A unitary caring science resilience-building model:Unifying the human caring theory and research-informed psychology and neuroscience evidence
Holly Wei ,Sonya Renae Hardin ,Jean Watson
a College of Nursing at East Carolina University,Greenville,NC,USA
b University of Louisville School of Nursing,Louisville,KY,USA
c Watson Caring Science Institute,Distinguished Professor/Dean Emerita University of Colorado Denver College of Nursing,CO,USA
Keywords:Health personnel Professional burnout Psychological resilience Resilience-building strategies Watson’s unitary caring science
ABSTRACT Resilience is the psychological capability to recover from difficulties quickly.Healthcare professionals are especially vulnerable to job-related stress and burnout.Unitary Caring Science is the framework for Watson’s Human Caring Theory,providing a philosophy of practice in healthcare.With the high rates of clinician burnout and psychological issues,it will be significant to unify the human caring theory with research-informed psychological and neuroscience evidence to develop clinicians’ resilience-building strategies.The purpose of this article is to introduce a Unitary Caring Science Resilience Model and explain the science behind the core strategies based on Unitary Caring Science philosophy and the psychological and neuroscience research.This model includes six strategies:Embracing loving-kindness for self and others; Nurturing interpersonal and intersubjective connections/relations; Deepening a creative use of self and sense of belonging; Balancing self-learning,self-awareness,and an evolved selfconsciousness; Valuing forgiveness and releasing negativity; Inspiring and maintaining faith-hope.The caring-theory guided resilience-building strategies are proven to alleviate the depletion of clinicians’energy and emotions.Healthcare practices are challenging but rewarding.Clinicians can be emotionally,psychologically,and physically exhausted if they always consider themselves ‘giving’ and ‘doing’ institutional tasks without a sense of purpose or fulfillment.The practice can be rewarding if it becomes more aligned with clinicians’value to serve humanity.Through the unitary caring science resilience strategies,clinicians can build resilience as an antidote to clinician burnout and depletion.
What is known?
·Clinicians face tremendous mental and moral distress at work,and clinician job-related burnout is an epidemic.
·Clinicians' resilience and well-being impact patient quality and safety.
·Stress is unavoidable in life,and it is essential to learn healthy ways to cope with adversities and recover from devastations more quickly.
What is new?
·A Unitary Caring Science Resilience Model was developed based on Unitary Caring Science philosophy and research-informed psychological and neuroscience evidence.
·The model comprises six resilience-building strategies,including Embracing loving-kindness for self and others;Nurturing interpersonal and intersubjective connections/relations;Deepening a creative use of self and sense of belonging;Balancing self-learning,self-awareness,and an evolved selfconsciousness; Valuing forgiveness and releasing negativity;Inspiring and maintaining faith-hope.
1.Introduction
Resilience refers to the capability to adjust and adapt to adversity,spring back,and move forward without stress-induced psychological issues,such as depression,anxiety,or posttraumatic stress disorder [1].The notion that resilience is a resistant factor to stress initiated in the 1970s,studying children’s ability to develop normally despite a difficult childhood.Since the 1990s,the focus of resilience research has moved to identifying positive protective factors to help individuals overcome difficulties [2,3].Healthcare professionals are vulnerable to job-related stress and burnout because of job characteristics[4,5].Healthcare practice is filled with uncertainties and stressors,and clinicians,including nurses and physicians,routinely face unpredictable and traumatic events.With the increasing rates of clinician burnout and psychological issues,it will be a significant contribution if we can unify a human caring theory with research-informed psychological and neuroscience evidence to help clinicians develop resilience.Unitary Caring Science is the framework for Watson’s Human Caring Theory [6],providing a philosophy of practice in healthcare.Thus,the purpose of this article is to introduce a unitary caring science resilience model and explain the science behind the core strategies based on Unitary Caring Science philosophy and the psychological and neuroscience research.
