Radical cystoprostatectomy with orthotopic neobladder for a case of treatment emergent neuroendocrine prostate cancer presenting as bladder mass with hematuria-a rare instance of tumor remission after local control
Dear editor
Treatment emergent neuroendocrine prostate cancer(t-NEPC)is most commonly observed after development of resistance to androgen deprivation therapy(ADT)and is associated with rapid progression and widespread metastases with survival less than 1 year from diagnosis[1].Management of this disease is mainly through cytotoxic chemotherapy and there is no published evidence of treating the primary prostatic lesion in this stage of the disease,unlike that of localized prostate cancer or castrate sensitive metastatic prostate cancer[2].In this letter,we report the only known case of t-NEPC who presented with an initial diagnosis of bladder urothelial carcinoma and was treated by early radical surgery and chemotherapy,which led to longterm disease control and preservation of quality of life.
A 60-year-old gentleman,a known case of metastatic adenocarcinoma prostate for the last 3 years,presented to us with complaints of gross,total painless hematuria with passage of clots of 3 months duration.His serum prostatespecific antigen(PSA)at initial presentation was 45.5 ng/dL and he had subsequently undergone ADT in the form of bilateral orchiectomy along with six cycles of docetaxel chemotherapy.One month after completion of docetaxel therapy,patient had achieved nadir PSA of 3.2 ng/dL,which gradually rose to 5.4 ng/dL,7.1 ng/dL,9.0 ng/dL,and finally to 11.4 ng/dL over the next 6 months.Tablet Abiraterone was then started for this patient at a dose of 1000 mg daily and the PSA again decreased to a nadir value of 1.2 ng/dL in the next 2 months.Patient was on regular follow-up at the center with monitoring of PSA levels for the next 12 months when he developed gross,total,painless hematuria and presented to us.Contrast enhanced computed tomography(CECT)scan of the abdomen revealed a strongly enhancing polypoidal mass lesion,measuring 6 cm×6 cm,in the left posterolateral wall of the bladder extending inferiorly to involve the prostate.There was bilateral pelvic lymphadenopathy,with the largest lymph node being 1.9 cm×1.8 cm in the left internal iliac region(Fig.1A-1C).Magnetic resonance imaging(MRI)showed a polypoidal bladder mass which was contiguous with the prostatic mass.Bilateral seminal vesicles and neurovascular bundles were involved(Fig.1D and 1E).Prostate-specific membrane antigen positron emission tomography computed tomography(PSMA PET CT)was done which showed no evidence of any distant metastases along with PSMA avid prostatic mass with intravesical component and pelvic lymphadenopathy(Fig.2).Cystoscopy showed a large polypoidal growth about 10 cm×7 cm arising from the left lateral wall,with multiple dilated blood vessels over the surface.Base of the growth showed multiple enlarged convoluted plexus of vessels.The growth was highly vascular with ooze from the entire surface and was bleeding on touch.Biopsy was taken from the growth which showed high grade lamina invasive transitional cell carcinoma(TCC)on histopathological examination(Fig.3).
Post-operative period was complicated by hematuria with clot retention needing multiple cystoscopic evacuations and serial fall in hemoglobin,so the decision to go ahead with cystoprostatectomy was taken.On exploration,there was a hard growth palpable in the bladder.There were multiple conglomerate lymph nodes presenting bilaterally,with the largest being 5 cm×5 cm present along the left internal iliac artery which was removed in toto ligation and division at the origin.Intra-operative frozen section of the bladder neck and the distal ureteric margins were done and confirmed to be free of tumor before proceeding with urinary diversion in the form of W-shaped orthotopicneobladder.The final histopathology report showed neuroendocrine prostate cancer with foci of adenocarcinoma with metastases to bilateral pelvic lymph nodes(Fig.4A-4C).Bilateral seminal vesicles as well as the lateral surgical margins of the prostate were involved by the tumor.Immunohistochemistry showed positive staining for chromogranin,synaptophysin,and PSA,confirming the diagnosis of neuroendocrine tumor of prostate(Fig.4D and 4E).As per the histopathology report,patient was planned for adjuvant chemotherapy and local radiotherapy.He received six cycles of etoposide and carboplatin and 72 Gy external beam radiotherapy to the prostatic bed.
