? Thou hast nothing else to do but go and draw water out of the fountain, and when a certain poor woman asks you to let her drink, to give it to her very civilly. 24
History of present illness
She first experienced pain in the epigastrium 2 h before the initial examination, with a gradual worsening of her condition.
History of past illness
And when Little Two-eyes thought that Little Three-eyes was sound asleep, she said her rhyme, Little goat, bleat, Little table, appear, and ate and drank to her heart s content, and then made the table go away again, by saying, Little goat, bleat, Little table, away
Personal and family history
Informed written consent was obtained from the patients for the publication of this report and any accompanying images.
Physical examination
Physical examination revealed epigastric pain, with a body temperature of 36.5 °C, blood pressure of 17,6/11 kPa, and oxygen saturation of 97%. Electrocardiogram (ECG) and cardiotocographic findings were normal. We initially suspected her to have hemolysis, elevated liver enzymes, and low platelet count syndrome (HELLP) and performed fetal lung maturity induction while administering 12 mg betamethasone intravenously for 24 h.
Laboratory examinations
After some years passed in this way, she heard that the daughter of the king of the country she was living in was going to marry a Prince called Fickle
Imaging examinations
The initial ultrasound examination revealed a live fetus without any abnormal findings.
Over a week, the liver enzymes and platelet count returned to normal levels. On the fourth day of hospitalization, pain developed in the right subcostal region and physical examination revealed a positive Murphy’s sign, while her ECG was normal, D-dimers concentration was above 10000 μg/L, and liver enzymes were slightly elevated (ALT: 372 IU/L; AST: 258 IU/L). Therefore, we ruled out acute coronary syndrome. Abdominal ultrasound examination confirmed no abnormalities in the abdominal organs, a viable fetus, and no free fluid in the abdominal cavity. We administered anticoagulant therapy(0.3 mL low molecular weight heparin every 12 h). The correlation between the laboratory findings and clinical findings was unclear. Within 2 h, the patient developed a collapsed state without trauma and her blood test showed a marked increase in ALT (1789.8 IU/L) and AST (1747.2 IU/L). In addition,lactate dehydrogenase (LD) levels (1671 IU/L) and platelets (88 × 10/L) were highly elevated.Therefore, an emergency cesarean section was planned.
He drew near and told me that through the power of his magic arts he had caused the soft music to waken me, and had made his way through bolts and bars to offer me his hand and heart
Further diagnostic work-up
Then she left the tower and drove the geese into a field. And when they had reached the common where the geese fed she sat down and unloosed her hair,33 which was of pure gold.34 Curdken loved to see it glitter in the sun, and wanted much to pull some hair out.35 Then she spoke23:
FINAL DIAGNOSIS
According to the laboratory and clinical findings, the diagnosis was most likely spontaneous liver rupture associated with SARS-CoV-2 infection.
TREATMENT
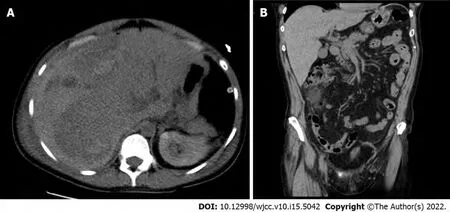
While performing the emergency cesarean section, we observed the findings of hemoperitoneum, and an apparent 6-cm liver rupture on the edges of segments V and VI of the right hepatic lobe. Suture and drainage were performed. The patient delivered a baby without signs of vitality, and lost 800 mL of blood. The postoperative condition was accompanied by a deficient response to supplementation with blood derivatives. The patient underwent computed tomography (CT) of the abdomen with intravenous contrast (Figure 1, Figure 2A and B), which revealed a massive subcapsular hematoma in the right hepatic lobe with active bleeding from the branches of the hepatic artery. Thereafter, embolization was performed as we suspected limited viability of the right hepatic lobe and proceeded with more conservative management. Hemodynamic decompensation continued, while paralytic ileus developed with an increase in the abdominal volume and dark bloody secretion was drained. There were signs of abdominal compartment syndrome and anemia (hemoglobin, 107-71 g/L). We investigated the abdominal cavity for bowel insufflation and performed drainage of a bulky subcapsular hematoma(involving the V, VI, VII, and VIII segments and good vitality of segments IV, II, and III). Liver packing was performed to control the damage. Postoperatively, the patient was maintained in a stable condition with mechanical ventilation and tested positive for SARS-CoV-2 infection. A repeat laparotomy was performed after two days when the liver packing was discontinued and no liver hemorrhages were observed. Furthermore, her subcapsular hematoma did not progress, and the liver parenchyma was stable. Thereafter, we gradually adjusted the liver parameters without coagulopathy or thrombocytopenia and extubated or spontaneously ventilated. A postoperative CT scan of the liver revealed no free fluid or progression of hepatic hematoma, and the drains were removed. Chest CT revealed groundglass opacity in both lungs with right pleural effusion, which was resolved by puncture, followed by massive hemoptysis conservatively treated with bronchoscopy (adrenaline) and non-invasive ventilation with high-flow air.