2.Background
Stressful situations,traumatic events,and life-altering illnesses are unavoidable in life.Individuals need to have the ability to meet the challenges and recover from the adversities.It is believed that a lack of resilience can lead to psychological issues,including fear,anxiety,depression,and emotional disorders [2,3].Current resilience research indicates two major pathways to fostering a resilient brain:behavioral pathways and cognitive pathways [3].The behavioral pathways refer to using learnable behaviors and habits to change the brain,and the cognitive pathways is applying learnable cognitive/linguistic strategies to boost resilience.Behavioral pathways include strategies that can directly reduce the responses of fear and stress,boost physical health,and seek social connection and support[3].Cognitive pathways focus on strategies that can promote emotion regulation and cognitive training [3].
Clinician burnout is an epidemic,a phenomenon faced by many countries in the world [7,8].Nurses and physicians are among the most at risk for job-related stress or burnout [4,5].Burnout has three dimensions -exhaustion (negative physical and emotional manifestations with stressors),depersonalization (detached from one’s job),and inefficiencies (dissatisfaction with one’s performance) [9].When nurses and physicians are burnout,they feel exhausted physically and mentally,exhibit a ‘do not care’ attitude,and have feelings of inefficiency toward one’s job performance or achievement [9].Nurses and physicians who report burnout are more worried about making errors and have lower confidence and ratings of patient care quality [10].
Most clinicians choosing to work in healthcare have a passion for caring and helping others.However,the professional training often focuses more on the clinical aspect of the profession,considered as the‘hard science,’such as disease management,and less on the art of the profession,thought of as the ‘soft science,’including caring,compassion,and resilience-building [11].This pattern of education may place clinicians in a vulnerable position,not knowing how to be more resilient.Clinicians’ well-being is critical in promoting healthcare quality,and it is essential to help clinicians adopt healthy strategies to build resilience and overcome difficulties.
3.Methods
This is a discussion paper that introduces an evidence-informed resilience-building model for clinicians,including nurses and physicians.This model was developed based on Unitary Caring Science philosophy,Watson Human Caring Theory,and researchinformed nursing,psychological,and neuroscience resilience literature.Unitary Caring Science is the framework for Human Caring Theory [6],providing a philosophy for healthcare practice[6,12].The Human Caring Theory includes ten Caritas Processes?:Embrace,Inspire,Trust,Nurture,Forgive,Deepen,Balance,Co-Create,Minister,and Open [6].The ten Caritas Processes? were the underpinning of the core strategies of the resilience-building model.
The literature search was conducted using the following databases of a university library website:Medline via PubMed,Cumulative Index to Nursing and Allied Health Literature (CINAHL),PsycINFO,and Google Scholar.The search aimed to find psychological and neuroscience studies that examined the effects of resilience strategies on brain structures and activities.Review articles summarizing practical resilience approaches were also included.
4.Results regarding the strategies to build resilience
The model comprises six resilience-building strategies based on the ten Caritas-Veritas Literacy of Unitary Caring Science and research-informed evidence.The six strategies include 1)Embracing loving-kindness for self and others (Embrace); 2)Nurturing interpersonal and intersubjective connections/relations(Trust and Nurture);3)Deepening a creative use of self and sense of belonging (Deepen and Minister); 4) Balancing self-learning,selfawareness,and an evolved self-consciousness (Balance and Co-Create); 5) Valuing forgiveness and releasing negativity (Forgive);6) Inspiring and maintaining faith-hope (Open and Inspire).(Fig.1)
Healthcare practices are challenging but rewarding.It is emotionally,psychologically,and physically exhausting if clinicians consider their job as always ‘giving’ and ‘doing’ institutional tasks without a sense of purpose or fulfillment.However,with a renewed consciousness of meaning,vision,and purpose,there can be a renewal of life-force energy.Healthcare practice can be rewarding when clinicians align practice with purpose,cherish each caring moment,and value their gift of service to humanity.Through unitary caring science resilience-building strategies,clinicians can gain a sense of belonging and awareness of meaning and purpose.Therefore,clinicians are more capable of engaging in compassionate self-caring,informed by both theory and science as an antidote to clinician burnout and depletion.