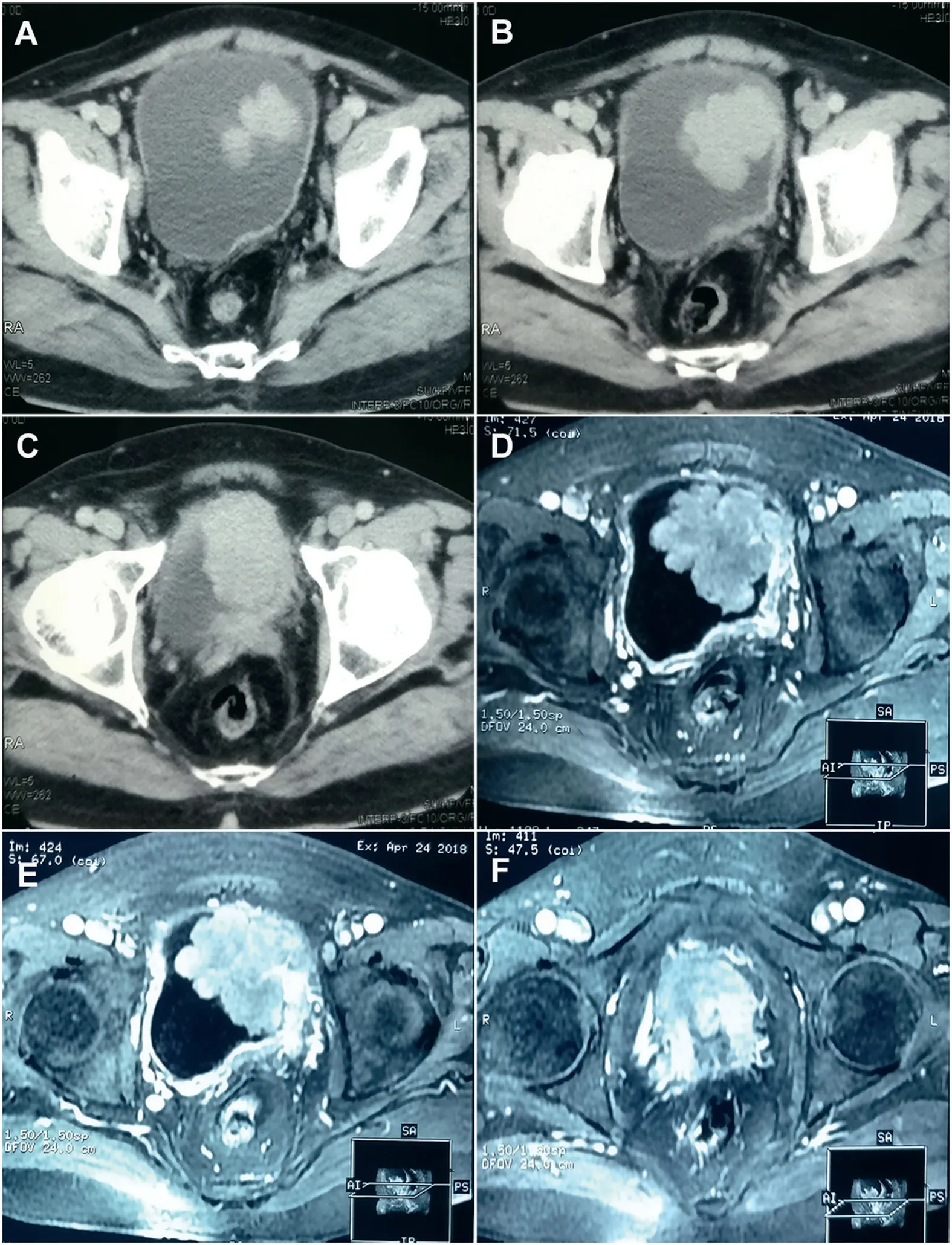
Figure 1 Cross sectional imaging showing locally advanced bladder tumour involving the prostate also.(A-C)Serial sections of contrast enhanced computed tomography images showing enhancing polypoidal intraluminal mass arising from the left lateral wall of the urinary bladder;(D-F)Magnetic resonance images showing the polypoidal mass arising from the urinary bladder wall and contiguous with the prostatic mass below.The seminal vesicles were involved bilaterally and bilateral pelvic lymph nodes are enlarged.
