Strategies and outcomes in severe open tibial shaft fractures at a major trauma center: A large retrospective case-series
Kavi H Patel, Karl Logan, Matija Krkovic
Kavi H Patel, Karl Logan, Matija Krkovic, Department of Trauma & Orthopaedics, Cambridge University Hospitals NHS Trust, Cambridge CB2 0QQ, United Kingdom
Abstract BACKGROUND Severe open tibia fractures are challenging to treat with a lack of published clear management strategies.Our aim was to provide an overview of the largest singlecenter experience in the literature, with minimum 1-year follow-up, of adult type 3 open tibial shaft fractures at Cambridge University Hospitals (a United Kingdom major trauma center).We sought to define patient characteristics and our main outcome measures were infection, union and re-fracture.AIM To retrospectively define patient and injury characteristics, present our surgical methods and analyze our outcomes–namely infection, union and re-fracture rates.METHODS Consecutive series of 74 patients with 75 open tibial fractures treated between 2014 and 2020 (26 classified as Gustilo-Anderson 3A, 47 were 3B and two were 3C).Nine patients underwent intramedullary nailing (IMN), 61 underwent Taylor spatial frame (TSF) fixation and 5 were treated with Masquelet technique (IMN and subsequent bone grafting).RESULTS Mean follow-up was 16 mo (IMN) and 25 mo (TSF).We had an infection rate of 6.7% (5), non-union rate of 4% (3) and re-fracture rate of 2.7% (2).Average time to union was 22 wk for IMN and 38.6 wk for TSF.Thirty-three cases had a bone defect with a mean of 5.4 cm (2-11).Patient age, sex, diabetes, smoking status or injury severity did not have a significant effect on union time with either fixation method.Our limb salvage rate was 98.7%.CONCLUSION Grade 1 to 3A injuries can effectively be treated with reamed or unreamed IMN.Grade 3B/C injuries are best treated by circular external fixators as they provide good, reproducible outcomes and allow large bone defects to be addressed via distraction osteogenesis.
Key Words: Tibia; Open fracture; Taylor spatial frame; Intramedullary nailing; Bone defect
INTRODUCTION
Severe open tibia fractures remain challenging to treat with long-term social, physical and financial implications.They are the most common long bone fractures, with a higher incidence in working-age males and are often associated with polytrauma[1].These high-energy fractures are often mutlifragmentary with extensive soft tissue disruption and require a multidisciplinary ortho-plastics approach.The publication of British Orthopaedic Association Standards for Trauma (BOAST 4) in 2009 and the introduction of the Major Trauma Network in 2010 have unquestionably improved outcomes in open tibia fractures[2].
Circular external fixators (CEF) such as the Taylor spatial frame (TSF) (Smith & nephew, Memphis, TN, United States), a multiplanar computer-assisted hexapod system, have been shown to result in good functional and radiological outcomes following severe open tibia fractures[3].Alternatively, both reamed and unreamed intramedullary nailing (IMN) are established treatment options with comparable surgical outcomes in experienced hands[4].More complex injury patterns, such as segmental fractures or where critical post-traumatic bone defects are present, provide their own challenges.In these cases, special techniques must be considered; for example, the induced membrane Masquelet technique[5].
Several crucial aspects in the surgical management of these patients remain equivocal with no clear guidelines and therefore, proceeding with evidence-based interventions is essential.We sought to retrospectively define patient and injury characteristics, present our surgical methods and analyze our outcomes–namely infection, union and re-fracture rates.To the best of our knowledge, we present the largest single-center experience of type 3 open tibial shaft fractures, with 1-year minimum follow-up, in the literature.
MATERIALS AND METHODS
Using our local electronic database, we retrospectively identified 74 adult patients with 75 GA type 3 open tibial shaft fractures who underwent treatment between October 2014 and February 2020 at Cambridge University Hospitals NHS Trust, a large level 1 trauma center.We recorded patient demographics, fracture type, mechanism of injury, timing and number of operations, time to union, infection, refracture and complications.The influence of patient characteristics on healing was also analyzed.There were 54 males and 24 females with a mean age of 43.1 (18-83).The fractures were classified according to the Gustilo-Anderson and Orthopaedic trauma association (OTA) grading systems.All intra-articular fractures were excluded with the majority of fractures diaphyseal (58, 77%), although metaphyseal fractures around the knee (3, 4%) and ankle (14, 19%) were included.Patients who required primary amputation due to injury severity (2 patients) or had less than 12 mo follow-up were excluded.
