Nonfunctional bladder paraganglioma misdiagnosed as hemangioma: A case report
INTRODUCTION
Paraganglioma of the urinary bladder (PUB) is a rare bladder neoplasm subtype, accounting for approximately 0.06% of bladder tumors. There are significant differences in symptoms between individuals,which makes this tumor extremely easy to misdiagnose or miss. A case of nonfunctional PUB diagnosed and treated in our hospital is reported herein.
CASE PRESENTATION
Chief complaints
A 22-year-old female patient was hospitalized on February 14, 2021, because "the bladder was found to feel occupied for 5 d."
History of present illness
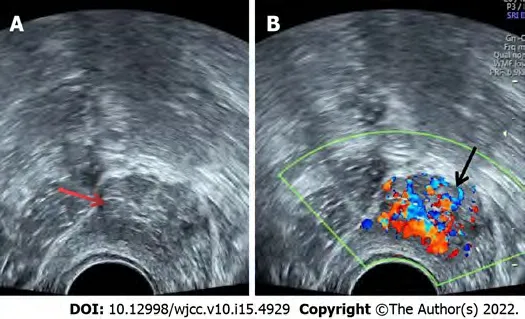
The patient underwent transvaginal ultrasonography for routine premarital examination 5 d prior.During the examination, a 2.5 cm × 2.1 cm medium-echo mass protruding into the right anterior wall of the bladder was found. The shape was regular. The boundary was clear, and the wide base was connected to the bladder wall. Color Doppler flow imaging detected rich strip blood flow signals, with an RI of 0.66 (Figure 1).
History of past illness
The patient had a free previous medical history.
30. Must make in that time six shirts for us out of star-flowers: Note that the spell must be broken with a method similar to how it was cast. White shirts caused the enchantment, so the sister must make new shirts for her brothers to counteract the spell. Return to place in story.
Personal and family history
The catheter was removed 14 d after the operation. Postoperative pathological findings indicated paraganglioma of the bladder. The cut surface of the lump was grayish-white and gray–brown, and the texture is slightly hard. Microscopically, the tumor cells were polygonal, with large nuclei, visible nucleoli, a nest-like arrangement, and abundant blood vessels. The immunohistochemical staining results were as follows: Syn (+), CgA (+), CD56 (+), S-100 (supporting cells+), CK (-), GATA3 (-), and Ki-67 (+, < 2%) (Figure 3). The patient’s 24-h urinary CA, plasma-free MNs and 24-h urinary vanillylmandelic acid (VMA) improved, and the results were normal. During the 6 mo of follow-up, there was no recurrence or metastasis of the tumor, and the patient did not complain of discomfort.
Physical examination
The patient had no frequent urination, urgency dysuria, or gross hematuria. There were no symptoms,such as hypertension, palpitations or cold sweats, during urination. Upon the physical examination, the patient’s heart rate was 75 bpm, and her blood pressure was 110/68 mmHg. There was no eminence,tenderness or percussion pain in the bladder area.
In this disguise she went over the seven mountains to the seven dwarfs, and knocked at the door and cried, Pretty things to sell, very cheap, very cheap
Laboratory examinations
Blood analysis, blood biochemistry and urinalysis revealed no significant abnormalities. Electrocardiogram and abdominal ultrasound (except bladder) also showed no abnormality.
Imaging examinations
The bladder is the most conventional site of urogenital paragangliomas (79.2%). Most PUBs are histologically benign, and only approximately 10% of PUB cases are malignant[14]. At present, there is no unified standard for the treatment of paraganglioma of the urinary bladder, but surgery is still the main method. Surgical methods include transurethral resection of bladder tumor, partial cystectomy and radical cystectomy. The specific choice of surgical method should be based on the actual situation of the patient and the technical strength of the surgeon to reduce risk and ensure safety as much as possible. In this case, laparoscopic partial cystectomy was performed because the mass did not protrude into the bladder cavity and the broad base was connected to the bladder wall.