At 6 months follow-up,patient had PSA of 0.02 ng/dL.He was completely continent and did not have any evidence of disease on PET scan.At 2 years post-operation,patient continues to have a PSA level of 0.01 ng/dL without any evidence of disease recurrence on functional and crosssectional imaging.
The increased use of second-line androgen receptor(AR)targeted therapies in treatment of prostate cancer in castrate na?¨ve setting[3,4]has led to the development of a distinct clinical and histologic subtype of castrate resistant prostate cancer called t-NEPC.Developing as aconsequence of lineage plasticity,these tumors are completely resistant to standard ADT and are highly metastable and invasive[5,6].Since therapeutic resistance is an universal phenomenon in prostate cancer,it would not be unwise to assume that t-NEPC represents a large proportion of patients of CRPC who are progressing on second-line AR targeted treatment.Biopsies from metastatic sites in such patients have demonstrated t-NEPC in 10%-20%[7-9].Usually the patients present with exclusively visceral or predominantly lytic bony metastases with bulky tumor masses and a low PSA level relative to the tumor burden or a short duration of response to AR targeted therapy[10,11].Our patient presented with hematuria,due to a polypoidal bladder mass.The PSA levels were low,but functional imaging and cross-sectional imaging did not reveal any soft tissue or bony metastases apart from the pelvic lymphadenopathy,which was persistent from the time of initial diagnosis.Serum carcino embryonic antigen(CEA)levels have been shown to be elevated in cases of t-NEPC.We did not check the same as we did not have any reason to suspect neuroendocrine differentiation.t-NEPC is a very aggressive phenotype and has a uniformly poor prognosis.In a literature review of 123 t-NEPC patients,the time to development of t-NEPC from initial diagnosis of PCa was 20 months,and the median survival after t-NEPC was just 7 months[2].Although the first-line cytotoxic chemotherapy in the treatment of prostate carcinoma is docetaxel,the treatment of t-NEPC involves a platinum-based regimen similar to that used for small cell carcinoma of the lung.Based on multiple phase II trials,National Comprehensive Cancer Network(NCCN)recommends using a combination of either cisplatin or carboplatin with etoposide or enrolment in a clinical trial for the treatment of such tumors[2,10,12,13].Most patients enrolled in these trials had disease burdens and clinical features typical of t-NEPC.Our patient did not have any distant metastases and no soft tissue metastases apart from pelvic lymphadenopathy,so the option of biopsy from the primary site to detect variant histology was not available to us.Also the presence of an aggressively bleeding bladder mass,showing features of TCC on histopathology,made us consider this to be a more likely cause of cancer related morbidity and mortality to the patient than his prostate cancer which was apparently under control.Therefore,we planned to do a palliative cystoprostatectomy with urinary diversion.In our experience even patients with limited life expectancy have a good quality of life with orthotopic neobladder urinary diversion.Furthermore,our patient was in good general condition and had Eastern Cooperative Oncology Group(ECOG)1 performance status[14].Therefore,we made a W-shaped pouch with serous lined extramural uretero-ileal anastomosis for urinary diversion.In a study by Aparicio et al.[10],113 patients were initially administered carboplatin and docetaxel for four cycles and more than 90% of the patients went on to receive second-line chemotherapy and showed disease progression even after that.Since our patient had already completed docetaxel based therapy and had progressed after that,it was decided that a course of carboplatin and etoposide should be administered.At the time of submitting this report,our patient continues to be on follow-up of 24 months and is free from serological or metastatic disease progression.
