Tension hydropneumothorax in a Boerhaave syndrome patient: A case report
Chun-ting Wang, Hui Jiang, Joseph Walline, Yan Li, Jian Wang, Jun Xu, Hua-dong Zhu
1 Emergency Department, Peking Union Medical College Hospital, Beijing 100730, China
2 Emergency Department, Civil Aviation General Hospital, Beijing 100123, China
3 Accident and Emergency Medicine Academic Unit, the Chinese University of Hong Kong, Hong Kong 999077, China
4 Department of Radiology, Peking Union Medical College Hospital, Beijing 100730, China
Dear editor,
Boerhaave syndrome, firstly described by Hermann Boerhaave in 1724, is a rare and life-threatening condition characterized by spontaneous transmural tear of the oesophagus.[1]The early diagnosis of Boerhaave syndrome is extremely important since a delay in the diagnosis can increase the mortality rate.[2]Here, we reported a Boerhaave syndrome patient combined with tension hydropneumothorax.
CASE
A 48-year-old man was brought to our emergency department (ED) complaining of epigastric pain,vomiting, dark-colored stools for one day, and worsening chest pain for nine hours.He previously had been well.
His symptoms began one day prior to the arrival in ED with nausea followed by several episodes of forceful emesis, then progressed to black-colored stools and intermittently vomiting black-colored material.About nine hours prior to the arrival in ED, the patient developed persistent lower thoracic and upper abdominal pain associated with dizziness, fatigue, and dyspnea.Social history was remarkable for 1,000 mL daily intake of alcoholic spirits for the past seven years.Physical examination revealed a middle-aged male in obvious painful distress, afebrile, tachycardia (168 beats per minute) with normal blood pressure (BP, 109/47 mmHg[1 mmHg=0.133 kPa]) and rapid respiratory rate (35 breaths per minute), and pulse oximetry cannot be measured.
Five minutes after arrival to our ED, he vomited once again, followed by a sudden loss of consciousness with no palpable pulses.Cardiopulmonary resuscitation(CPR) was started immediately.After 13 minutes of resuscitation, including mask ventilation for three minutes, endotracheal intubation, and positive pressure ventilation, the patient was successfully resuscitated(heart rate 156 beats per minute, oxygen saturation[SpO2] 91% on 100% fraction of inspired oxygen [FiO2],and BP 87/56 mmHg).
On examination, the patient had both midrange neck swelling and subcutaneous crepitation.His abdomen was diffusely tender with normoactive bowel sounds.Arterial blood gas was as follows: pH 7.02, partial pressure of carbon dioxide (PCO2) 54 mmHg, partial pressure of oxygen (PO2)53 mmHg, and serum lactic acid 12.6 mg/dL.The white blood cell count was 6.37×109/L.The red blood cell was normal (117 g/L).Potential kidney injury was noted by an elevated serum creatinine (2.6 mg/dL) and blood urea nitrogen (66 mg/dL).The levels of glucose (8.8 mmol/L)and potassium (5.1 mmol/L) were slightly elevated.Mallory-Weiss syndrome or aortic dissection was initially suspected,so an aortic-enhanced computed tomography (CT) was performed.The image indicated subcutaneous emphysema,mediastinal emphysema, bilateral pleural cavity-free air, and large left-sided hydropneumothorax with the air around the esophagus (Figure 1).These findings strongly suggested spontaneous esophageal perforation.
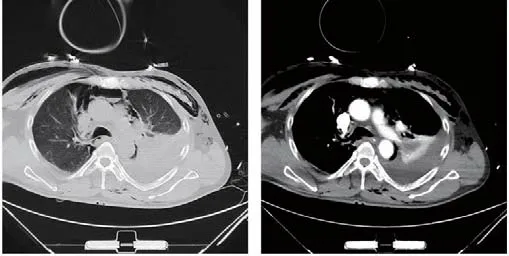
Figure 1.The aortic-enhanced computed tomography performed on the patient.
During resuscitation, 520 mL of black-colored fluid was extracted via a nasogastric tube.The left-sided emergent closed thoracic drainage with a 32-F chest tube was then performed, which produced about 650 mL of thick and black-colored fluid.The patient received intravenous hydration, large doses of vasopressors,and broad-spectrum antibiotics.Emergent surgery was considered, but given the patient’s condition and high surgical risk, his son refused further interventions.The patient died due to acute circulatory failure within 24 hours after ED arrival.