All patients received intravenous antibiotics in the Emergency Department and 68 patients (91.9%) initially underwent damage control procedures with debridement, lavage and skeletal stabilisation within 24 h of presentation.The remaining six underwent IMN as their primary procedure.Definitive surgery was performed at a mean of 22 d (0-45) from admission with timing dependent on patient physiology and soft tissue condition.All patients were treated by a single surgeon specializing in trauma and limb reconstruction with access to a dedicated team of nurses and physiotherapists.Plastic surgeons were involved on admission and soft tissue coverage was performed at a mean of 9.3 d (1-41) from injury on a combined ortho-plastics list.Soft tissue coverage comprised a free flap in 60 cases (80%; gracilis, latissimus dorsi or anterolateral thigh), local flap in 10 (10.7%) and split skin graft in 5 cases (6.7%).Two patients had injury to the posterior tibial artery which required urgent bypass grafting by the vascular surgeons.
Definitive surgery was either with TSF or IMN depending on patient factors (e.g.,compliance, age), fracture pattern and soft tissue condition (GA severity).Weightbearing was commenced where possible depending on fracture configuration and other injuries.Patients with reduced mobility were given venous thromboembolism prophylaxis.Where required, a low-energy corticotomy was performed at the time of TSF application with bone transport starting on day 8 post-op.Fracture malalignment was corrected during outpatient clinics and regular pin-site care was adhered to.Twelve patients required further TSF adjustment in the operating theatre.Five patients with bone defects were treated using the described induced membrane Masquelet technique with aggressive debridement, use of the reamer/irrigator/aspirator (RIA, DePuy Synthes, West Chester, PA, United States) for bone graft harvesting, antibioticloaded cement and calcium sulphate beads[6].The mean interval between 1stand 2ndstages was 16.8 wk (9-27).
Fracture union was defined as evidence of bridging trabeculae seen on three cortices on plain radiographs or computed tomography (CT).The absence of pain following frame dynamization was also considered indicative of union.In those who underwent bone transport, regenerate of sufficient quality on radiographs was also required prior to frame removal.Infection was defined as the identification of organisms on two or more tissue samples.Antibiotic treatment was led by a microbiologist.
Statistical analysis was carried out using GraphPad (GraphPad Software Inc, San Diego, CA, United States).Descriptive statistics for means, ranges and frequency are provided.Analysis of categorical data was performed using the Mann-WhitneyUtest and continuous variables using Spearman’s correlation coefficient.APvalue < 0.05 (two-tailed) was considered significant.
RESULTS
Patient demographics are presented in Table 1.Of the 75 fractures, 26 were classified as GA 3A, 47 were 3B and two were 3C.OTA classification was also recorded (Table 2).61 fractures were treated with TSFs, 9 were treated with IMN and 5 were treated using the Masquelet technique with IMN and subsequent bone grafting.72 fractures went on to union after primary surgery.Average time to union was 22 wk for IMN (excluding those who underwent the Masquelet technique) and 38.6 wk for TSF (Table 3).
We treated 11 segmental fractures (3 with IMN and 8 with TSF) with a mean union time of 48.9 wk.The mean number of operations prior to IMN and TSF was 0.5 (0-1) and 2.2 (1-5) respectively.Thirty-three cases had a bone defect with a mean of 5.4 cm (2-11).Mean follow-up was 16 mo (13-26) for IMN and 25 mo (15-38) for TSF.
Two of the 5 fractures treated with the Masquelet technique developed infections which required revision procedures (both TSFs) (Table 4).A total of 5 patients, all of whom had GA 3B fractures, developed post-operative infections (Table 5).Three patients (all of whom were treated with TSFs) developed non-unions.All progressed to union following revision procedures (Table 6).Two patients treated with TSFs went on to re-fracture at the docking site, following removal of frame (Table 7).Both refractures occurred despite CT evidence of bony union and one had previously been treated for an infected non-union.Patient age, sex, diabetes, smoking status or injury severity (based on GA classification) did not have a significant effect on time to union with either fixation method.One patient, following fracture union with TSF, underwent amputation at another hospital due to chronic intractable pain.