OUTCOME AND FOLLOW-UP
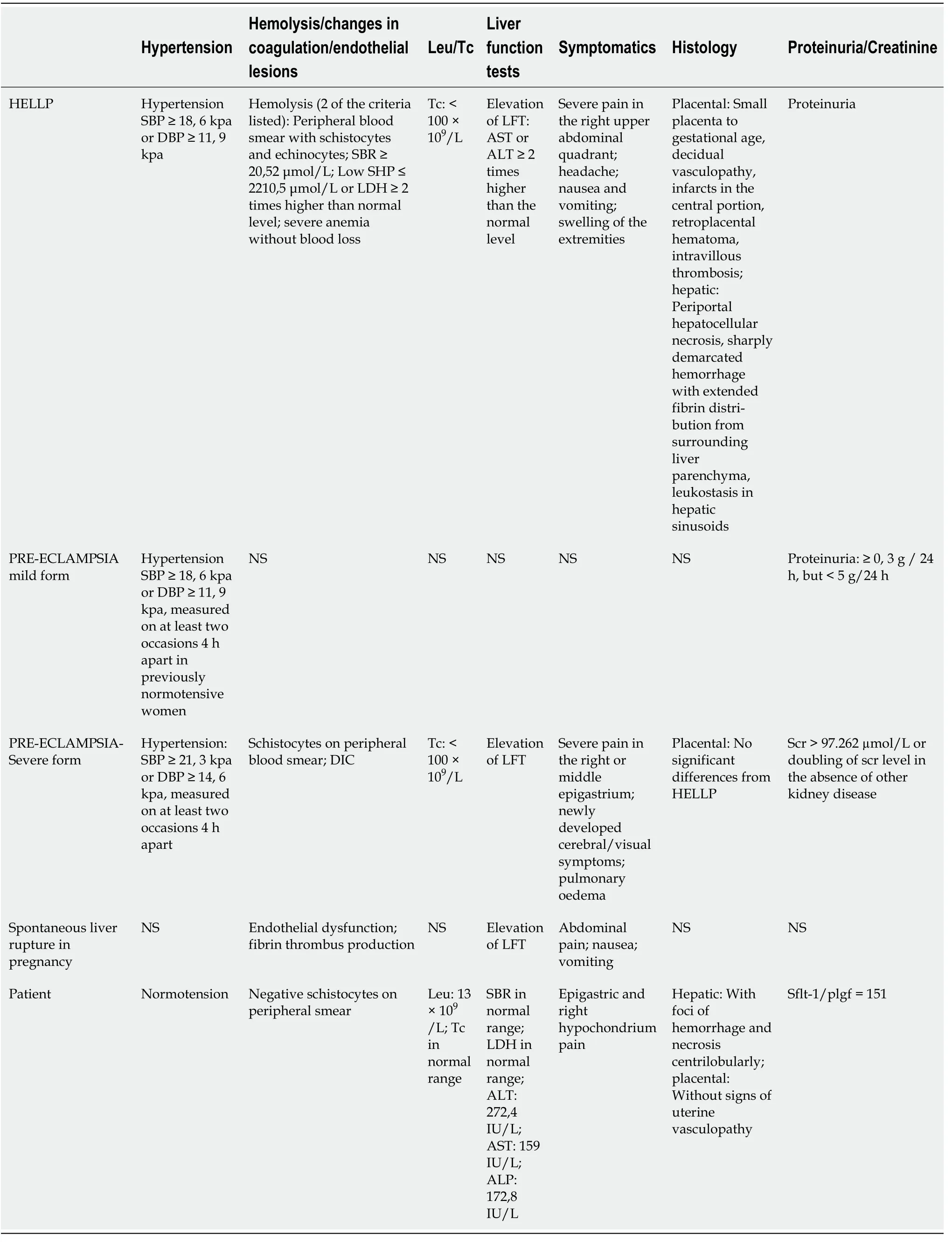
According to our differential diagnosis, HELLP syndrome appeared to be the most likely diagnosis,which occurs in 1 per 1000 pregnancies and is associated with a high mortality rate (up to 40%) due to the possible occurrence of disseminated intravascular coagulopathy[16] and spontaneous liver rupture[17,18]. The only causal therapy is to terminate the pregnancy immediately after confirming the diagnosis and evaluating the clinical condition of the pregnant woman and the gestational age of the fetus. In the present case, we observed the angiogenic markers, sharp rise in liver transaminases over a short period, inconclusive clinical signs, negative schistocytes, and the coincidence with lung involvement (Table 1), and concluded that they were unrelated to HELLP. Likewise, the histological findings of the liver biopsy specimens did not confirm this diagnosis. Pre-eclampsia, a multisystem disease associated withhypertension occurring after the 20week of pregnancy with proteinuria, was considered. One component of the clinical picture is characterized by the dysfunction of other maternal organs, such as renal insufficiency, hepatic involvement, neurological or hematological complications, and uteroplacental dysfunction or fetal growth restriction[19]. Risk factors for the occurrence of pre-eclampsia include antiphospholipid syndrome, previous pre-eclampsia, chronic hypertension, pre-gestational diabetes, pre-pregnancy body