DISCUSSION
In practice, the “H’s and T’s” are potentially reversible causes of cardiac arrest.Timely correction of a reversible cause of cardiac arrest may lead to a good prognosis.[3]Cardiac arrest in this case may attribute to several different factors.Firstly, it is reasonable that acidosis from shock and hypoxia causes cardiac arrest.Secondly, tension pneumothorax, a complication of spontaneous esophageal rupture, can also cause cardiac arrest.It is likely that our patient suff ered cardiac arrest due to tension hydropneumothorax.In addition, the possibility of cardiac arrest caused by circulatory shock should also be considered.
Boerhaave syndrome is usually associated with the excessive indulgence of food or alcohol.Our patient initially had dark-colored vomitus with a past medical history of alcoholism, which may suggest spontaneous esophageal rupture.Prolonged alcohol use can lead to severe vomiting.The study showed that lower esophageal tears might involve a spectrum of disease from Mallory-Weiss syndrome to full-thickness perforation.[4]Autopsy examinations revealed that a Mallory-Weiss tear caused by barotrauma from severe vomiting or air insufflation during endoscopy might evolve into a full-thickness rupture.[5]
A delay in diagnosis and treatment of Boerhaave syndrome is associated with significantly higher morbidity and mortality.CT abnormalities in Boerhaave syndrome include extraluminal air, peri-esophageal fluid, esophageal thickening, and extraluminal contrast.These CT findings can be the first clue to the diagnosis of esophageal perforation.[6]Contrast CT is considered the ‘‘golden standard’’ for diagnosing spontaneous esophageal rupture in suspected patients.[7]Traditionally,an esophagram performed with a water-soluble contrast agent can be helpful for the diagnosis of Boerhaave syndrome.Suzuki et al[8]reported a case of Boerhaave syndrome that was confirmed via thoracic drainage,which revealed bloody fluid and food residue in the drainage bag.Therefore, thoracic drainage can be used as a strategy for diagnosis and treatment in some cases.
The reported mortality rate of esophagus perforation is estimated to be 35%-40%.A favorable prognosis is associated with early definitive surgical treatment within 12 hours of rupture.If the intervention is delayed above 24 hours, the mortality rate (even with surgical intervention) rises to over 50% and reaches nearly 90%after 48 hours.If left untreated, the mortality rate is close to 100%.[8,9]Endoscopic stent insertion provides a promising approach for some Boerhaave syndrome patients, but it is associated with a high rate of treatment failure and further surgical intervention.[10]Prompt surgical repair and drainage can play an important role in management.[11]
This case presented with Mackler’s triad, tension hydropneumothorax and cardiac arrest, and was confirmed to have Boerhaave syndrome on contrast CT and through thoracic drainage within 12 hours of ED arrival.Even though initial resuscitation efforts were successful, he still died of acute circulatory failure.While paying attention to the possibility of Mallory-Weiss syndrome, aortic dissection, or gastrointestinal bleeding,hydropneumothorax should alert providers to the possibility of Boerhaave syndrome.Thoracic drainage is a useful measure to conf irm Boerhaave syndrome rapidly and can relieve pressure inside the thoracic cavity.The lack of prompt treatment can significantly increase morbidity and mortality despite a timely diagnosis.
Funding:None.
Ethical approval:The study was approved by the Ethics Committee of the hospital.
Conflicts of interest:The authors declare that there are no conf licts of interest regarding the publication of this paper.
Contributors:CTW and HJ contributed equally to this work.All authors contributed substantially to the writing and revision of this manuscript and approved of its contents.
 World journal of emergency medicine2021年3期
World journal of emergency medicine2021年3期
- World journal of emergency medicine的其它文章
- Chemical pneumonitis caused by intravenous injection of insecticide spray
- Myocardial infarction detected by a smartwatch after transcatheter aortic valve replacement during the COVID-19 pandemic
- Mediastinum metastasis in a post-surgical pancreatic cancer patient successfully conf irmed with endoscopic ultrasonography
- Biphasic anaphylaxis manifested as type I Kounis syndrome induced by ingestion of raw f ish gallbladder: A case report
- Performance of extracorporeal membrane oxygenation in patients with fatal paraquat poisoning:grasp for straws?
- Intravenous haloperidol for the treatment of intractable vomiting, cyclical vomiting, and gastroparesis