FINAL DIAGNOSIS
Nonfunctional paraganglioma of the urinary bladder.
TREATMENT
When perfecting the relevant examinations and excluding surgical contraindications, the patient underwent laparoscopic partial cystectomy under general anesthesia. During the operation, a spaceoccupying lesion on the right side of the bladder outside the peritoneum was found, with a smooth surface. The space invaded the bladder wall, and its border was unclear. The bladder wall connected to the new mass was removed under direct laparoscopic vision. The bladder incision was then sutured.After observing that there was no obvious bleeding from the incision, an abdominal drainage tube was placed, a 16 F three-chamber balloon tube was placed in the bladder, and 10 mL of water was injected.The procedure went smoothly. The patient had no obvious discomfort during the operation, with normal vital signs.
They greeted one another rapturously, and were just sitting down to talk over everything cosily56, and enjoy the Enchanter s discomfiture57 together, when out he burst in a fury from behind a bush
OUTCOME AND FOLLOW-UP
The patient was previously healthy and her family had no relevant medical history.

DISCUSSION
PUB is a neuroendocrine tumor that originates from the chromaffin tissue of the sympathetic nerve in the bladder wall[1]. PUB mainly occurs in adults[2] and is mostly located on the sidewall of the bladder;the trigone has the least common incidence[3], which may be related to the distribution of chromaffin tissue on the bladder wall. PUB can be divided into functional and nonfunctional types according to whether the tumor secretes catecholamine hormones and the release activity of hormones[4,5].Functional PUB can manifest as a clinical type or a resting type. Hypertension, dizziness, palpitations and even syncope during urination are the specific manifestations of clinical PUB. Compared with resting PUB, the symptoms of the clinical type are more subtle. Only touching or cutting the tumor during examination or surgery can cause a large amount of catecholamines to enter the bloodstream,which causes the patient to develop symptoms. Nonfunctional PUB primarily manifests as painless hematuria and urinary tract obstruction or is found during physical examination. In the present case,the patient did not have any clinical symptoms. Indeed, the mass was only discovered by chance during a gynecological physical examination. There was no clinical manifestation of large amounts of catecholamines in the blood when touching the tumor during the operation or after the operation. In addition, the catecholamine hormone levels in the blood and urine of the patient measured after the operation were within the normal ranges. Therefore, it was diagnosed as nonfunctional PUB.
In summary, PUB is very uncommon. It is misdiagnosed easily and missed clinically. For the bladder appears a single round, well-circumscribed and wide base of the mass, the possibility of PUB should be considered before surgery. Surgeons should be fully prepared. Patients should be followed up for a long time after surgery. There are currently no histological, genetic or molecular markers that can distinguish benign and malignant paragangliomas preoperatively. The diagnosis of a malignant tumor relies only on the presence of metastasis.
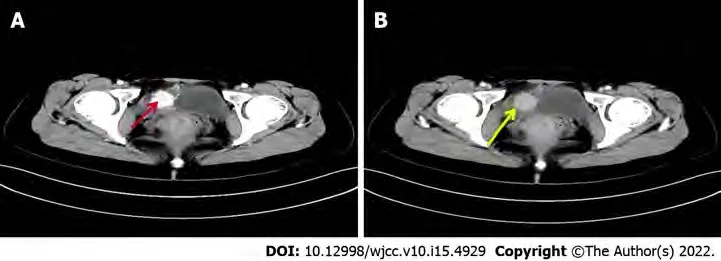
In our case, the first lesion was found on vaginal ultrasound. Because the probe was placed in the vaginal vault, we could comprehensively observe the bladder and urethra during the vaginal ultrasound scan, and the results were clearer than those of transabdominal ultrasound. The transvaginal ultrasound findings were consistent with those previously reported based on transabdominal ultrasound[5,6,11]. A wide-base isoechoic round mass with abundant blood flow signals was detected.During enhanced CT, we also noticed a single lesion on the bladder wall. After enhancement, the signalwas obviously strengthened and then slowly subsided in the delay period; thus, it was considered to be a hemangioma. However, most patients with bladder hemangioma have recurrent painless hematuria[12]. In addition, sessile, blue, raised masses were found by cystoscopy[13]. Although the two can be indistinguishable on imaging, they can be distinguished by combining clinical symptoms and other auxiliary examinations.