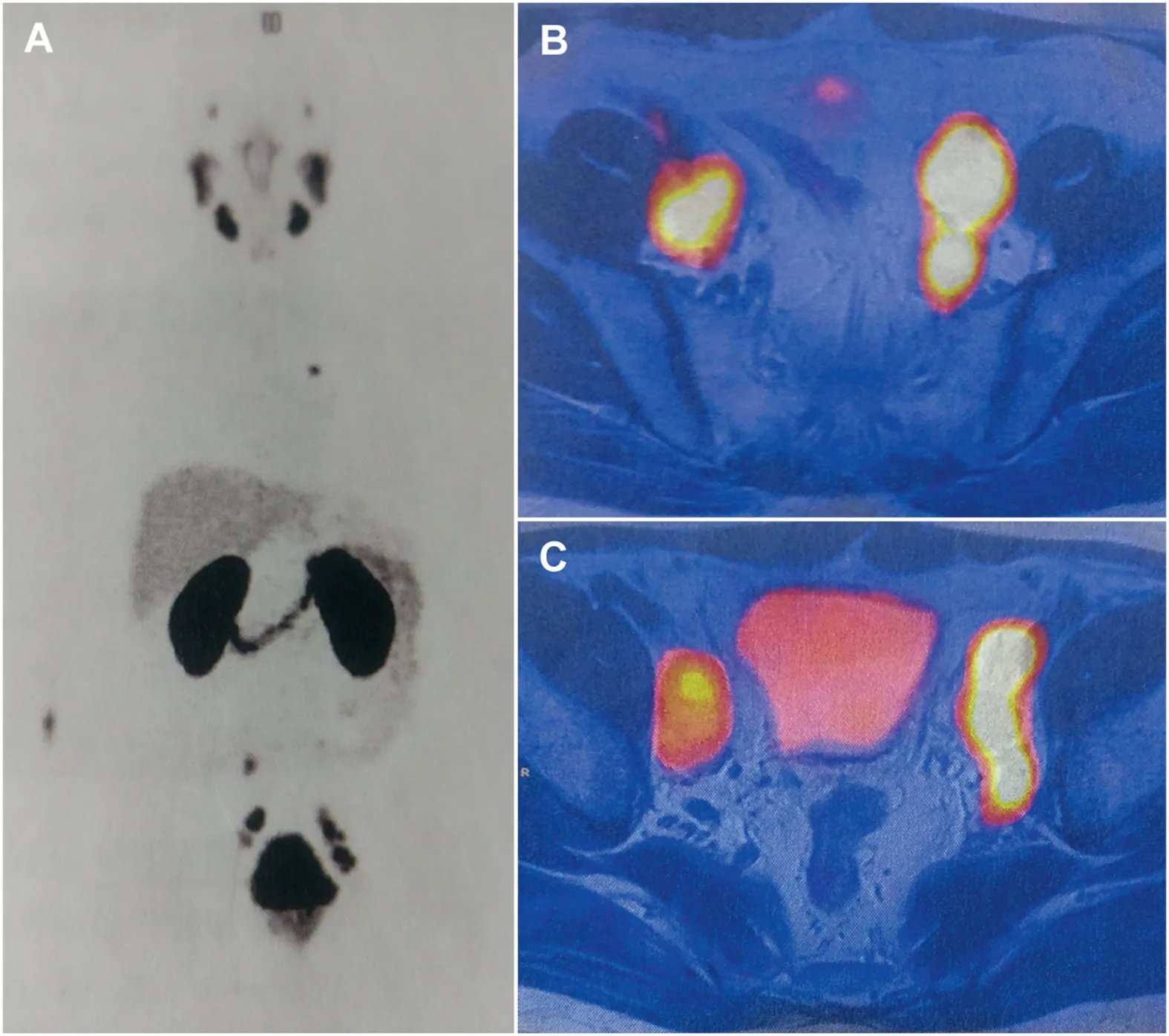
Figure 2 PSMA PET scan images.(A)Maximum intensity projection images showing a single area of uptake in the aortopulmonary node which was later shown to be inflammatory in nature based on its tracer avidity;(B and C)PSMA PET scan showing bilateral PSMA avid pelvic lymphadenopathy.PSMA PET,prostate-specific membrane antigen ositron emission tomography.
