Optimization of transdisciplinary management of elderly with femur proximal extremity fracture: A patient-tailored plan from orthopaedics to rehabilitation
Alessandro de Sire, Marco Invernizzi, Alessio Baricich, Lorenzo Lippi, Antonio Ammendolia, Federico Alberto Grassi, Massimiliano Leigheb
Alessandro de Sire, Antonio Ammendolia, Department of Medical and Surgical Sciences, University of Catanzaro “Magna Graecia,” Catanzaro 88100, Italy
Marco Invernizzi, Alessio Baricich, Lorenzo Lippi, Physical Medicine and Rehabilitation, Department of Health Sciences, University of Piemonte Orientale, Novara 28100, Italy
Marco Invernizzi, Infrastruttura Ricerca Formazione Innovazione, Azienda Ospedaliera SS.Antonio e Biagio e Cesare Arrigo, Alessandria 15121, Italy
Federico Alberto Grassi, Massimiliano Leigheb, Orthopaedics and Traumatology Unit, Department of Health Sciences, University of Piemonte Orientale, Novara 28100, Italy
Abstract Fractures of femur proximal extremity (FFPE) are the most common fragility fractures requiring hospitalization, with a high risk of mortality, low independence in the activities of daily living and severe consequences on healthrelated quality of life.Timing for surgery has a key role in the management of elderly patients with FFPE as recommended by the Australian and New Zealand guidelines and the National Institute for Health and Care Excellence guidelines.Early surgery (within 48 h from hospital admission) allows significant benefits in terms of lower rates of postoperative complications and risk of death and can provide better functional outcomes.Therefore, time for surgery could be considered as a comorbidity marker.The choice between conservative or surgical approach surprisingly seems to be still not strongly supported by available literature, but it seems that both 30 d and 1 year risk of mortality is higher with the conservative treatment rather than with surgery.In light of these considerations, the optimization of FFPE management care is mandatory to improve functional outcomes and to reduce sanitary costs.Albeit it is widely accepted that transdisciplinary approach to patients suffering from FFPE is mandatory to optimize both short-term and long-term outcomes, the feasibility of a comprehensive approach in clinical practice is still a challenge.In particular, the large variability of figures involved could be considered both a resource and an additional disadvantage taking into account the difficulty to coordinate multidisciplinary approach covering care in all settings.Therefore, the aim of the present article was to summarize current evidence supporting transdisciplinary management of patients with FFPE, highlighting the benefits, feasibility and limitations of this approach.
Key Words: Transdisciplinary management; Elderly; Femur fracture; Hip fracture; Rehabilitation; Pathway
INTRODUCTION
Fractures of femur proximal extremity (FFPE) are the most common fragility fractures requiring hospitalization[1], with a high risk of mortality[2], low independence in the activities of daily living[3] and severe consequences on health-related quality of life[4].
FPE fracture patients are expected to increase worldwide due to the aging population and increasing average life expectancy[5,6], reaching 4.5 million by the year 2050, with detrimental issues on the health care system and sanitary costs[7].Kaniset al[8] recently reported a high variability in the incidence rate based on different countries, ranging from 439/100000 to 55/100000.According to the International Osteoporosis Foundation, women are mostly affected with a prevalence of 18% of hip fractures rather than 6% in men[9].
Aging is considered an independent, non-modifiable risk factor for fragility fracture, with over 90% of FFPE occurring in patients aged more than 65 years suffering from pre-existing medical comorbidities[10].Disability related to hip fractures is responsible for major health care expenditures resulting from both medical care and assistance that should be associated with the sanitary costs due to surgical procedures and hospitalization[11-13].Furthermore, a recent systematic review by Downeyet al[14] reported that hospitalization costs for hip fracture patients during the first year might be estimated as £14000 (€15900/$18750) per patient.