An enhanced computed tomography (CT) scan of the bladder was performed after admission: the right front of the bladder was occupied, and the boundary with the bladder wall was not clear. The bladder was under pressure, and the size was approximately 2.5 cm × 2.4 cm. In the arterial phase of the enhanced scan, obvious enhancement could be seen as well as multiple tortuous vascular shadows. The lesion was considered a hemangioma (Figure 2).
This snow-flake10 grew larger and larger, till at last it became the figure of a woman, dressed in garments of white gauze, which looked like millions of starry12 snow-flakes linked together
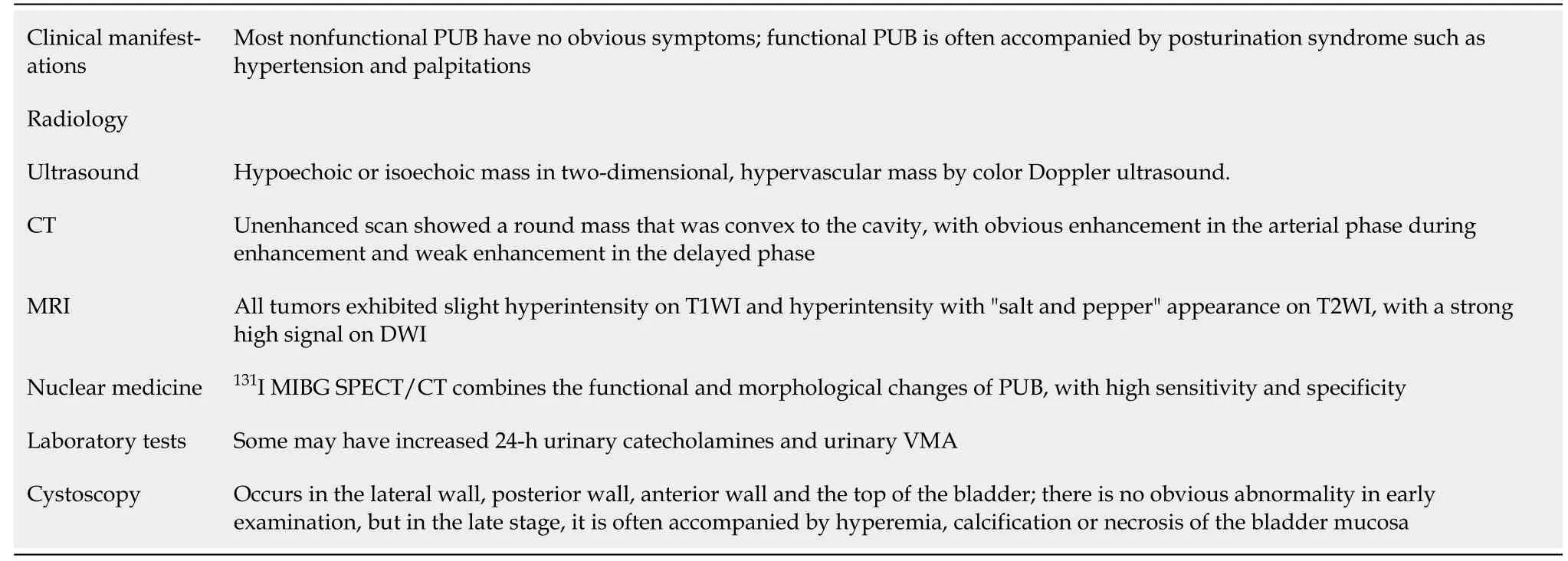
Qualitative diagnosis of paraganglioma mainly depends on the detection of blood and urine catecholamines and 24-h urine VMA. Location diagnosis relies on imaging [Ultrasound, CT and magnetic resonance imaging (MRI)] and cystoscopy. Ultrasound is the most routinely used method for the urinary system. PUB shows a hypoechoic or isoechoic mass with a wide base on two-dimensional ultrasound. Color Doppler ultrasound can elicit abundant blood flow signals in PUB[5,6]. PUB on plain CT scan imaging is a single round or round-like soft tissue mass on the lateral wall of the bladder. It may be accompanied by necrotic cystic degeneration and arc-shaped calcification. Based on enhanced CT scans, PUB is significantly enhanced in the arterial phase, with weakened enhancement in the delayed phase, which is its typical feature; arterial shadows are occasionally visible[6]. This feature is of great significance for preoperative localization and qualitative diagnosis. In contrast, most bladder urothelial carcinomas show mild to moderate enhancement on enhanced CT scans[7]. PUB display an equal or slightly high signal on T1WI in MRI and a high "salt and pepper" signal on T2WI; on DWI, it shows a high signal. PUB shows significant enhancement after intravenous injection of Gd-DTPA[6,8].Radionuclide-labeled metaiodobenzyl guanidine (MIBG) imaging can combine the functional characteristics of pheochromocytoma with morphological changes with high accuracy and specificity[9]. PUB showed hypermetabolic lesions on
I MIBG SPECT/CT. Nuclear medicine examination can accurately identify the location and size of lesions and can perform staging determination and treatment[10](Table 1).