Table 3 Time to union based on fixation method and fracture type
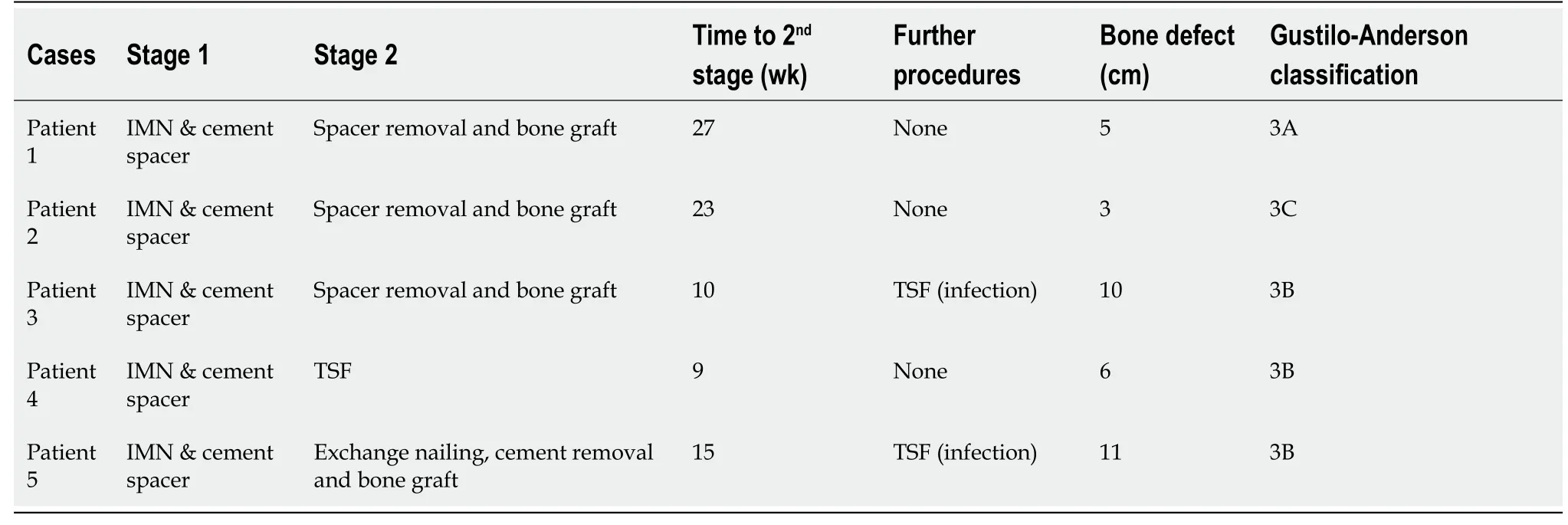
Table 4 Summary of patients treated with Masquelet technique
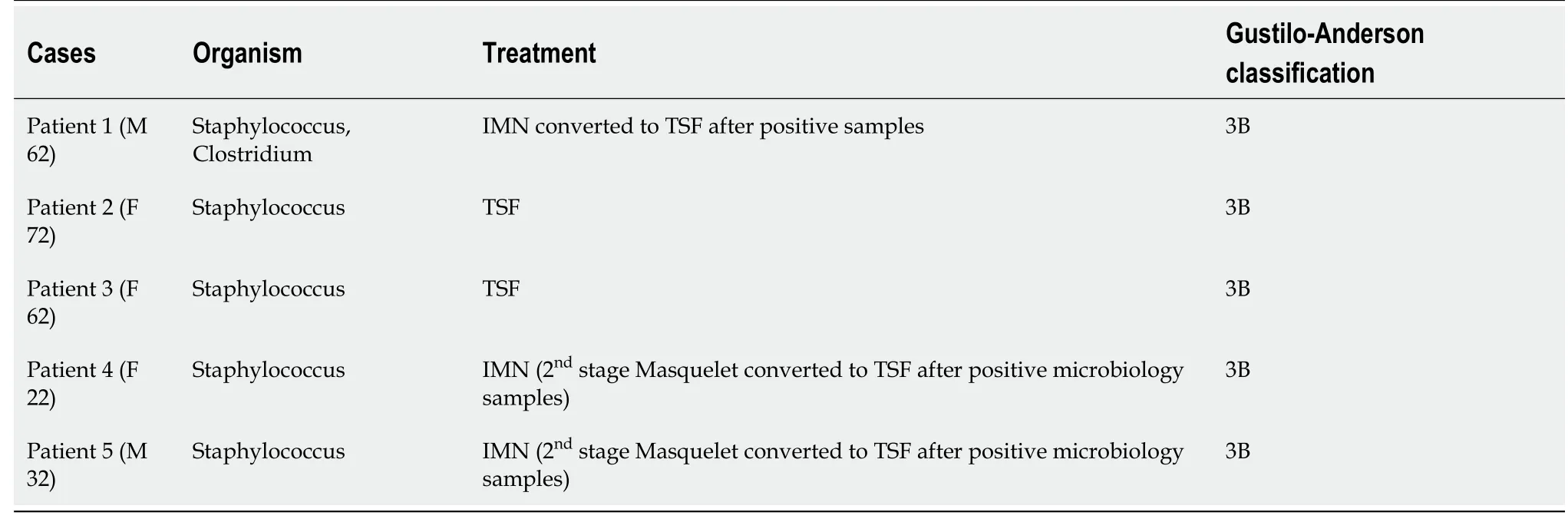
Table 5 Treatment of infected cases
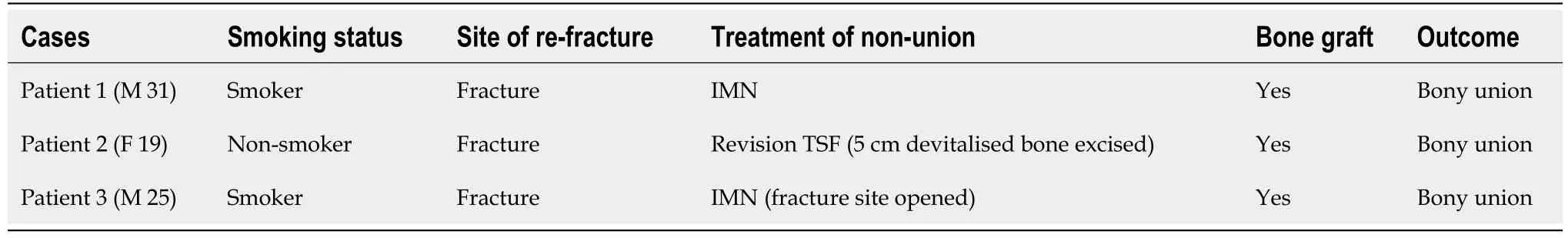
Table 6 Treatment of non-union following Taylor spatial frame application
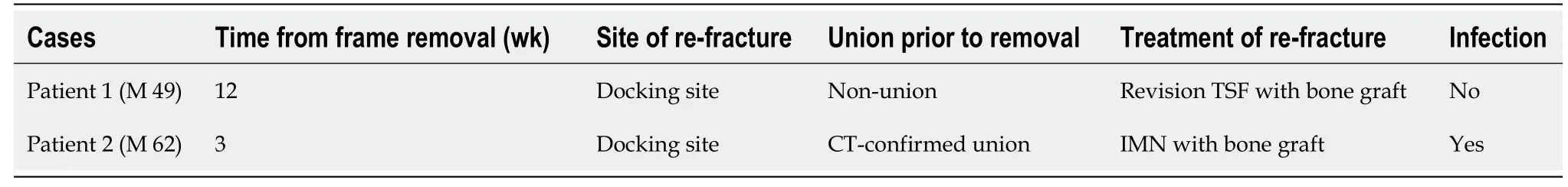
Table 7 Re-fracture following Taylor spatial frame removal
DISCUSSION
Severe open tibial shaft fractures are often associated with high-energy polytrauma and consequently are managed according to Advanced Trauma Life Support guidelines.Several studies have shown these fractures to be associated with rates of chronic infection and non-union as high as 38% and 50% respectively[7,8].Our study shows that it is possible to achieve good results with a timely multi-disciplinary approach and careful soft tissue management, as evidenced by our deep infection rate of 6.7%, non-union rate of 4% and re-fracture rate of 2.7%.