4.1.Embracing loving-kindness for self and others
Embracing loving-kindness for self and others is one of the most fundamental Caritas of Watson’s Human Caring Theory.Lovingkindness is the essence of our relationships with ourselves and others [13].Kindness is transmissible; a kind act can lift the mood of the ones performing it and those receiving it.We all belong to the universe,in which we embrace the universal field of love[14].We can live and grow in this world because of the love surrounding us,nurturing us and making our lives meaningful.
Research shows that acts of kindness can have a positive effect on the brain and the neuroendocrine system,releasing ‘happy’hormones like oxytocin,dopamine,and serotonin.Oxytocin,also known as a ‘love hormone,’ can boost our trust and bonding with others,promote social functions,and increase our self-esteem and optimism [15].Oxytocin can also decrease inflammation,relax blood vessels,improve cardiac functions,stimulate angiogenesis,and promote healing[16].Dopamine can lift our mood and results in a‘helper’s high.’Serotonin can regulate our emotions and give us a euphoria feeling; lower serotonin levels are linked to poor memory and depression[17,18].Loving-kindness acts make people feel happier and more satisfied [19-21],making love-kindness a critical resilience factor.
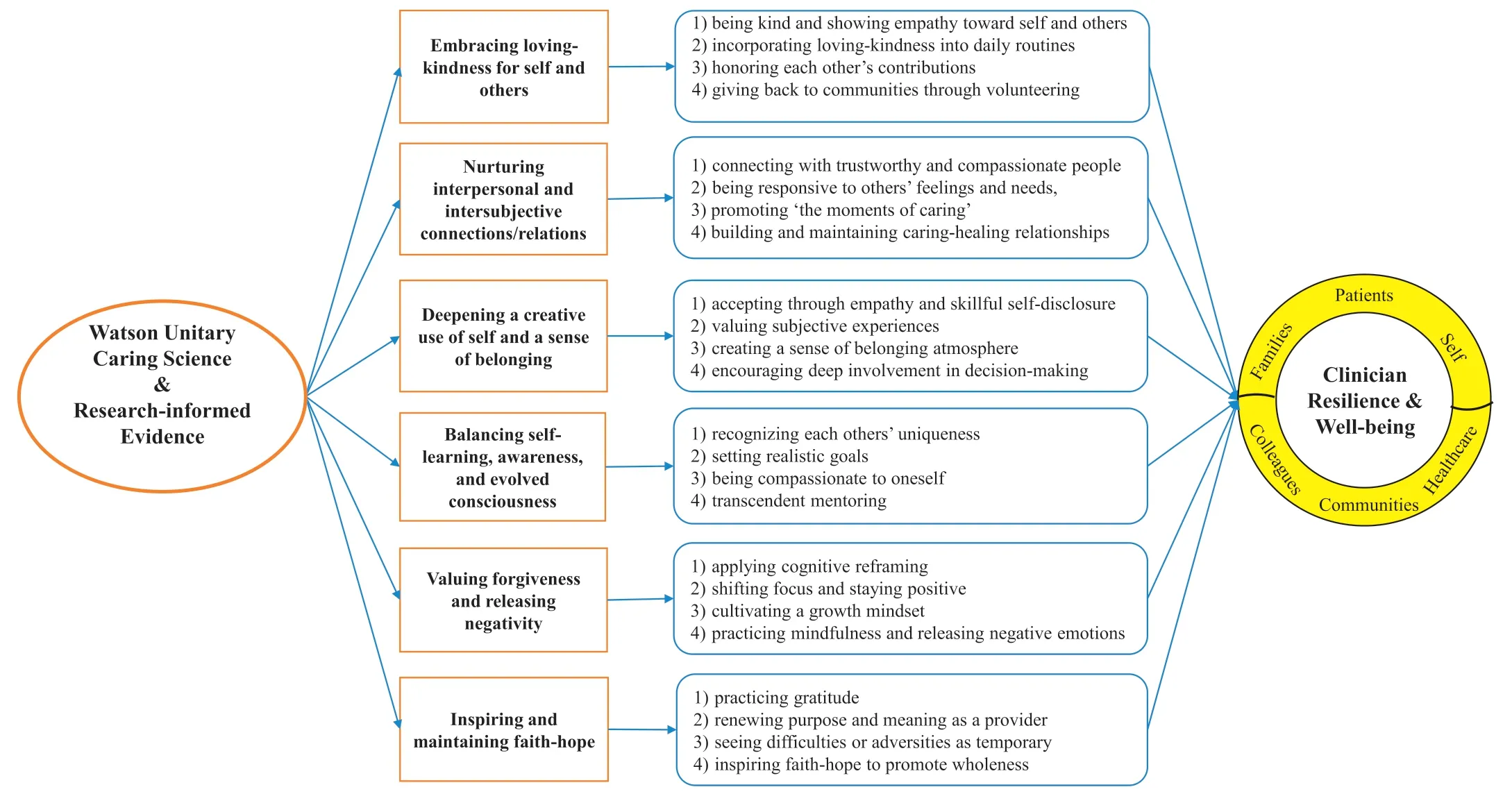
Fig.1.Unitary caring science resilience-building model.