mass index > 30 kg/m, and the use of assisted reproductive technology[20]. Pre-eclampsia commonly presents with headache, epigastric pain,visual disturbances, nausea, and vomiting[21]. The association between pre-eclampsia and HELLP syndrome requires sufficient explanation.
These were the wolf s parting words, and the Prince could not restrain his tears when he saw his friend vanishing in the distance; but one glance at his beloved mermaid soon cheered him up again, and they continued on their journey merrily
DISCUSSION
Pregnancy-specific liver diseases can be categorized as early and late pregnancy diseases; the HELLP syndrome is a late pregnancy-related liver disease along with liver rupture/infarction[14]. Other late pregnancy-related liver diseases include intrahepatic cholestasis in pregnancy, acute fatty liver of pregnancy (AFLP), and nonspecific elevated liver enzymes. Liver rupture occurs in approximately 1 per 200000 pregnancies and is largely associated with AFLP or HELLP syndrome, rarely without associated liver disease[15]. Running a panel of blood tests is the standard protocol for diagnosing hepatic pathology: ALT, AST, ALP, gamma-glutamyl transferase, bilirubin, Alpha-fetoprotein, LD, hepatitis antibodies (A, B, C, E, HCMV, EBV, ceruloplasmin, copper, iron, ferritin, dot liver 7, coagulation parameters, schistocyte smear). The differential diagnoses of the causes of liver rupture in pregnancy include HELLP syndrome, severe pre-eclampsia, and hemangioma rupture.