Although the timing of initial debridement is controversial[9], we believe aggressive soft tissue debridement by an experienced surgeon and damage control with temporary external skeletal stabilisation within 24 h of injury is critical.The BOAST 4 standards of care recommend definitive soft tissue closure or cover within 72 h, however, 90.1% of our patients waited longer than this.This was because a significant proportion of our patients required prolonged intensive care admission which inevitably delayed surgery.Our use of negative-pressure wound therapy (VACa) in open fractures until definitive soft tissue closure is well supported in the literature[10].Early prophylactic antibiotic therapy in patients with open fractures results in a relative risk reduction of 59% for acute infection and consequently all our patients received 1.2 g intravenous co-amoxiclav (or clindamycin if penicillin allergic) as early as possible after injury and until definitive soft tissue closure[11,12].We recommend the use of antibiotic-impregnated calcium sulphate beads (Stimulana, Biocomposites Inc, Wilmington, NC, United States) in type 3 open fractures where there is a bone defect as this has shown to reduce infection rate (6.5% vs 20.6%, P < 0.001)[13].We found that age, smoking, diabetes and GA severity had no significant effect on infection rate and this has been reflected in other studies[3].Wordsworth et al[2] reported a deep infection rate of 1.6%, however, two of our patients who developed deep infection were treated with the induced membrane technique for bone transport which we have found to have an unacceptably high failure rate as previously described[2,6].Adjusting for this, our infection rate would be in line with most other studies.
In our study, the majority of patients who underwent IMN fixation had GA type 3A fractures (71.4%).Several studies have shown IMN fixation to be associated with high union, low infection and low re-operation rates in GA type 1 to 3A tibial shaft fractures[14,15].Inanet al[16] reported a significantly shorter time to union (19 wkvs21 wk,P= 0.04) with IMN compared to Ilizarov fixation in GA type 3A fractures although there was no difference in deep infection[16].Our results show that IMN fixation leads to a faster union time than TSF in GA type 3A fractures (25.9 wkvs41.1 wk), however, comparison is difficult as fractures treated with TSF tended to be more complex.All patients who were treated with temporizing external fixation prior to IMN fixation were converted within 14 d as this has been shown to be important in the prevention of deep infection[17].We prefer reamed IMN although there is no clear evidence showing this to be superior to unreamed IMN in open tibia fractures[18].
Studies that have shown higher rates of non-union and infection with external fixation compared to IMN have only included monolateral external fixators which are biomechanically inferior to CEF[19].A meta-analysis of five randomized controlled trials concluded that IMN was the more effective treatment for GA type 3 fractures due to the lower incidence of infections.In that study however, monolateral external fixators and CEF were grouped together and fracture classifications were not consistently specified[20].Our mean TSF union time of 38.6 wk is longer than that reported in other studies (25-26 wk)[3,21].This is explained by the fact that 28 cases (45.9%) had significant bone loss requiring distraction osteogenesis.Furthermore, 25 patients (33.8%) presented with polytrauma which prolonged post-operative rehabilitation and consequently, union time.Of 61 patients treated with TSF, 3 developed aseptic non-union (4.9%), which is comparable to other studies[21,22].Two of these, both smokers, underwent exchange nailing and the third, re-application of TSF.All went on to unite.Assessing functional outcome was beyond the scope of our study, however, the literature suggests that CEF yields good functional outcomes in the majority of cases in GA type 3 fractures[23].
In the presence of critical bone loss, we found that treatment with TSF provides a safe and reliable method of regenerating significant quantities of boneviadistraction osteogenesis following an osteotomy at a site away from the fracture.Our bone healing index (time to bony union divided by length of bony defect) was 56 d/cm.This did not necessarily correlate with when bone regenerate was considered strong enough for frame removal.Other authors have reported similar results[24].We therefore advocate early resection of devitalized bone, as this reduces the risk of infection whilst still achieving good results with long transport distances.In selected cases of large bone loss, a protocol of debridement/PMMA spacer, soft tissue coverage, circular frame application, removal of spacer/corticotomy and distraction osteogenesis published by Hohmannet al[25] reported good outcomes[25].Open segmental diaphyseal fractures present their own challenges and, as reflected in our study, often result in longer times to union.A systematic review by McMahonet al[26] concluded that CEF provides the most satisfactory outcomes in this group of patients[26].