Clinicians are in a prime position to care for others with lovingkindness.Nurses and physicians can build resilience through loving-kindness by 1)being kind and compassionate to oneself and others; 2) incorporating loving-kindness into their daily routines,such as “Random Acts of Kindness” and “Paying it Forward; ” 3)honoring one another’s contributions to patient care;4)giving back to communities through volunteering; 5) self-caring by having moderate exercise,balanced nutritional diet,and adequate sleep.When performing loving-kindness to ourselves and others,we become psychologically stronger.
4.2.Nurturing interpersonal and intersubjective connections/relations
Interpersonal connections are relationships between individuals.Intersubjective connections and relations are the connecting moments between two subjective minds,also called ‘the moments of connection’ or ‘the moments of caring’ based on Watson’s Human Caring Theory [6].A ‘moment of caring’ is both intersubjective and transformative.As clinicians,we bring many internal states to our relationships with patients,whose subjectivity also swirls around us,looking for patterns to relate.When the two subjective minds connect,the relations between them transform,during which clinicians understand patients’ subjective experiences.The quality of the relationships with others directly affects one’s emotions.Having trusting relationships helps individuals cope with stressful situations and is one of the most critical aspects of promoting resilience and overcoming adversities.Trust emerges through believing in and having the courage to be honest with another.
Research indicates that social support and connections can affect individuals’ physical and mental health through regulating the hypothalamic-pituitary-adrenocortical (HPA) axis and central oxytocin pathways.The regulation of the HPA axis stress response and central oxytocin pathways can help boost the immune system,promote resistance to illness,recover from disease quicker,and increase the lifespan [16,22,23].Individuals with higher levels of social support and connections have an increased sense of companionship [24].Those with more social support and connections are mentally and physically healthier,and lack of social connections is more harmful to health than conditions like obesity,smoking,and high blood pressure [22].Interpersonal and intersubjective connections are crucial in promoting physical and psychological well-being.
Clinicians can promote interpersonal and intersubjective connections by 1) connecting with others who are trustworthy and compassionate; 2) being more responsive to self and others’ feelings and needs; 3) authentically listening to others about their experiences and concerns;4)creating opportunities to connect and nurturing trusting-caring relationships with colleagues at work and outside of work; 5) promoting ‘the moments of caring’ at the intersubjective level,and 5) building a caring-healing work environment.
4.3.Deepening a creative use of self and sense of belonging
A sense of belonging is a subjective experience that is associated with the longing of acceptance.Biologically,based on Maslow’s Hierarchy of Needs,a sense of belonging is considered a fundamental human need,like food and shelter,and comes before our esteem and self-actualization [25].Ethically,according to Levinas’Philosophy of the Other,the sense of belonging is the first principle of science and human relations [26].This philosophy is also the ontology of Watson’s Unitary Caring Science and the nursing discipline[6,27].The creative use of self is the combination of one’s knowledge,values,and skills learned in nursing and medical education with one’s personal self,including personal beliefs and experiences.Clinicians’ creative use of self helps them strive to contribute with authenticity and genuineness through empathy and skillful self-disclosure,communicating and revealing oneself skillfully.
Belonging is one of the biology traits.Since birth,our brains continually crave belonging and feel at ease when we feel safe and belonging.Endocrinological research shows that when we feel connected,socially included,and bonded,our bodies secret oxytocin,helping us feel safe and loved [28].Social rejection or ostracism can cause tremendous social pain,which is similar to the reactions to physical pain [29].People having a strong sense of belonging to a social group are happier and more satisfied with their health status [30].A report indicates that being employed increases individuals’sense of belonging and is beneficial for their mental state [31].The benefits of having a job are beyond the monetary aspects but correlated with one’s feelings of social status and life purpose,which is a critical resilient factor.
The increased sense of belonging can improve clinicians’ satisfaction and happiness at work.Clinicians can promote a sense of belonging and the creative use of self by 1) accepting one another through empathy and skillful self-disclosure; 2) valuing subjective experiences to achieve transformative relations;3)creating a sense of belonging atmosphere; 4) promoting clinicians’ sense of belonging through professional development at a system level; 5)encouraging clinicians’ deep involvement in decision-making to develop an ownership mentality.
4.4.Balancing self-learning,self-awareness,and an evolved consciousness
Self-learning is a process through which individuals identify their learning needs,develop learning goals,locate learning resources,and assess learning outcomes.The self-learning process helps individuals gain self-awareness and evolved self-consciousness.Self-consciousness is a deepened sense of self-awareness,a conscious exploration of one’s thoughts,values,beliefs,and behaviors[32,33].Self-awareness is the conscious knowledge about one’s own thoughts,behaviors,feelings,and desires.Balancing is a process of knowing oneself as a whole and making decisions to balance needs and desires.Being aware of one’s beliefs and values can help develop an inner power,empowerment from within.Balancing self-learning and an evolved consciousness is a vital resilient factor.It helps us recognize our strengths and limitations,balance our life and work demands,and be better prepared to face challenges and stress.Balance is about moderation,where over-doing,-thinking,or-working may result in an imbalance and increase the risk of patient safety.
Chronic stress can lead to a series of negative effects on individuals.Through a neuroscience lens,chronic stress can activate the body’s HPA axis and a series of stress responses [23,34].For instance,the perceptions of stress stimulate glucocorticoid receptors in the hippocampus that activates the hypothalamus,which secretes the corticotropin-releasing hormone (CRH).The CRH will then activate the pituitary gland to release adrenocorticotropic hormone (ACTH),which leads the adrenal glands to secrete cortisol,a‘stress hormone.’The chronic elevation of cortisol can increase conditions like blood sugar,blood pressure,protein catabolism,and insomnia,and suppress immune cells and gastrointestinal functions.The prolonged elevation of cortisol may increase inflammation and result in diabetes and hypothyroidism;the extended stimulation of the HPA axis can affect the functions of the hippocampus (cognition,learning,and memory) and the amygdala,the ‘fight or flight’ center,affecting the critical thinking capability [28].These stress responses indicate the criticality of balancing our thoughts,feelings,and behaviors.
Healthcare clinicians can promote the balance of self-learning,self-awareness,and an evolved self-consciousness through 1)recognizing each of us as a unique human being,appreciating one another’s strengths and limitations; 2) setting realistic goals that we can achieve with certain efforts,not out of our reach; 3) being compassionate to oneself by performing self-learning and selfawareness; 4) finding opportunities to relax and soothe the mind and body with some simple exercises,such as practicing mindfulness and connecting with nature; 5) transcendent mentoring:applying transpersonal teaching and spreading positivity; 6)authentically listening to others’ life stories to understand others’perspectives.
4.5.Valuing forgiveness and releasing negativity
Forgiveness is a person’s conscious and deliberate decision to let go of the resentment.Forgiving,letting go of the past,helps us focus on the current moments,show empathy toward the person or events that hurt us,and release our negativity.Forgiving is not pretending that the hurtful behaviors did not occur but rather opening a venue to empty our resentments and release our negative thoughts and feelings.Working on forgiveness is a process that can increase our self-esteem,change our inner positively,and help us regain happiness,a vital ingredient of being happy,healthy,and resilient.
Research that examined brain structures underlying forgiving responses showed that higher tendency to forgive scores were positively correlated with the gray matter volume in the dorsolateral prefrontal cortex,a brain area that plays a significant role in envisioning others’feelings and showing empathy;the tendency to forgive was negatively related to the gray matter volume in the right insular cortex and inferior frontal gyrus,indicating being more forgiving [35,36].Studies on the effects of mindfulness practice indicated that focusing on the present moments could increase the hippocampus’ gray-matter density (a brain area important for learning and memory) and decrease it in the amygdala,the emotional center playing an important role in causing anxiety and stress [37].When we feel hurt emotionally,senses associated with a threat in the amygdala can trigger the fear response.If the stressors,such as anger,fear,anxiety,and stress,are constant,the brain can be soaked in elevated stress hormones,leading to negative feelings and harming the body,mind,and spirit.If these alterations persist,they can affect our whole-body system and be detrimental to our physical and psychological well-being[38].Forgiving can promote physical and psychological health,including better sleep quality and reduced pain,blood pressure,cholesterol,anxiety,depression,and stress [39,40].So,when we forgive,we get the benefits,which is key for being resilient and happy.
Healthcare clinicians are individuals working with people of all kinds,including patients,families,and interprofessional team members.There may be times that we feel hurt or offended,during which clinicians may try the following to mitigate their negative feelings:1) using cognitive reframing to help us look at the situations from a different perspective and foster a forgiving mentality.Reframing is vital to help clinicians change their negative feelings about their work,shifting from ‘serving’ patients as institutional tasks to caring for patients as sacred acts; 2) applying expressive writing to deeply express and reflect on the things that bother us and release our anger,thoughts,and feelings; 3)shifting focus is a way in which clinicians can focus on the positive instead of the negative aspects of situations and stay positive; 4) cultivating a growth mindset to adapt and adjust to the ever-changing world;5)performing mindfulness practice to focus on the present moment,being aware of the senses and feelings in the current moment without judgment and releasing negative emotions.Mindfulness practice does not need to take a long time.When clinicians have a few minutes of spare time,they can practice mindfulness handwashing (paying attention to the handwashing movements) and mindfulness breathing (focusing on the slow movement of inhalation and exhalation).
4.6.Inspiring and maintaining faith-hope
Inspiring faith-hope is our capacity to maintain beliefs and get through adversities.Having faith-hope is a significant motivator for individuals to strive for physical and mental health and well-being[8].We all go through crises,difficult times,and trials in life; it is what we do and how we choose to deal with those situations that make a difference in outcomes.Maintaining faith-hope is the underpinning for us to stand up and stay positive when facing adversities,a crucial resilience strategy to cultivate.
Neuroscience research shows that practicing positive and grateful acts can increase the gray matter volume in our hippocampus and neocortex,the areas responsible for our memory and critical thinking [41].People who have a gratitude attitude,stay positive,and have a purpose in life are happier and healthier than their counterparts; even just by appreciating what we have in our lives can help us feel more optimistic and positive [41,42].Other studies suggest that a high level of gratitude can have a significantly positive influence on individuals’physical and psychological health,promoting their self-esteem and decreasing depression [43,44].People with a purpose feel more hopeful in life [45,46]and more fulfilled in work[47].Maintaining hope and gratitude is a protective factor when facing adversities [48,49].A strong sense of purpose can be like an inner compass,guiding us to re-find passion or vision and maintain faith-hope.
Clinicians are often faced with tragedies and crises related to human suffering.Clinicians can inspire and maintain faith-hope by 1)practicing gratitude;2)honoring the inner-subjective life world and power of ourselves and others; 3) being open to the possibilities of spiritualism and unknowns and allowing for miracles; 4)refocusing one’s purpose and meaning of being a healthcare provider; 5) seeing the difficulties or adversities as a temporary moment in time; 6) inspiring faith-hope to promote wholeness.
5.Discussion and implications to practice
This article introduced a resilience-building model that unified the philosophy of Unitary Caring Science and research-informed psychological and neuroscience evidence.The importance of clinicians’well-being has been elevated to one of the top priorities to ensure patient safety and care quality [4].The resilience-building model suggests six strategies to foster clinicians’ resilience:Embracing loving-kindness for self and others; Nurturing interpersonal and intersubjective connections/relations; Deepening a creative use of self and sense of belonging;Balancing self-learning,selfawareness,and an evolved self-consciousness; Valuing forgiveness and releasing negativity;Inspiring and maintaining faith-hope.
These strategies are essential ingredients to cultivate a resilient brain and can be readily incorporated into clinicians’daily routines to promote their resilience and well-being [50,51].Resilient clinicians strive to create a work environment that welcomes and cares for all involved and accepts and honors diversity [27,52].System leaders play a significant role in creating a practice culture whereby clinicians have a sense of belonging.They can promote it by helping clinicians grow professionally,creating a culture of caring and trust among staff and teams,offering them opportunities to be engaged at work and develop an ownership mentality.
Within a Unitary Caring Science context,nurses and physicians understand the healing power of faith-hope and the importance of inspiring faith-hope in themselves and others.Healthcare professionals are expected to provide loving and compassionate care to patients while facing uncertainty and stress [12,53].These resilience-building strategies are proven to alleviate nurses’ and physicians’ emotional stress through bio-social-psychological processes.Authentic caring relationships are essential to healthcare professions.The authentic caring relationships in healthcare can promote clinicians’ physical,psychological,emotional,and social well-being and enhance healing [53].
Healthcare service is a challenging but rewarding career,depending on clinicians’ mindset.Reframing and shifting our mindset can help us look at situations from a different perspective[52,54].An example is caring for patients’basic needs,which could be physically and mentally draining if clinicians only consider it as tasks to complete without a purpose or fulfillment.However,if they shift their mindset and consider it as patients’ trust in the professions and as sacred acts,they can discover its meaning and value,making them feel fulfilled instead of depleted.Another way to help clinicians avoid feeling depleted is acknowledging one’s limitations.We know that our mission is to save lives,but we need to accept that we may not be able to save all the lives at times and balance our desires and capabilities[45].When we learn to balance what we can and cannot,we may mitigate our feelings of being depleted and insufficiency,which are signs of burnout.Resiliencebuilding strategies,informed by both theory and science,can be an antidote to mitigate clinician burnout and improve healthcare quality.
6.Conclusions
This article underscores a connection between clinicians’caring actions and resilience building.These resilience-building strategies have biological scientific underpinnings and are integrated and informed by philosophy and ten Caritas processes? of Unitary Caring Science.The underpinning of clinician resilience-building is a conscious-intentional mindset-shift,which is that when we give,we also receive,and that energy flow is communal.If clinicians can shift their mentality from giving to giving/receiving,they may change from feeling depleted to feeling fulfilled.If clinicians are depleted,so will be human caring for patients/families/society.Through self-caring strategies,healthcare practices can serve as an antidote for burnout.This unitary caring science resilience-building model is one way forward to bridge the gap between theory,practice,and outcomes.
CRediT authorship contribution statement
Holly Wei:Conceptualization,Methodology,Validation,Formal analysis,Resources,Data curation,Writing-original draft,Writingreview & editing.Sonya Renae Hardin:Conceptualization,Methodology,Validation,Writing -review & editing.Jean Watson:Conceptualization,Methodology,Validation,Writing -review &editing.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2020.11.003.
 International Journal of Nursing Sciences2021年1期
International Journal of Nursing Sciences2021年1期
- International Journal of Nursing Sciences的其它文章
- Focuses and trends of the studies on pediatric palliative care:A bibliometric analysis from 2004 to 2018
- Relationship between negative emotions and perceived support among parents of hospitalized,critically ill children
- The effect of digital health technologies on managing symptoms across pediatric cancer continuum:A systematic review
- Effectiveness of animal-assisted therapy on pain in children:A systematic review and meta-analysis
- Effects of creative expression program on the event-related potential and task reaction time of elderly with mild cognitive impairment
- Struggling to live a new normal life among Chinese women after losing an only child:A qualitative study