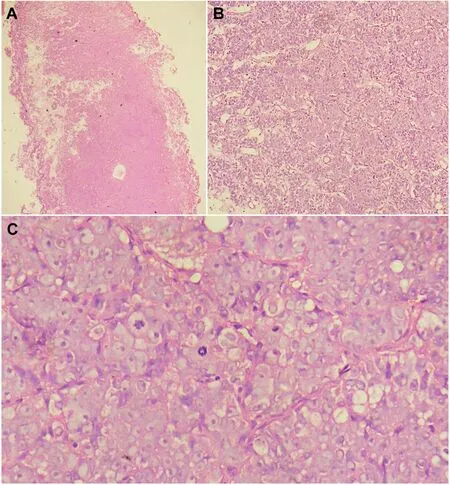
Figure 3 Sections of histopathological examination of the transurethral biopsy specimen.(A)HE stained sections 100×magnification,Low power view showing tumour infiltrating the prostate;(B)Tumour arranged in nests separated by thin fibrovascular septae(HE stain,200×magnification);(C)Oil immersion view showing moderately pleomorphic tumour cells with prominent nucleoli and brisk mitotic activity(HE stain,1000×magnification).HE,hematoxylin and eosin.
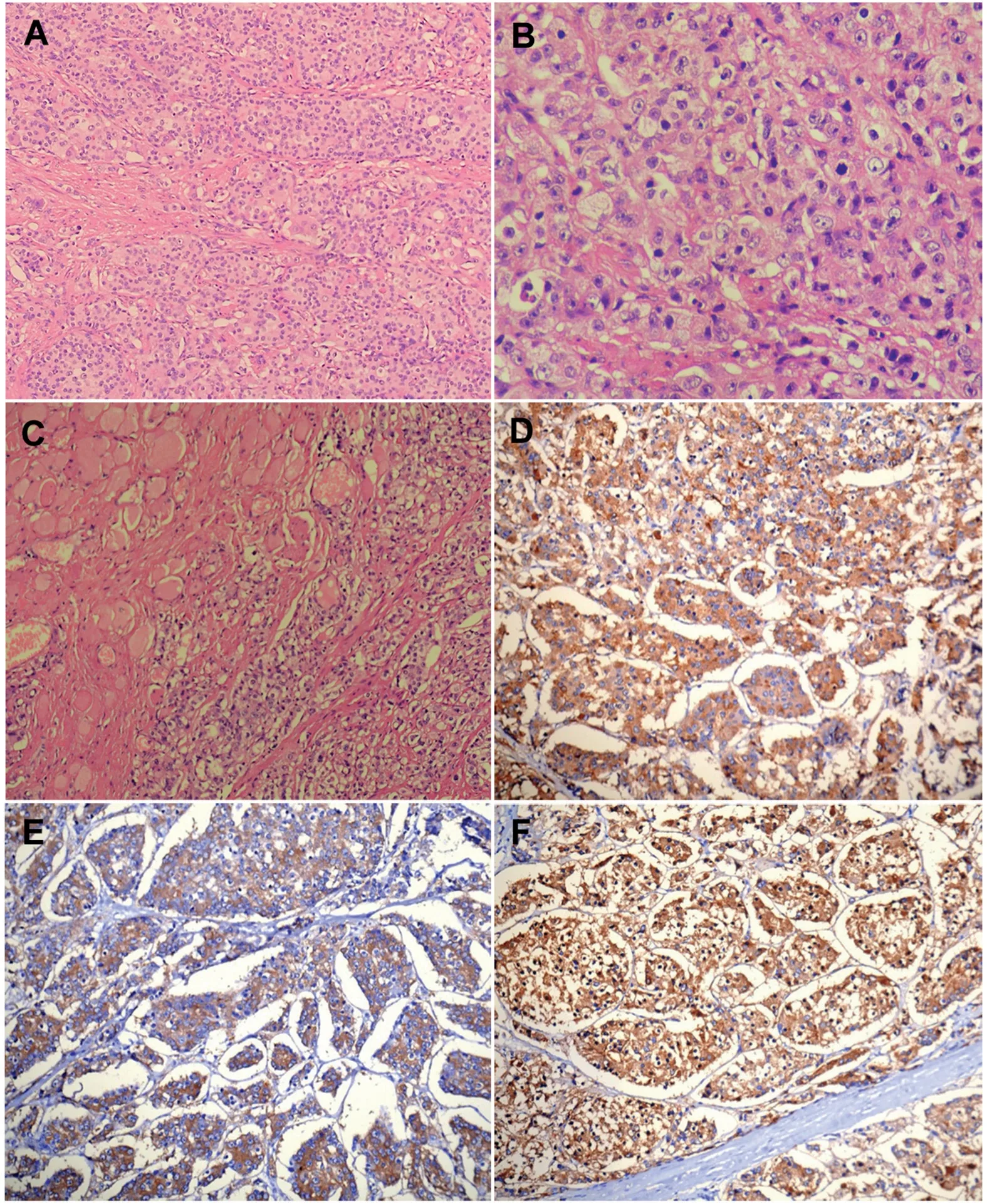
Figure 4 HE and immunohistochemistry stained sections of the tumour from the resected surgical specimen.Top row:Mildly pleomorphic to isomorphic tumour cells arranged in nested configuration(200×magnification)(A);Tumour cells showing moderate nuclear atypia(400×magnification)(B);Periprostatic skeletal muscle infiltration by the tumour(200×magnification)(C).Bottom row(200×magnification):Microphotographs showing positive immunostaining for synaptophysin(D),chromogranin(E),and prostate-specific antigen(F).HE,hematoxylin and eosin.
While the treatment done by us is not the standard of care for this type of prostate cancer,it provided the patient relief from symptoms and the subsequent local disease control and cytoreduction probably helped in the response to carboplatin based therapy.Though treatment of the primary lesion has not been described in the castrate resistant setting,local therapy in the setting of metastatic prostate cancer is being investigated in the ongoing TROMBONE trial and the recently published HORRAD trial[15,16].The favorable results seen in our case may need to be validated in larger studies examining the effect