In our study, two patients sustained atraumatic re-fracture at the docking site following removal of TSF.In addition to autologous bone graft, one patient was treated with IMN and the other with re-application of TSF.A successful outcome was achieved in both patients.There is very little in the literature regarding re-fracture as a complication of CEF[27].
Our limb salvage rate was 98.7% which is consistent with other studies.Superficial pin site infection requiring oral antibiotics (20%) and ankle equinus (16%) were the most common complications with TSF treatment and both are well recognised[28].Importantly, pin site infection does not appear to translate into deep infection.We had no cases of symptomatic malunion and there were no further interventions required to correct malalignment.
Retrospective case-series have their limitations and despite being the largest singlecenter study of GA type 3 open tibia fractures, the study is not powered to promote one treatment over another with any certainty.Variations in fracture pattern, degree of bone loss and soft tissue management make comparison difficult.We look forward to the results of the FIXIT study, a prospective multicenter RCT comparing 1-year outcomes after treatment of severe open tibial shaft fractures with modern CEFvsinternal fixation in adults[29].Further study should include patient-reported outcome measures when comparing treatments.
CONCLUSION
Meticulous and aggressive debridement of GA type 3 open tibia wounds by experienced orthopaedic and plastic surgeons is paramount.Grade 1 to 3A injuries can effectively be treated with reamed or unreamed IMN.Grade 3B/C injuries are best treated by CEF as they provide good if not superior outcomes to other limb salvage techniques and allow large bone defects to be addressedviadistraction osteogenesis.In addition, TSF offers the advantages of postoperative adjustability.
ARTICLE HIGHLIGHTS
Research background
Open tibial fractures are a challenging injury to treat.They are often associated with high energy trauma and multiply injured patients.There is also a spectrum of severity of injury which makes it a challenge to establish clear treatment guidelines.
Research motivation
The motivation for this study was to assess the outcomes of a single surgeon treating open fractures in a level one trauma center.These injuries remain a challenge to manage and various treatment options are available and indeed used over the period studies.
Research objectives
We aimed to review the results of the treatment of these severe injuries.We chose infection, union and re-fracture rates as our primary outcome measures.We also sought to compare the outcomes of intramedullary nailing (IMN), Taylor spatial frame(TSF) and the Masquelet technique.
Research methods
This was a case series of 75 open tibial fractures in 74 patients treated over the course of six years by a single trauma surgeon in level one trauma center.We reviewed fracture type, mechanism of injury, timing and number of operations, time to union,infection, re-fracture and complication rates.Mann-Whitney U test and Spearman’s correlation coefficients were used for statistical analysis.Follow up time was 16 mo for intramedullary nails and 25 mo for TSF.
Research results
Of 26 injuries were classified as Gustilo-Anderson 3A, 47 were 3B and two were 3C.Nine patients underwent IMN, 61 underwent TSF fixation and 5 were treated with Masquelet technique.Infection rate was 6.7%, non-union rate was 4% and re-fracture rate was 2.7%.Average time to union was 22 wk for IMN and 38.6 wk for TSF fixation.Limb salvage rate was 98.7%
Research conclusions
Meticulous and aggressive debridement of Gustilo-Anderson type 3 fractures by experienced orthopaedic and plastic surgeons is paramount.Grade 1 to 3A injuries can effectively be treated with reamed or unreamed IMN.Grade 3B/C injuries are best treated using circular external fixation as this provide good if not superior outcomes to other limb salvage techniques and allows large bone defects to be addressed via distraction osteogenesis.In addition, this approach offers the advantages of postoperative adjustability.
Research perspectives
Further studies should be prospective, and ideally include patient recorded outcome measures, particularly if comparing the results of different treatments available for the fixation of open tibial fractures.
 World Journal of Orthopedics2021年7期
World Journal of Orthopedics2021年7期
- World Journal of Orthopedics的其它文章
- Arthrodesis of the first metatarsophalangeal joint: The “when and how”
- Arthroscopic removal as an effective treatment option for intraarticular osteoid osteoma of the knee
- Technological advancements in the analysis of human motion and posture management through digital devices
- Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation