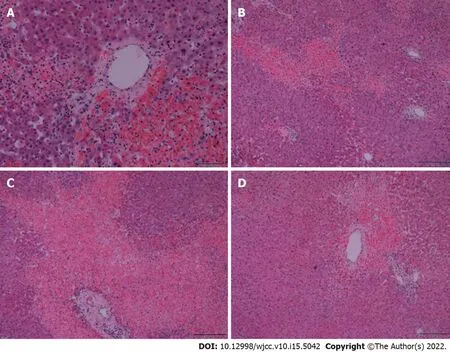
A biopsy of the liver tissue showed foci of hemorrhage and necrosis with an irregular centrilobular distribution (Figure 2), no hepatocyte steatosis and no cholestasis. Fibrin thrombi or inflammatory infiltrations were not detected. Thus, patients with HELLP syndrome were excluded. Pathological dissection of the placenta and fetus showed that the chorionic plate and decidua basalis did not show inflammation, thrombosis, or vasculitis. Both chorionic and stem villi were small with regard to the gestational age, suggesting an acceleration of maturation, and were vascularly altered with more abundant Hofbauer macrophages. We also noted irregular arborization with globular appearance of distal villous hypoplasia. Multifocally, a significant fibrinoid increase was clear, which occurred intravillously;fibrinoid sites completely filled individual villi but also intervillously and subchorially; however, this finding did not exceed 30% of the tissue volume. Escalation was excessive knotting of the hyperplastic syncytiotrophoblasts that appeared similar to Tenney-Parker changes. Cytotrophoblasts were discontinuous. Agglutination and infarcts were present below the decidua, chorion, and centrally in the placental parenchyma; however, they were within 15% of the parenchyma. Thus, it was shown that fetal death occurred because of acute intrauterine asphyxia during acute ischemia of the placenta under hemorrhagic shock conditions in the mother. The subsequent course was no longer complicated, and the patient was followed up at our department and the pulmonary clinic, and antiphospholipid syndrome was ruled out. A follow-up CT scan revealed significant regression of the pulmonary changes with fluidothorax regression on the right. According to the control spirometry findingsventilation was within normal limits.
Blood tests results revealed elevated liver enzymes [alanine aminotransferase (ALT): 272.4 IU/L,aspartate transaminase (AST): 159.6 IU/L, and alkaline phosphatase (ALP): 172.8 IU/L], without any findings of viral hepatitis (the samples were negative for hepatitis A virus, hepatitis B virus, hepatitis C virus, hepatitis E virus, Epstein-Barr virus (EBV), human cytomegalovirus (HCMV). Her coagulation parameters were normal; hence other pregnancy-related liver pathologies were excluded. The hepatologist suggested that her condition was most likely related to hepatopathy of unknown etiology. SARSCoV-2 positivity on reverse transcription-polymerase chain reaction was confirmed, although the patient was asymptomatic.
Regarding the inconclusive diagnostic modalities associated with lung involvement, we considered the possibility of liver rupture due to damage caused by SARS-CoV-2 infection. The presumed mechanism of viral entry isthe host’s ACE2 receptors, which are abundantly present in alveolar type-2 cells. ACE2 receptors are expressed in the gastrointestinal tract, vascular endothelium, and liver cholangiocytes. Hepatic involvement may be directly related to the cytopathic effect of the virus,uncontrolled immune reaction, sepsis, or drug-induced liver damage[2]. Recent findings suggest that viral elements may be present in endothelial cells, with an accumulation of dead inflammatory endothelial cells. These findings indicate that SARS-CoV-2 infection facilitates the pathogenesis of endotheliitis in several organs as a direct consequence of viral involvement and the inflammatory response of the host[22].
The patient had no comorbidities and was not taking any chronic medication.
Vascular effects of SARS-CoV-2 (endotheliitis, procoagulation, and thrombosis) seem to be important contributors to placental damage. Potential fetal complications are most likely linked to placental circulation damage. Vivanti[23] described a transplacental transmission of SARS-CoV-2, where the placenta showed diffuse perivillous fibrin deposits with infarction and acute and chronic intervillous lesions. Immunohistochemistry may prove a seropositive status of the villous trophoblast for SARSCoV-2 nucleocapsid protein[23]. Linenhan[24] hypothesized that trophoblast necrosis is directlyrelated to either viral damage or the host’s subsequent inflammatory response. Thus, it appears as a form of placental disease that is specifically associated with direct infection of the placental villous trophoblast by SARS-CoV-2, which represents true SARS-CoV-2 placentitis. During hepatic hemorrhage, apart from offering conservative therapy with hemoptysis, vasopressor support, and hemotherapy, the possibility of performing embolization of the branches of the hepatic artery should be considered along with surgical management. The success of embolization depends on the visualization of the hemorrhagic focus, embolization technique, and availability of the artery. This is indicated in hemodynamically stable patients[25].