of treatment of the primary site in patients of castrate resistant prostate cancer with bulky local disease and small distant metastatic burden.We would like to conclude by saying that rarely t-NEPC may present with symptoms of hematuria and bladder outlet obstruction without stigmata of metastatic bony or visceral disease.Poorly differentiated tumors may be mistaken for TCC.In such patients,radical local treatment with aggressive post-operative platinum-based chemotherapy may help in extending survival.
Author contributions
Study design:Rahul Jena,Nandita Chaudhary,Uday Pratap Singh.
Data acquisition:Rahul Jena,Uday Pratap Singh,Nandita Chaudhary,Hira Lal.
Data analysis:Rahul Jena,Hira Lal.
Drafting of manuscript:Rahul Jena,Uday Pratap Singh.
Critical revision of the manuscript:Uday Pratap Singh,Hira Lal.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2021年4期
Asian Journal of Urology2021年4期
- Asian Journal of Urology的其它文章
- Late upper urinary tract urothelial carcinoma following radical cystectomy,presenting as page kidney
- Metachronous chest wall metastasis from clear cell renal cell carcinoma-A rarity
- Perioperative anticoagulation and open distal corpora cavernosa shunt in the management of a case of stuttering idiopathic persistent childhood ischaemic priapism
- Effect of tamsulosin versus tamsulosin plus tadalafil on renal calculus clearance after shock wave lithotripsy:An open-labelled,randomised,prospective study
- A novel spherical-headed fascial dilator is feasible for second-stage ultrasound guided percutaneous nephrolithotomy:A pilot study
- Impact of COVID-19 on endourology surgical practice in Saudi Arabia:A national multicenter study