CONCLUSION
The imaging patterns of PUB and bladder hemangioma are similar. In clinical practice, the possibility of PUB should be considered for a single wide-based isoechoic mass in the bladder, especially functional PUB may cause some adverse effects during surgery. Surgeons should be fully prepared. Patients should be followed up for a long time after surgery so that recurrence of the disease can be detected early.
FOOTNOTES
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
The authors declare that they have no conflicts of interest.
Informed consent was obtained from the patient for information and images to be published.
At last an idea struck him, and he said to his sons: You must all go out into the owrld, and look about you, and each learn a trade, and then, when you return, whoever can produce the best masterpiece shall have the house
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Chen J was the patient’s radiologist, reviewed the literature and drafted the manuscript; Chen J and Yang HF were responsible for the revision of the manuscript for important intellectual content; all authors gave final approval for the version submitted.
China
Oho! cried the soldier, I will tickle9 thy nose for thee, so that thou shalt soon lose thy fancy for growling, and he aimed at the bear and shot it through the muzzle10; it fell down and never stirred again
Jiao Chen 0000-0001-8293-7689; Han-Feng Yang 0000-0002-4593-7150.
Gong ZM
A
Except that it didn't. The real caption of the post was "good morning" in Arabic. But for some unknown reason, Facebook's artificial intelligence-powered translation service translated the text to
Gong ZM
1 Siatelis A, Konstantinidis C, Volanis D, Leontara V, Thoma-Tsagli E, Delakas D. Pheochromocytoma of the urinary bladder: report of 2 cases and review of literature.
2008; 60: 137-140 [PMID: 18500228]
2 Purnell S, Sidana A, Maruf M, Grant C, Agarwal PK. Genitourinary paraganglioma: Demographic, pathologic, and clinical characteristics in the surveillance, epidemiology, and end results database (2000-2012).
2017; 35: 457.e9-457.e14 [PMID: 28325651 DOI: 10.1016/j.urolonc.2017.02.006]
3 Beilan JA, Lawton A, Hajdenberg J, Rosser CJ. Pheochromocytoma of the urinary bladder: a systematic review of the contemporary literature.