Surgical intervention is indicated for hemodynamic instability, usually involving an approach by a midline laparotomy, also accounting for the possibility of association with the cesarean section; when it is technically impossible to carry out a primary liver suture, it is suitable to apply the principles of damage control surgery (packing, ligation of the portal vein branch, followed by stabilization, and a repeat laparotomy with a definitive control of hemorrhage and a liver tissue biopsy).
On the following morning, before the sun rose, he fastened hisknapsack on his back, took his wooden provision box in his hand, and went away among the sand-hills towards the coast path. This way was more pleasant than the heavy sand road, and besides it was shorter; and he intended to go first to Fjaltring, near Bovbjerg, where the eel-breeder lived, to whom he had promised a visit.
Liver transplantation can be considered an ultimum refugium in cases of hepatic failure. However, in cases of SARS-CoV-2 infection, liver transplantation is a high-risk procedure, despite reports of successful cases[26]. Hence, the prognosis of the patient depends on the degree of SIRS development,multi-organ involvement during SARS-CoV-2 infection, and the early indication of interventional therapy.
The limitation of histology is the absence of direct detection of viral particles in the liver parenchyma,and the examination was not available at the time of the histological evaluation. The influence of viral infection can be considered a primary and secondary cause. It can be assumed that SARS-CoV-2 infection may have contributed to the development of SIRS and endotheliitis, with an effect on the occurrence of microvascular and macrovascular thromboses to aggravate pre-existing hepatopathy.However, this premise needs to be further investigated and evaluated in a larger cohort of patients.
CONCLUSION
SARS-CoV-2 infection may contribute to the worsening of hepatopathy during pregnancy, possibly by affecting the endothelium in the SIRS microenvironment that may contribute to liver rupture developing in the framework of severe hepatopathy. Spontaneous liver rupture is associated with massive infant and maternal mortality rates as high as 42%[27] and 39%[17], respectively. The management of such clinical case scenarios requires close collaboration between the obstetrician and the surgeon with an urgent indication for cesarean section, preferably approaching through midline laparotomy after a thorough liver examination for any liver injury and its treatment. Nevertheless, the complications induced by the presence of SARS-CoV-2 in the development of severe hepatopathy during pregnancy require further research.
FOOTNOTES
Ambro? R was the attending physician, reviewed the literature and contributed to manuscript;Molnár J and ?pi?ka P reviewed the literature and consulted the histopathological findings; Klos D performed the surgery, and was responsible for supervising this article; Hambalek Josef performed the gynaecological part of the surgery, and was also the attending physician; Skanderová D provided histopathological findings including imaging material; all authors issued final approval for the version to be submitted.
the Ministry of Health, Czech Republic-conceptual Development of Research Organization, No. FNOl 00098892.
But as he did this he had plenty of time to read them as well, and he read away at them until at last he was just as wise as his master--who was a great wizard4--and could perform all kinds of magic
The whole castle was surrounded by a deep moat, and the drawbridge and the gates, and even the water in the moat, were all of the same sombre hue46 as the walls and towers
There was no significant personal or family history.
The authors declare that they have no conflict of interest.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Czech Republic
Radek Ambro? 0000-0002-5572-3148; Martin Sta?ek 0000-0002-1308-7390; Ján Molnár 0000-0002-4231-1726; Petr ?pi?ka 0000-0003-3166-2624; Du?an Klos 0000-0002-3097-4418; Jozef Hambálek 0000-0003-3047-674X; Daniela Skanderová 0000-0001-9106-8104.
?eská léka?ská komora, No. 1150408180.
Chen YL
A
Chen YL
 World Journal of Clinical Cases2022年15期
World Journal of Clinical Cases2022年15期
- World Journal of Clinical Cases的其它文章
- Diet and intestinal bacterial overgrowth: Is there evidence?
- Metastasis of liver cancer to the thyroid after surgery: A case report
- Solitary primary pulmonary synovial sarcoma: A case report
- Knot impingement after arthroscopic rotator cuff repair mimicking infection: A case report
- Clear aligner treatment for a four-year-old patient with anterior crossbite and facial asymmetry: A case report
- Catheter-related infections caused by Mycobacterium abscessus in a patient with motor neurone disease: A case report
