Extensive complex thoracoabdominal aortic aneurysm salvaged by surgical graft providing landing zone for endovascular graft: A case report
INTRODUCTION
Surgical repair of complex thoracoabdominal aortic aneurysm (CAAA) is associated with a higher perioperative mortality[1,2]. Endovascular aortic repair (EVAR) has been increasingly performed due to its minimal invasiveness that results in reduced periprocedural complications[3]. However, EVAR is a challenging procedure in CAAA without the infrarenal neck due to the lack of landing zone for the stent grafts (SGs) or cases involving the visceral or renal arteries (RA). Herein, we report a case of CAAA with concomitant involvement of the common iliac artery (CIA) treated by a stepwise-combined surgery and EVAR, in which the surgical graft of the proximal half of CAAA facilitated a sealing zone for EVAR in the distal half.
CASE PRESENTATION
Chief complaints
A 60-year-old male was referred to our clinic for a large AAA detected during ultrasound screening of the abdominal aorta during cardiovascular screening check-up.
History of present illness
He had a history of heavy smoking (50 pack years). The patient had developed mild shortness of breath for the past 3 wk. Coronary angiography revealed chronic total occlusion of the mid right coronary artery with good collateral blood supply from the left coronary artery. Percutaneous coronary intervention was deferred as symptoms subsided after medical therapy. The patient was then referred to our clinic after the screening abdominal ultrasound revealed a CAAA.
History of past illness
The patient had a history of hypertension and renal tuberculosis 5-years prior. His electrocorticography performance status was also dramatically decreased from 4 to 2 after his diagnosis of renal tuberculosis.
Personal and family history
The patient had not any personal or family history.
Physical examination
A pulsating mass was palpable in the peri-umbilical area.
Laboratory examinations
The baseline creatinine level was 1.1 mg/dL. Other laboratory findings were all within normal limit.
Imaging examinations
Thereupon they bent27 their steps towards the sea, which stretched out before them, as far as their eyes could see, all the waves dancing and glittering in the bright sunshine
MULTIDISCIPLINARY EXPERT CONSULTATION
Jang AY and Kang WC were the patient’s interventionists, reviewed the literature and contributed to manuscript drafting, writing, editing, and revising; Oh PC, Kang JM, and Park CH were interventionists or surgeons of the patient, who reviewed and edited the manuscript; all authors issued final approval for the version to be submitted.
FINAL DIAGNOSIS
The final diagnosis was a long CAAA involving visceral arteries, RAs, and both CIAs requiring extensive correction.
TREATMENT
Informed written consent was obtained from the patients for the publication of this report and any accompanying images.
EVAR was performed 15 mo post-surgery. After implantation of the main SG (Endurant 32 × 103 mm,Medtronic, Minneapolis, MN, United States) on the surgical graft, a limb extension was deployed for the right CIA aneurysm (Endurant 16 × 156 mm). Another limb extension (Endurant 16 × 125 mm) for the left external iliac artery and an additional SG (GORE
VIABAHN
Endoprosthesis 8 × 100 mm, Gore,Flagstaff, AZ, United States) for the left IIA were implanted using the sandwich technique, to preserve the left IIA (Figure 3A). Follow-up angiography revealed a type Ib endoleak in the left IIA, which was sealed by a bare metal stent (Express? LD 9 × 37 mm, Boston Scientific, Marlborough, MA, United States).
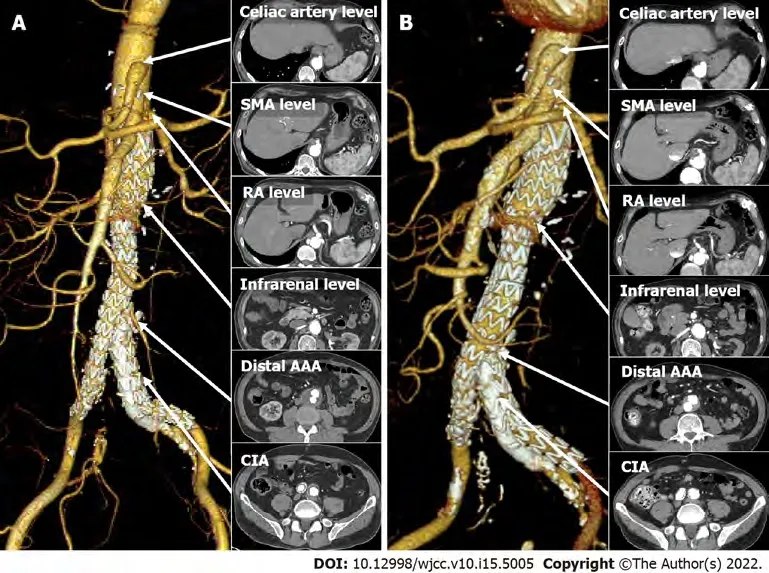
OUTCOME AND FOLLOW-UP
The patient was discharged in 3 d without any complications. CTA performed 5 mo post-EVAR showed no endoleaks or compromise of SGs (Figure 3A). CTA performed 5 years post-EVAR showed no endoleaks or graft failure (Figure 3B). Over time, the maximal diameter of the distal AAA (49 mm to 32 mm) and CIA (30 mm to 19 mm) were reduced. The patient has been uneventful without complaints for the following 5 years and is being followed up in the outpatient department.