2013; 13: 22 [PMID: 23627260 DOI: 10.1186/1471-2490-13-22]
4 Male M, Ye T, Tao J, Chen ZQ, Peng E. Differentiating Nonfunctional Paraganglioma of the Bladder from Urothelial Carcinoma of the Bladder: Pitfalls and Breakthroughs.
2019; 2019: 1097149 [PMID: 31781590 DOI:10.1155/2019/1097149]
5 Zhang B, Fu Z, Liu L, Qiao B, Liu C. Non-functional paraganglioma of urinary bladder managed by transurethral resection.
2019; 45: 910-915 [PMID: 31038858 DOI: 10.1590/S1677-5538.IBJU.2018.0604]
6 Qin J, Zhou G, Chen X. Imaging manifestations of bladder paraganglioma.
2020; 9: 346-351 [PMID:32233638 DOI: 10.21037/apm.2020.03.09]
7 Wentland AL, Desser TS, Troxell ML, Kamaya A. Bladder cancer and its mimics: a sonographic pictorial review with CT/MR and histologic correlation.
2019; 44: 3827-3842 [PMID: 31676920 DOI:10.1007/s00261-019-02276-w]
8 Liang J, Li H, Gao L, Yin L, Zhang J. Bladder Paraganglioma: Clinicopathology and Magnetic Resonance Imaging Study of Five Patients.
2016; 13: 2605-2611 [PMID: 27085560]
9 Withey SJ, Christodoulou D, Prezzi D, Rottenberg G, Sit C, Ul-Hassan F, Carroll P, Velusamy A, Izatt L, Nair R, Jacques AET. Bladder paragangliomas: a pictorial review.
2022; 47: 1414-1424 [PMID: 35157102 DOI:10.1007/s00261-022-03443-2]
10 Jain TK, Basher RK, Gupta N, Shukla J, Singh SK, Mittal BR. Unusual Presentation of Bladder Paraganglioma:Comparison of (131)I MIBG SPECT/CT and (68)Ga DOTANOC PET/CT.
2016; 15: 65-67 [PMID:26912984 DOI: 10.4103/1450-1147.167591]
11 Li Y, Guo A, Tang J, Li Q, Fei X, Zhang Y, Gao J. Evaluation of sonographic features for patients with urinary bladder paraganglioma: a comparison with patients with urothelial carcinoma.
2014; 40: 478-484 [PMID:24412175 DOI: 10.1016/j.ultrasmedbio.2013.10.014]
12 Xiao L, Granberg CF, Hull NC. Bladder hemangioma: An arduous diagnosis of hematuria.
2021; 16:1042-1046 [PMID: 33680273 DOI: 10.1016/j.radcr.2021.02.032]
13 Syu SH, Chan KS, Hsiao CH, Chen WY, Lee LM, Wen YC. A Large Urinary Bladder Hemangioma Mimicking Urachal Cancer: A Case Report and Literature Review.
2019; 123: 224-226 [PMID: 30308263 DOI:10.1016/j.urology.2018.09.033]
14 Rzepka E, Gilis-Januszewska A, Opalińska M, Sowa-Staszczak A, Hubalewska-Dydejczyk A. Difficulties in the diagnosis and treatment of malignant paraganglioma of the urinary bladder.
2020; 71: 196-197 [PMID: 32293698 DOI: 10.5603/EP.a2019.0068]
 World Journal of Clinical Cases2022年15期
World Journal of Clinical Cases2022年15期
- World Journal of Clinical Cases的其它文章
- Diet and intestinal bacterial overgrowth: Is there evidence?
- Spontaneous liver rupture following SARS-CoV-2 infection in late pregnancy: A case report
- Metastasis of liver cancer to the thyroid after surgery: A case report
- Solitary primary pulmonary synovial sarcoma: A case report
- Knot impingement after arthroscopic rotator cuff repair mimicking infection: A case report
- Clear aligner treatment for a four-year-old patient with anterior crossbite and facial asymmetry: A case report