Taken together, all these findings highlight that the optimization of hip fracture management care is mandatory in order to improve functional outcomes and to reduce sanitary costs.To date, it is widely accepted that the transdisciplinary approach to patients suffering from hip fractures is mandatory in the correct management of this condition to optimize both short-term and long-term outcomes[15].More in detail, the Australian and New Zealand Guidelines[16] and the National Institute for Health and Care Excellence (NICE) guidelines[17] support a coordinated multidisciplinary approach covering care in all settings, from the ambulance to the discharge destination.Cornerstones of this approach were: Orthogeriatric assessment, optimi-zation of fitness for surgery, identification of rehabilitative goals, integration with related services including bone health and an adequate clinical and service governance responsibility for all stages of the pathway of care and rehabilitation.
Therefore, an adequate coordination of different figures including orthopaedic surgeons, physical and rehabilitation physicians, geriatric physicians, physical therapists and caregivers should be planned for hip fracture patients.
The aim of the present article was to summarize current evidence supporting transdisciplinary management of patients with fracture of the proximal extremity of femur, highlighting the benefits, feasibility and limitations of this approach.
ORTHOPAEDIC SURGERY TIMING
It is widely accepted that timing for surgery has a key role in FFPE management[18-20], as also affirmed by the NICE guidelines[17] that recommended that an early surgery (within the first day or next day from the admission) improved functional outcomes in older patients with FFPE.
In this scenario, a recent meta-analysis performed by Simunovicet al[21] assessed the effects of surgery performed within the 72 h controlling for comorbidities, reporting significant benefits in terms of risk of death and lower rates of postoperative complications.Despite previous large studies suggesting that time for surgery could be considered as a comorbidity marker[22,23], higher rate of mortality and complication were recorded in patients with surgical delay over 24 h[24].In contrast, a randomized controlled trial did not find significant differences between surgery performed within the first 6 h rather than within the first 24 h[25].
Albeit the early surgical approach is supported by high level of evidence according to both Australian and New Zealand[16] and NICE guidelines[17], the choice between conservative or surgical approach surprisingly seems to not be strongly supported by available literature.In particular, a Cochrane systematic review by Handollet al[26] reported several biases in studies supporting surgical management, and the limited available evidence did not show significant differences between conservative and surgical management.
A recent systematic review and meta-analysis[27] assessed randomized controlled trials comparing conservative and surgical treatment.The authors included seven observational studies with a total of 1189 patients reporting that both 30 d and 1 year mortalities were higher in the conservative group rather than the surgical group (odds ratio (OR): 3.95, 95% confidence interval (CI): 1.43-10.96; OR: 3.84, 95%CI: 1.57- 9.41).Unfortunately, functional outcomes and health-related quality of life were not assessed by these studies.
Altogether, these findings suggest that early surgical approach should be considered in elderly patients suffering from FFPE, taking into account the need for a transdisciplinary integrated management of these patients.
TRANSDISCIPLINARY MANAGEMENT OF PATIENTS WITH FEMUR PROXIMAL EXTREMITY FRACTURE
A transdisciplinary management of FFPE patients started from a model of a “fracture liaison service” that might reduce the osteoporosis treatment gap, improving functional outcomes in these patients[28-30].Figure 1 describes a model of a transdisciplinary management of patients with FFPE.
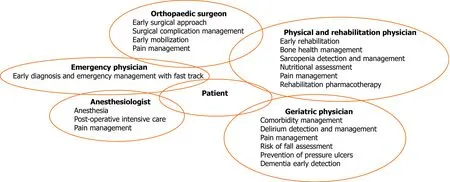
Figure 1 Model of a transdisciplinary management of patients with femur proximal extremity fracture.
Linet al[31] recently performed a meta-analysis assessing the effects of comprehensive geriatric care.They reported a consistent decrease of overall mortality (OR: 0.71; 95%CI: 0.53-0.95), whereas independence in activities of daily living significantly improved (standardized mean difference: 0.29; 95%CI: 0.12-0.47).Despite reports that hospital-based transdisciplinary rehabilitation could be more expensive than usual care, the sanitary costs may be offset by the benefits in terms of reduced length of stay and independence at discharge[32].