Life just hadn’t turned out the way I’d planned. Sure, I was happy. I had a wonderful husband and two great kids in the center of my life. But somehow, working part-time as a secretary and mom hardly fit my definition of someone my classmates had voted as “most likely to succeed.” Had I really wasted 20 years?
DISCUSSION
Although extensive CAAAs are generally corrected by mega-aortic surgery, such invasive strategies are associated with a high-risk of mortality and morbidity. To our knowledge, this case is the first to demonstrate that Crawford type IV CAAA concurrently involving bilateral CIA can be successfully treated by coordinating the surgical graft to provide a landing zone for the infrarenal SG. This combined approach may be a considerable option for patients with extensive CAAA.
And there are surprises. One time I came home to find a note on the front door that led me to another note, then another, until I reached the walk-in closet. I opened the door to find Scott holding a pot of gold (my cooking kettle) and the treasure of a gift package. Sometimes I leave him notes on the mirror and little presents under his pillow.
Crawford type IV AAA is associated with a high-risk of post-operative mortality and morbidity with mortality. Post-operative mortality is up to 7% with high rates of detrimental complications, such as spinal cord injury or AKI[1,2]. The preferred treatment strategy, surgical, EVAR, or combined, is debatable, although EVAR has become popularized for its less invasiveness. AAA with the CIA involvement is also associated with a high-risk surgical mortality and complications[3]. EVAR has not been proven to reduce mortality, but perioperative complication rates are less severe[4-7]. In this patient, open surgery of the whole extent of AAA was not considered because of the patient’s initial poor performance and high-risk. Additionally, EVAR for the juxtarenal aneurysm was not an option for the lack of infrarenal landing zone and angulated proximal neck. Fenestrated EVAR was also not available in South Korea at the time. However, combined surgery was feasible because there was an intact area of the infrarenal aorta without aneurysmal change or calcification, which enabled distal anastomosis of the surgical graft. The branched surgical graft also facilitated a sufficient landing zone for EVAR of the distal aneurysm and IIAs.
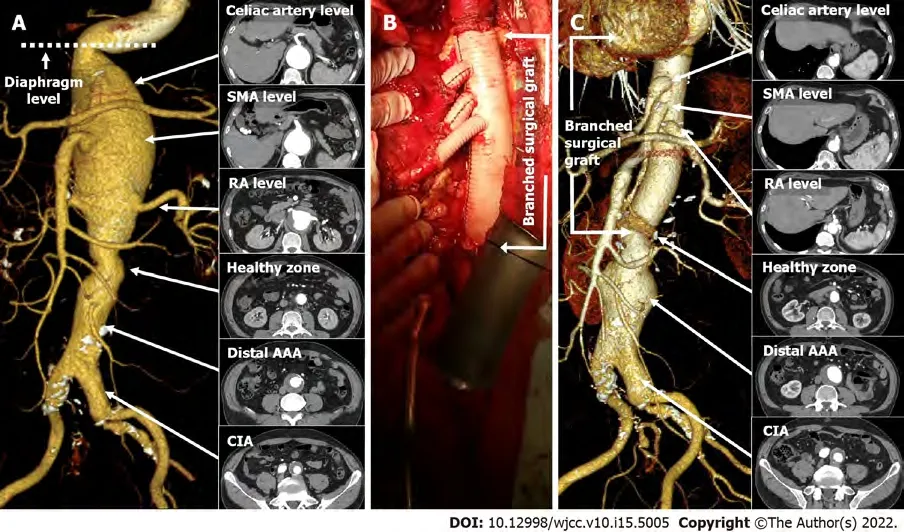
Computed tomographic aortography (CTA) was performed successfully. The diagnosis was made based on the serial axial images and its Three-dimensional reconstruction of the CTA. The patient had a Crawford type IV CAAA consisting of a proximal and distal aneurysmal sac separated by a 1 cmhealthy zone in the infrarenal level (Figure 1A). The proximal AAA was a fusiform juxtarenal aneurysm(max diameter: 79 mm), starting directly below a sharp kink at the diaphragm level and ending at approximately 4 cm distal to the RA (Figure 1A). The distal aneurysm (max diameter: 49 mm) was fusiform starting 5 cm distal to the RA and involving both the CIAs, where occlusion of the right internal iliac artery (IIA) was observed (Figure 1A).