Furthermore, interdisciplinary management might play a key role also in the screening for common co-occurring conditions, such as delirium or pain[33].In particular, delirium is very common after hip fractures, with a prevalence between 13.5% to 33.0%[34] and was shown to negatively affect clinical and functional outcomes[35,36].Unfortunately, the clinical manifestations are heterogeneous, ranging from a hyperactive delirium, characterized by irritability, pressured speech and uneasiness to a hypoactive delirium, characterized by quiet mobility reduction, special-temporal disorientation, carelessness and trouble to answer simple questions[37].A transdisciplinary screening for delirium should be provided across the FFPE management to avoid detrimental consequences on functional outcomes, complications and even mortality[10].Unfortunately, routine assessment remains uncommon with approximately 39% of hip fracture patients suffering from delirium at discharge and 32% at 1 mo after fracture[36].
Taking into account that pain is a major risk factor for delirium, adequate management is mandatory to reduce delirium onset[10,38].NICE guidelines[17] recommend analgesia administration within the first 30 min from hospital admission.Paracetamol should be considered as first-line in the management of the elderly with FFPE.However, frequent analgesia targets were not reached by paracetamol administration only.Therefore, oral opioids should be considered even if intravenous opioids provide faster relief[39].Recently, peripheral nerve blocks have been introduced in managing pain and minimizing the side effects and sedation related to opioid drugs[40,41].In addition, continuous blocks can be included after surgical intervention for postoperative analgesia, with potentially positive effects in terms of pain, confusional state and probably in time to the first mobilization[42].
In this context, an early rehabilitation might reduce pain in FFPE patients and should be adequately planned particularly in elderly patients.
REHABILITATION AND MANAGEMENT OF OSTEOSARCOPENIA
Rehabilitation is recommended by the main Osteoporosis Guidelines available in the literature in patients with osteoporotic FFPE[43].The main goals of the rehabilitation management are reducing pain, improving physical function, independence in activities of daily living and health-related quality of life[44].Oldmeadowet al[45] reported potential benefits of walking 24 h or 48 h from surgery compared to delayed assisted ambulation after 3 d or 4 d from surgery.Moreover, a higher rate of discharge to home (26.3%) was recorded compared to the delayed ambulation group (2.4%).In a single-blinded cohort study, Overgaardet al[46] assessed progressive strength training shortly (17.5 ± 5.7 d) after FFPE surgery in outpatients, with positive effects in terms of pain and functional outcome measurements.
In this context, rehabilitation plays a key role in the comprehensive management of FFPE patients, taking into account the positive effects of exercise in the recovery of functional status[47] and for balance and prevention of risk of falling, which is a major determinant of refracture occurrence[48].
During the transdisciplinary management of FFPE patients, caregivers should be included across the whole pathway[49,50].As a matter of fact, functional impairment resulting from FFPE in elderly patients require long-term care in different settings.Albeit the transition from hospital to home should be conducted by health professionals[51], in outpatient settings, caregivers should be informed and trained with health education programs in order to optimize patient management at home[52-54].
In this scenario, long-term management of FFPE patients should include osteoporosis and sarcopenia screening[17].In light of this consideration, dual-energy x-ray absorptiometry should be performed to provide data of the baseline condition and treatment monitoring, whereas bone densitometry exams are not mandatory to start anabolic/antiresorptive treatment.However, promising studies showed that ultrasound assessment might be used for osteoporosis diagnosis[55,56].
Despite bone health playing a key role in patients suffering from FFPE, the optimal management of patients with fragility fractures is still evolving, with new pharmacological therapeutic strategies including sequential therapies aimed at optimizing bone formation or inhibit bone resorption[57].
Bisphosphonates are still the osteoporosis drug most commonly prescribed, characterized by antiresorptive action induced by osteoclast function inhibition[57,58].However, denosumab, a fully human IgG2 monoclonal antibody preventing the development of osteoclasts by RANK inhibition, has been introduced as effective therapy for osteoporosis in the last decade[58,59].In contrast, an anabolic drug such as teriparatide might stimulate bone formation and could be used in FFPE patients for a limited period of time (anabolic window)[60].
Several exercise modalities have been proposed as nonpharmacological treatments to prevent bone loss, increase bone mineral density and reduce fall risk[61].In particular, balance training, weight-bearing, strength training, progressive resistance exercise and Tai Chi seem to be effective in both osteoporosis prevention and treatment.Moreover, these exercise trainings were encouraged by national and international recommendations[62].Exercise therapy should be tailored to patients’ characteristics, focusing on back extensors and hip muscles due to the widely noted osteogenic effects of physical exercise and the improvement in terms of balance control[63,64].
Moreover, besides osteoporosis management, physicians should focus on sarcopenia, taking into account the strict relation among muscle strength, function impairment and risk of fall.More in detail, sarcopenia is considered a multifactorial common condition sharing several pathophysiological mechanisms with osteoporotic hip fracture patients[47].
A recent meta-analysis including more than 10000 older patients reported that sarcopenic patients have a higher risk of falls compared to non-sarcopenic ones (pooled OR: 1.52, 95%CI: 1.32-1.77,I2= 39.1%)[65].However, risk of fall is not the only mechanism linking sarcopenia and FFPE.Indeed, sarcopenia and osteoporosis share several underlying pathogenic factors, including cellular biomolecular pathways involving muscle-derived cytokines (myokines) influencing bone density, growth and repair[66].
Moreover, albeit aging is the most common risk factor for sarcopenia, malnutrition has been widely recognised to be strictly related to sarcopenia onset.In this context, previous studies reported a malnutrition prevalence in hip fracture patients ranging from 40% to 80% of hospitalized patients[67,68].Furthermore, it has been reported that malnutrition may be considered a risk factor for FFPE, and it is a strong predictor of poor functional recovery[10,67].In this scenario, oral nutrition supplementation has been proposed to reduce minor postoperative complications after FFPE, with promising results even in overall length of stay[69-71].Nevertheless, a recent systematic review reported several methodological flaws on trials supporting oral supplementation, underlining that nutritional interventions were supported by only weak evidence[69].In addition, nutrient supplementation without exercise seems ineffective in muscle strength improvement or physical frailty[72,73].
On the other hand, it has been reported that micronutrients might play a key role in the musculoskeletal system, promoting muscle anabolism and functioning in older people[74,75].Therefore, combined nutrition and physical exercise might be crucial to treat complex and multifactorial conditions affecting the musculoskeletal system, including sarcopenia in hip fracture patients[76,77].
Taking into account these findings, our group has recently performed a pilot randomized controlled trial[47] to assess the effects of a transdisciplinary rehabilitative and nutritional approach, showing promising results in terms of strength and physical function in sarcopenic hip fracture patients.Moreover, a further analysis in a subgroup of this population suggested that serum myostatin levels might be considered as promising biomarkers of sarcopenia in hip fracture patients undergoing rehabilitation after orthopaedic surgery[78].
In this scenario, the “rehabilitation pharmacotherapy” has been recently introduced to characterize medical management based on optimization of functional outcomes and minimization of adverse effects on nutritional status[79].
Thus, these findings suggested that a comprehensive long-term patient-tailored rehabilitative approach should be planned for the elderly with FFPE to optimize physical exercise, nutritional intake, bone health and medical drugs to promote complete functional recovery of frail patients.
However, despite the large amount of literature supporting a transdisciplinary approach in the elderly suffering from FFPE, the feasibility in most hospital settings still remains difficult.We retain that this approach might optimize the integration among hospital care management, rehabilitative outcomes and ensure continuity of care at discharge[80,81].
DEMENTIA IN HIP FRACTURE PATIENTS
Dementia is a cognitive disorder characterized by intellectual function impairment affecting both function and social performance[82,83].Recent studies[84,85] reported that approximately 19% of patients with FFPE meet diagnostic criteria for dementia.In addition, considering that age represents one of the most common risk factors for dementia, the number of hip fracture patients with dementia is expected to increase worldwide.To date, previous evidence showed that FFPE older patients with dementia were admitted to long-term care more frequently, and the mortality rate was significantly higher in these patients[86].In this scenario, targeted interventions are needed to optimize a multidisciplinary management of hip fracture patients with dementia.In particular, structured and familiarised routines, orientation to environment and cues were proposed to enhance care pathway and their rehabilitation plan[87].
Despite physical and cognitive rehabilitation were considered as effective therapies to improve functional and performance outcomes in elderly, a gap in the current literature in terms of effectiveness in patients with dementia has been shown[88].Similarly, a recent Cochrane systematic review[89] reported very low-quality evidence supporting geriatrician-led recovery and enhanced rehabilitation strategies in the functional recovery of elderly patients with dementia after FFPE surgery.
Therefore, the optimization of rehabilitative pathways in these particular patients might be considered a challenge.However, multidisciplinary management should be tailored to the patients in order to overpass cognitive impairment limitations to optimize functional outcomes of patients with dementia.Unfortunately, albeit the optimal rehabilitation and care model is still uncertain, an early detention in addition to dementia-focused treatment might be considered in the future, taking into account the potential role of assistive technologies and caregivers in the recovery pathway of these patients.
Furthermore, in light of these considerations, fragility fracture prevention should be emphasized to improve long-term management of patients with dementia.In contrast, it has been reported that dementia could be strictly linked to osteoporosis[90].However, bone health management could be frequently underestimated in the elderly with cognitive impairment due to the short life expectancy of these patients[91].On the other hand, a growing number of papers underlined poor compliance with osteoporosis drugs, especially in patients with dementia or elderly with polypharmacotherapy[92].
Therefore, given the high sanitary burden and the social consequences of fragility fracture recurrence, osteoporosis management should be emphasized considering subcutaneous denosumab or annual zoledronic acid infusions characterized by a lower discontinuation rate and earlier onset of efficacy in fracture reduction[93], with possible implications in long-term outcomes of patients after fragility fractures with dementia.
STUDY LIMITATIONS
Albeit the aim of the present article was to underline the key role of transdisciplinary management of patients with FFPE, some limitations should be taken into account before drawing conclusions.
First, in the clinical scenario, FFPEs are composed by a wide variability of anatomic presentations including head fractures, femur neck fractures, intertrochanteric fractures, subtrochanteric fractures and proximal femur shaft fractures.In the era of precision medicine, we are aware that a specific stratification should be provided to clearly present data of FFPE, given the strict linking among anatomic presentation, surgical intervention, bone health and rehabilitation.Unfortunately, the present editorial did not distinguish FFPEs; however, this intrinsic limitation reflects the high number of studies in the literature considering FFPE as a single pathology, resulting in a wrong generalization of study results probably affected by the type of fracture, with crucial implication in terms of evidence supporting a patient-tailored therapeutic plan.
Furthermore, it should be noticed that the high heterogeneity of key topics discussed in the present study did not allow a systematic review to be performed.In light of these considerations, a narrative analytical technique has been performed to highlight the gaps in the current literature and to guide future research and clinicians in a tailored transdisciplinary management of FFPE.
CONCLUSIONS
Taken together, the optimization of FFPE patient management should be considered as crucial to avoid the detrimental consequences on functional outcomes and the assistance and healthcare burden related to fragility fractures.Albeit the current literature supports a transdisciplinary care of elderly patients suffering from FFPE, global challenges still exist to implement these findings in the common clinical practice.The main limitation in terms of generalization of organization models might be found in the large heterogeneity of settings, healthcare models, community opportunities and specializations involved in the complex management of these patients.It would be optimal to be able to organize the care of these patients in multidisciplinary hospital wards of orthogeriatrics.However, this editorial was meant to describe the need to define a tailored transdisciplinary management that could be performed in the common clinical practice to reduce functional and social consequences of patients with FFPE.Further studies are warranted to define feasible organization models supported by clear evidence to manage FFPE patients across the whole health care pathway, in both inpatient and outpatient settings.
 World Journal of Orthopedics2021年7期
World Journal of Orthopedics2021年7期
- World Journal of Orthopedics的其它文章
- Arthrodesis of the first metatarsophalangeal joint: The “when and how”
- Arthroscopic removal as an effective treatment option for intraarticular osteoid osteoma of the knee
- Strategies and outcomes in severe open tibial shaft fractures at a major trauma center: A large retrospective case-series
- Technological advancements in the analysis of human motion and posture management through digital devices