You have come just in time, said the Prince, for I should have been married to-morrow; but I will not have the long-nosed Princess, and you alone can save me
CONCLUSION
This case demonstrates that surgical graft can provide a sufficient landing zone for the EVAR in patients with extensive CAAA with the concomitant CIA involvement.
FOOTNOTES
Due to the poor performance of the patient, we planned a stepwise-combined surgery and EVAR(surgical debranching of the visceral/RA followed by a second stage EVAR) to minimize invasiveness.
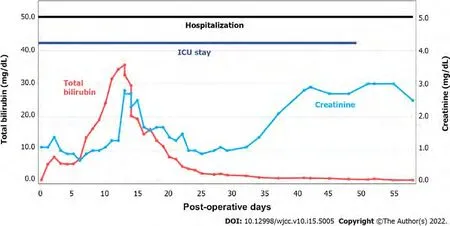
Open surgery was performed by a retroperitoneal approach. Supraceliac clamping was performed slightly distal to the diaphragm while distally clamping the infrarenal healthy zone of the aorta. Surgery was prolonged due to difficulty in locating the small-calibered calcified right RA. End-to-end anastomosis between the Coseli branched graft (Gelweave
Coselli Thoracoabdominal Graft, Vascuteck-Terumo, Renfrewshire Scotland, United Kingdom), proximal/distal aortic stump and visceral/RAs was performed, and reinforced by the remaining aortic wall (Figure 1B). The total duration of surgery was approximately 7 h from start to finish of anesthesia. After surgery, the patient remained in the intensive care unit (ICU) for approximately 50 d for liver failure, acute kidney injury (AKI), and pneumonia(Figure 2). The second stage EVAR was delayed until the patient was physically and mentally ready for the second procedure. He refused of undergoing any type of additional interventions, including surgery, due to the traumatic memories of staying in the ICU for almost 2 mo. The 10-mo post-surgical CTA showed no dysfunction of the surgical graft (Figure 1C). There was no change in diameter of the distal AAA (maximal diameter: 49 mm), although the diameter of the left CIA slightly increased from 27 mm to 30 mm, compared with previous CTA.
The authors declare that they have no conflict of interest.
The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Although the surgery was successfully performed without any intra-operative complications, the patient exhibited life-threatening post-operative morbidities, such as AKI, liver failure, and pneumonia.Post-surgical AKI rate is as high as 39% in CAAA repair, while new onset dialysis incidence is up to 4%[1,2]. In patients with CAAA undergoing visceral vessel repair (VVR), the postoperative mortality was 8.9%, while chances for hemodialysis (HD) and pneumonia were 7.6% and 17.2%, respectively[8]. The independent predictors for mortality in patients undergoing VVR were poor functional status, baseline creatinine, the presence of diabetes and older age. It is likely that the patient’s poor initial performance status may have been associated with the life-threatening liver and renal injury after surgery. The most optimal way of reducing such liver or renal injuries is reducing ischemic time[9]. Alternative methods,such as selective renal perfusion with cold saline or crystalloids have been introduced[10]. Selective visceral perfusion to both the hepatic and renal artery have also shown promising results in reducing ischemic injury[11]. He developed AKI within 2 d of surgery and creatinine levels were not fully recovered until discharge (Figure 2). His creatinine level was 2.5 mg/dL at discharge. He gradually developed chronic kidney disease, which eventually led to HD in 3 years. His bilirubin level after initial surgery was also increased up to 35.7 mg/dL, while the exact cause of isolated bilirubinemia was not confirmed; abdominal ultrasound did not show obstruction of the biliary tract. The prolonged ischemic time may have caused impairment of the liver and kidney. The patient also developed hospital-acquired pneumonia 3-d after the surgery. He was unable to wean from ventilator support for 49 d, which prolonged his stay in the ICU. He was discharged 60 d after the surgery (Figure 2). These detrimental complications altogether suggest that the patient may have had a high chance of developing a debilitating complication had he received open mega surgery of the whole extent of CAAA, from the supraceliac to CIA level.
Then my father poked12 his chopsticks just below the fish eye and plucked out the soft meat. Amy, your favorite, he said, offering me the tender fish cheek. I wanted to disappear. At the end of the meal my father leaned back to and belched13 loudly, thanking my mother for her fine cooking. It s a polite Chinese custom to show you are satisfied, explained my father to our astonished guests. Robert was looking down at his plate with a reddened face. The minister managed to muster14 up a quiet burp. I was stunned15 into silence for the rest of the night.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
South Korea
It s the most amazing thing that will ever happen in my life. This was Roger s first National League home run, and I caught the ball. Tears rolled down my face. Roger came running out at the end of the inning and said, I can t believe it. I said, You can t? I can t!
Albert Youngwoo Jang 0000-0002-8802-268X; Pyung Chun Oh 0000-0002-9955-223X; Jin Mo Kang 0000-0002-1477-9778; Chul Hyun Park 0000-0001-7982-1765; Woong Chol Kang 0000-0003-4590-7178.
Chen YL
A
They had each a pot for their porridge, a little pot for the Little, Small, Wee Bear; and a middle-sized pot for the Middle Bear; and a great pot for the Great, Huge Bear
Chen YL
1 Latz CA, Boitano L, Schwartz S, Swerdlow N, Dansey K, Varkevisser RRB, Patel V, Schermerhorn ML. Editor's Choice -Mortality is High Following Elective Open Repair of Complex Abdominal Aortic Aneurysms.
2021; 61: 90-97 [PMID: 33046385 DOI: 10.1016/j.ejvs.2020.09.002]
2 Swerdlow NJ, Wu WW, Schermerhorn ML. Open and Endovascular Management of Aortic Aneurysms.
2019;124: 647-661 [PMID: 30763206 DOI: 10.1161/CIRCRESAHA.118.313186]
3 Bannazadeh M, Jenkins C, Forsyth A, Kramer J, Aggarwal A, Somerset AE, Bove PG, Long GW. Outcomes for concomitant common iliac artery aneurysms after endovascular abdominal aortic aneurysm repair.
2017; 66:1390-1397 [PMID: 28697942 DOI: 10.1016/j.jvs.2017.02.058]
4 Katsargyris A, Oikonomou K, Klonaris C, Bal A, Yanar F, Verhoeven EL. Common iliac and hypogastric aneurysms:open and endovascular repair.
2015; 56: 249-255 [PMID: 25512317]
5 Paravastu SC, Jayarajasingam R, Cottam R, Palfreyman SJ, Michaels JA, Thomas SM. Endovascular repair of abdominal aortic aneurysm.
2014; CD004178 [PMID: 24453068 DOI:10.1002/14651858.CD004178.pub2]
6 Schermerhorn ML, O'Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population.
2008; 358: 464-474 [PMID: 18234751 DOI:10.1056/NEJMoa0707348]
7 Stather PW, Sidloff D, Dattani N, Choke E, Bown MJ, Sayers RD. Systematic review and meta-analysis of the early and late outcomes of open and endovascular repair of abdominal aortic aneurysm.
2013; 100: 863-872 [PMID:23475697 DOI: 10.1002/bjs.9101]
8 Patel VI, Lancaster RT, Conrad MF, Lamuraglia GM, Kwolek CJ, Brewster DC, Cambria RP. Comparable mortality with open repair of complex and infrarenal aortic aneurysm.
2011; 54: 952-959 [PMID: 21723071 DOI:10.1016/j.jvs.2011.03.231]
9 Waked K, Schepens M. State-of the-art review on the renal and visceral protection during open thoracoabdominal aortic aneurysm repair.
2018; 4: 31 [PMID: 29552513 DOI: 10.21037/jovs.2018.01.12]
10 Wynn MM, Acher C, Marks E, Engelbert T, Acher CW. Postoperative renal failure in thoracoabdominal aortic aneurysm repair with simple cross-clamp technique and 4°C renal perfusion.
2015; 61: 611-622 [PMID: 25720924 DOI:10.1016/j.jvs.2014.10.040]
11 Fernández-Doblas J, Ortega-Loubon C, Pérez-Andreu J, Linés M, Fernández-Molina M, Abella RF. Selective visceral perfusion improves renal flow and hepatic function in neonatal aortic arch repair.
2018;27: 395-401 [PMID: 29590367 DOI: 10.1093/icvts/ivy091]
 World Journal of Clinical Cases2022年15期
World Journal of Clinical Cases2022年15期
- World Journal of Clinical Cases的其它文章
- Diet and intestinal bacterial overgrowth: Is there evidence?
- Spontaneous liver rupture following SARS-CoV-2 infection in late pregnancy: A case report
- Metastasis of liver cancer to the thyroid after surgery: A case report
- Solitary primary pulmonary synovial sarcoma: A case report
- Knot impingement after arthroscopic rotator cuff repair mimicking infection: A case report
- Clear aligner treatment for a four-year-old patient with anterior crossbite and facial asymmetry: A case report
